Abstract
Abstract 2012
Poster Board I-1034
Cardiovascular magnetic resonance (CMR) is being increasingly used worldwide for monitoring chelation therapy in transfusion-dependent β-thalassemia patients. The assessment of cardiac iron loading using myocardial T2 star (T2*) is a reliable, quick and non-invasive method which can be combined with highly accurate and reproducible cardiac volume and function measurements. It has previously been noted that myocardial siderosis (T2*<20ms) is associated with progressive impairment in left ventricular (LV) function but little is known about the relation of T2* measurements to right ventricular (RV) function in these patients. This study assesses the impact of myocardial iron loading on the right ventricle.
A retrospective analysis was performed of 323 consecutive β-thalassemia patients referred for their first CMR scan from 21 UK hematology centers. Only patients on a single chelating agent (deferoxamine) were included. All had received chelation from the mid-to-late 1970s or from an early age if born since then. Patients were excluded if there was significant cardiac, vascular or lung pathology (such as aortic stenosis, pulmonary artery stenosis, tetralogy of Fallot or pulmonary hypertension). All scans were performed using a 1.5T Sonata (Siemens Medical Systems, Germany). A single breath-hold multi-echo sequence with 8 different echo times (TE = 2.54-17.9ms) was used to measure T2* from a full-thickness region of interest in the septum of a mid-ventricular short axis slice. Myocardial T2* was calculated from the exponential signal intensity decay curve using a truncation method to account for background noise. RV and LV volumes and ejection fraction (EF) were calculated from a series of short axis ventricular slices (7mm thickness with 3mm gap).
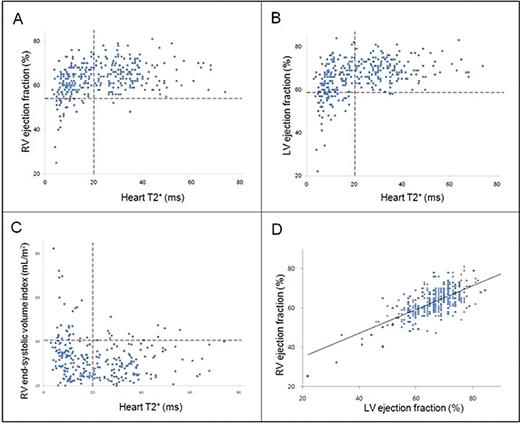
In patients with normal T2* (>20ms), RV EF was within normal limits in 98% of cases (RV EF [mean ±SD] = 65.0 ±6.1%). In patients with myocardial siderosis (T2*<20ms), there was a progressive and significant fall in RV EF (r=0.43, p<0.001) and an increase in RV end-systolic volume index (r= -0.33, p<0.001). LV EF was within the normal range in 99% of patients with T2*>20ms (LV EF = 69.5 ±5.2%). Once again, where T2* fell below 20ms, there was a progressive decline in LV EF (r=0.40, p<0.001). 82.6% of the patients with low T2* and impaired RV ejection fraction also had an impaired LV EF and linear regression analysis showed a significant relation between RV and LV EF (r=0.69, p<0.001).
There is a strong association between increasing myocardial iron loading and RV dysfunction which mirrors the decrease in LV ejection fraction seen with worsening myocardial siderosis. RV impairment may be a significant contributor to the syndrome of heart failure associated with severe myocardial siderosis.
RV ejection fraction (vertical axis) versus heart T2* (horizontal axis). B: LV ejection fraction (vertical axis) versus heart T2*. C: RV end-systolic volume index (vertical axis) versus heart T2*. D: RV versus LV EF (%). Horizontal dotted lines denote the lower limit of normal for RV and LV EF and the upper limit of normal for RV end-systolic volume index. Vertical dotted lines indicate lower limit of normal for heart T2* (20ms).
RV ejection fraction (vertical axis) versus heart T2* (horizontal axis). B: LV ejection fraction (vertical axis) versus heart T2*. C: RV end-systolic volume index (vertical axis) versus heart T2*. D: RV versus LV EF (%). Horizontal dotted lines denote the lower limit of normal for RV and LV EF and the upper limit of normal for RV end-systolic volume index. Vertical dotted lines indicate lower limit of normal for heart T2* (20ms).
Carpenter:Swedish Orphan: Honoraria; Apotex: Honoraria. Porter:Novartis: Consultancy, Research Funding. He:Novartis: Consultancy. Smith:Novartis: Consultancy. Pennell:Siemens: Consultancy; Novartis: Consultancy; Apotex: Honoraria; Cardiovascular Imaging Solutions, London: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal