Abstract
Abstract 2909
Poster Board II-885
Previous studies have identified sole abnormalities of del(20q) and del(13q) as prognostically favorable cytogenetic markers in primary myelofibrosis (PMF) (Tefferi et al. BJH 2001;113:763). A more recent study (Tam et al. Blood 2009;113:4171) confirmed these findings and suggested additional cytogenetic markers of prognosis. In the current study with larger numbers of informative patients studied at time of diagnosis, we wanted to validate these observations and examine the prognostic interaction between cytogenetic risk categorization and the International Prognostic Scoring System (IPSS).
Patients with cytogenetic information at diagnosis were selected from the Mayo Clinic database of WHO-defined PMF. Specific cytogenetic categories were considered only in the presence of at least 5 informative patients; otherwise, they were included in the category of “other cytogenetic abnormalities”. Follow-up information was updated in July, 2009. Survival curves were prepared by the Kaplan-Meier method and compared by the log-rank test. Cox regression model was used for multivariable analysis.
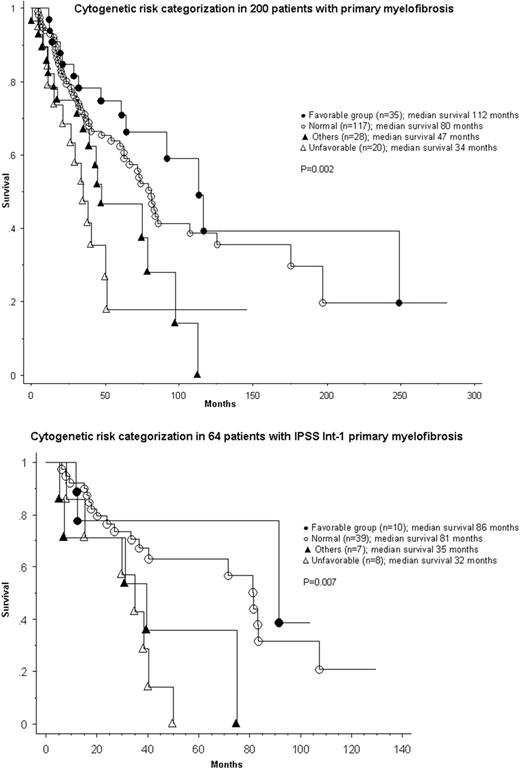
200 patients were studied (median age, 62 years; 63% males). The IPSS risk distributions were low in 66 patients, intermediate (int)-1 in 64, int-2 in 44 and high in 26. Cytogenetic findings at diagnosis were abnormal in 83 (42%) patients and included sole del(20q) in 21, complex (i.e. 3 or more abnormalities) in 13, sole del(13q) in 8, sole +8 in 7, sole +9 in 6, and other abnormalities in 28 patients. Median survivals in low, int-1, int-2 and high IPSS risk groups were 188, 71, 47 and 26 months, respectively (p < 0.0001). Median survival in patients with sole +9 was not reached and in those with sole del(13q), sole del(20q), normal karyotype, complex abnormalities and sole +8 was 112, 108, 80, 37 and 27 months, respectively, while it was 46 months for patients with other cytogenetic abnormalities (p = 0.01). Accordingly, sole abnormalities of +9, del(20q) and del(13q) were categorized as being favorable (n = 35) and complex abnormalities and sole +8 as unfavorable (n = 20); the respective median survivals were 112 and 34 months (p=0.002; Figure). Multivariable analysis confirmed the IPSS-independent prognostic value of cytogenetic risk categorization and the intra-IPSS risk prognostic distinction was most apparent in the int-1 group: median survival was 35 and 81 months in the presence of unfavorable or favorable cytogenetic markers, respectively (p=0.0009; Figure).
The current study identifies sole +9, along with del(13q) and del(20q), as favorable and sole +8, along with complex abnormalities, as unfavorable cytogenetic markers of prognosis in PMF. Cytogenetic risk categorization in PMF has an IPSS-independent prognostic value that is important in patient selection for specific therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal