Abstract
The viral infectivity factor (Vif) is essential for HIV-1 infectivity and hence is an ideal target for promising anti–HIV-1/AIDS gene therapy. We previously demonstrated that F12-Vif mutant inhibits HIV-1 replication in CD4+ T lymphocytes. Despite macrophage relevance to HIV-1 pathogenesis, most gene therapy studies do not investigate macrophages because of their natural resistance to genetic manipulation. Here, we confirm the F12-Vif antiviral activity also in macrophages differentiated in vitro from transduced CD34+ human stem cells (HSCs). Moreover, we identified the 126- to 170-amino-acid region in the C-terminal half of F12-Vif as responsible for its antiviral function. Indeed, Chim3 protein, containing this 45-amino-acid region embedded in a WT-Vif backbone, is as lethal as F12-Vif against HIV-1. Of major relevance, we demonstrated a dual mechanism of action for Chim3. First, Chim3 functions as a transdominant factor that preserves the antiviral function of the natural restriction factor APOBEC3G (hA3G). Second, Chim3 blocks the early HIV-1 retrotranscript accumulation and thereby HIV-1 DNA integration regardless of the presence of WT-Vif and hA3G. In conclusion, by impairing the early steps of HIV-1 life cycle, Chim3 conceivably endows engineered cells with survival advantage, which is required for the efficient immune reconstitution of patients living with HIV/AIDS.
Introduction
Anti–HIV-1 gene therapy is based on the concept that autologous hemopoietic stem cells (HSCs) carrying antiviral transgenes once reinfused into HIV-1+ subjects will naturally expand and differentiate into CD4+ T cells and macrophages, the 2 major HIV-1 cellular hosts. HIV-1–resistant CD4+ T cells and macrophages will then contribute to reconstitute the heavily compromised immune system of AIDS patients.1 It is manifest that an anti–HIV-1/AIDS gene therapy strategy should affect early step(s) of HIV-1 life cycle, such as viral entry and proviral DNA integration, to be most effective. This will reduce the generation of infected cells from noninfected cells.1,2
Viral infectivity factor (Vif) is an HIV-1 key protein because it counteracts the action of the cellular anti–HIV-1 restriction factor human APOBEC3G (hA3G) that, in the absence of Vif, has a deadly effect on HIV-1 replication.3 Vif is therefore an excellent target for the development of new anti–HIV-1/AIDS gene therapy approaches. In this context, we have previously reported that the natural F12-Vif mutant, containing 14 unique amino-acid substitutions,4 once delivered in CD4+ T lymphocytes by second-generation lentiviral vector (LV), efficiently prevents HIV-1 production.5 Recently, several Vif functional domains involved in either protein-protein or protein-viral RNA interactions have been identified.6-10 Of particular interest is the identification of a novel HCCH zinc-coordination motif conserved among primate lentivirus Vifs.11-13 This motif is critical for the interaction of Vif and Cullin5, which is one of the E3 ubiquitin ligase multiprotein complex deputed to hA3G degradation.14
Gene therapy preclinical studies, aimed at providing safety, feasibility, and efficacy analyses, mainly privilege the use of CD4+ T lymphocytes because these cells are easy to obtain, cultivate, and transduce by viral vectors, and are highly susceptible to HIV-1 infection in vitro. In contrast, primary macrophages are nonproliferating terminally differentiated cells, which are transduced by LVs at efficiency not higher than 30%.15-18 Hence, despite that macrophages are the major contributors of viral persistence and latency in vivo,19 anti–HIV-1 gene therapy studies exploiting macrophage-based experimental models have been adopted with success only by few groups.20-24
On this basis, the objective of this study is 3-fold: (1) to identify the amino acid domain(s) responsible for the antiviral activity of F12-Vif; (2) to set up an anti–HIV-1 gene therapy model based on macrophages differentiated from CD34+ HSC cells; and (3) to identify the step(s) of the HIV-1 life cycle affected by the inhibitory activity of the Vif mutant(s) and thereby their mechanism of action. To achieve these goals, we constructed 3 chimeric proteins, Chim1-3, expressing different portions of F12-Vif in the NL4-3 WT-Vif background and tested them for efficacy in CD4+ T cells and cord blood (CB)–derived CD34+ HSC-differentiated macrophages. Here, we provide evidence that Chim3 highly suppresses HIV-1 replication in both types of primary cells. Of major interest, we have also elucidated the dual mechanism of action of Chim3. It acts as a dominant-negative factor relative to hA3G degradation, and it reduces early retrotranscripts accumulation and, therefore, subsequent HIV-1 DNA integration, regardless of the presence of hA3G and WT-Vif.
Methods
Cells
The HEK-293T cells were propagated in Iscove modified Dulbecco medium supplemented with 10% fetal calf serum (EuroClone, Paignton, United Kingdom) and a combination of penicillin-streptomycin and glutamine. The CEM A3.01,25 SupT1, and ACH-2 cells, a CEM A3.01 subclone carrying a single copy of HIV-1LAI provirus,26 T-cell lines were grown in RPMI 1640 containing 10% fetal calf serum and penicillin-streptomycin and glutamine.
Neonatal leukocytes and CD34+ HSCs were purified from umbilical cord blood (UCB) centrifugation on a Ficoll-Hypaque gradient (Lymphoprep; Nycomed Pharma, Oslo, Norway). After centrifugation, CD4+ T cells or CD34+ HSCs were isolated from the collected CB mononucleated cells ring by negative selection using CD4+ T-cell isolation kit II (Miltenyi Biotec, Sunnyvale, CA) and positive selection using CD34 MicroBeads Kit and MiniMACS Separator Columns (Miltenyi Biotec), respectively. Purity (> 95% for CD4+ and > 92% for CD34+ cells) was confirmed by fluorescence-activated cell sorter (FACS) analysis (FACSCalibur; BD Biosciences, San Jose, CA) and FlowJo software (TreeStar, Ashland, OR), using anti-CD4 and CD34-PE antibody (Ab), respectively (BD Biosciences PharMingen, San Diego, CA). CD4+ T lymphocytes were expanded for 3 days by the Dynabeads CD3/CD28 T-cell expander (Dynal Biotech, Lake Success, NY) at 0.5 beads/cell ratio. CD34+ cells were differentiated to macrophages as described in Document S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Plasmids, production of LVs, and cell transduction by LVs
Plasmid and LV constructions, as well as transduction conditions, are described in details in Document S1 and Figure S1.
R9Δenv-HIV1/VSV-G production, HIV-1 infection, p24Gag ELISA, and RT activity assay
HIV-1 infectivity/integration assay of Figures 4E, 6E, and S5A, which assess the role of Chim3 and F12-Vif in producer cells, was performed as follows. The VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were obtained by cotransfection of either empty, Chim3-, or F12-Vif–transduced HEK-293T cells with the corresponding HIV-1 plasmids, the pMD.G vector encoding the VSV-G envelope glycoprotein,27 and, for Figures 4E and S5A, the pCEM15 plasmid at the ratio of 1:1:0.5. The viruses were used at a multiplicity of infection (MOI) of 4. The level of HIV-1 DNA integration was evaluated either indirectly by FACS analysis of the intracellular level of p24Gag using the BD Cytofix/Cytoperm-Fixation/Permeabilization kit (BD Biosciences) and the Kc57 FITC monoclonal Ab (Beckman Coulter, Fullerton, CA) or directly by TaqMan polymerase chain reaction (PCR) analysis as detailed in “LV and HIV-1 DNA copy number quantification by real-time TaqMan PCR.” The viruses used in HIV-1 infectivity/integration assay of Figures 6C,D and S6, in which the role of Chim3 is verified in target cells, were produced in mock HEK-293T cells as described in this section, but without hA3G.
HIV-1 infection was performed by exposing T cells at the indicated MOI with the following HIV-1 molecular clones: the X4 HIV-1 NL4-3, the R5 HIV-1 AD8 (ABI; Advanced Biotechnologies, Columbia, MD), AD1, kindly provided by Dr K. Peden (Food and Drug Administration, Bethesda, MD), and the laboratory-adapted HIV-1 BaL as previously described.5 CD34+ HSC-derived macrophages were infected at an MOI of 0.01 with the following R5 strains: the laboratory-adapted HIV-1 BaL, the molecular clone AD1, and the primary isolate TZ97001, donated by Dr G. Scarlatti (DIBIT, HSR, Milano, Italy). Reverse transcriptase (RT) activity assay and p24Gag ELISA (Coulter test kit; Beckman Coulter) were performed as previously described.5
LV and HIV-1 DNA copy number quantification by real-time TaqMan PCR
The copy number of the integrated LVs was established by quantitative PCR using an ABI Prism 7900 FAST instrument and analyzed by SDS 2.3 software (Applied Biosystems, Foster City, CA). Genomic DNA (gDNA) was amplified with the following primers and probe derived from the ΔLNGFR gene: forward: 5′-GAC CAC AGT GAT GGG CAG CT-3′; reverse: 5′-GCC TTG TAA GTC ATT GGT CTT AAA CG-3′; nerve growth factor receptor (NGFR) probe: FAM 5′-TGA CCC GAG GCA CCA CCG ACA-3′ TAMRA. PCR conditions are the following: 2 minutes at 50°C and for 5 minutes at 95°C, followed by 40 cycles for 15 seconds at 95°C and 15 seconds at 60°C, with an increment of 0.1°C/cycle.
The copy number of HIV-1 DNA was determined by the same method using the following primers and probe derived from the p24-gag region of HIV-1: forward: 5′-ACA TCA AGC AGC CAT GCA AAT-3′; reverse: 5′-ATC TGG CCT GGT GCA ATA GG-3′; Gag probe: FAM 5′-CAT CAA TGA GGA AGC TGC AGA ATG GGA TAG A-3′ TAMRA.28 Standard curves were obtained by gDNA of ACH-2 cells with a linear distribution (r = 0.99). The intersample variation was monitored by the amplification of the housekeeping telomerase gene. The thermal cycling conditions were: 50°C for 2 minutes and 95°C for 15 minutes, followed by 40 cycles for 15 seconds at 95°C and 60 seconds at 60°C, with an increment of 0.1°C/cycle.
Western blot and coimmunoprecipitation analyses
Whole-cell extracts (WCEs) and viral proteins derived from isolated cell-free virions were prepared as previously described.29 Western blot analysis was performed as in Vallanti et al.5 HIV-1 HXB2 Vif rabbit antiserum30 was obtained through the AIDS Research and Reference Reagent Program (Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD) from Dr D. Gabuzda and used at 1:1000 dilution. The rabbit anti-hA3G, donated by Dr W. C. Greene (Gladstone Institute of Virology and Immunology, San Francisco, CA),31 was used at 1:4000 dilution. The rabbit antiactin and the anti-HA monoclonal Ab (clone HA-7; Sigma-Aldrich, St Louis, MO) were used at 1:2000 and 1:10 000 dilutions, respectively. A serum obtained from an HIV-1+ patient was used at 1:2000 dilution.
Coimmunoprecipitations were performed as follows: HEK-293T cells were cotransfected with the Vifs-tag vectors in the possible combinations to determine both the WT-Vif and Chim3 homodimers and WT-Vif/Chim3 heterodimer. After 36 hours, cells were lysed in the lysing buffer (150 mM NaCl, 50 mM Tris-HCl, pH 7.5, 0.5% NP-40, and a cocktail of protease inhibitors). A total of 500 μg cell lysates/sample was immunoprecipitated with 5 μg mouse anti-HA Ab (clone HA-7; Sigma-Aldrich) coupled to 20 μL protein G–conjugated Sepharose 4 Fast Flow (GE Healthcare Bio-Sciences, Little Chalfont, United Kingdom) for 3 hours rotating at 4°C. The Sepharose beads were washed 4 times with the washing buffer (150 mM NaCl, 20 mM Tris-HCl, pH 7.5, 0.5% NP-40). After elution from the beads with 2× Laemmli buffer and boiling, the coimmunoprecitated complexes were run into sodium dodecyl sulfate–polyacrylamide gel electrophoresis followed by Western blot analysis using rabbit anti-c-Myc Ab (Sigma-Aldrich) at 1:600 dilution and mouse anti-HA Ab.
Results
Construction of LVs expressing chimeric Vifs
To determine the amino acid region(s) responsible for the antiviral activity of F12-Vif,5 we generated 2 chimeras, Chim1 and Chim2, by swapping the C- and N-terminal domains of the WT-vif gene with those of the F12-vif gene. Chim1 carries the first 87 N-terminal amino acids (1-87), whereas Chim2 carries the last 105 C-terminal amino acids (88-192) of F12-Vif, respectively (Figure S1A,B). We cloned the chimeras into the HIV-based second-generation LV, PΔN (Figure S1C),5 in which the transgene is up-regulated over a basal constitutive level in the presence of Tat and thereby in HIV-1–infected cells only.5
Southern blot analysis of gDNA derived from LV-transduced cells revealed correct-in-size bands of the integrated LVs (data not shown).
The C-terminal domain of F12-Vif possesses antiviral activity
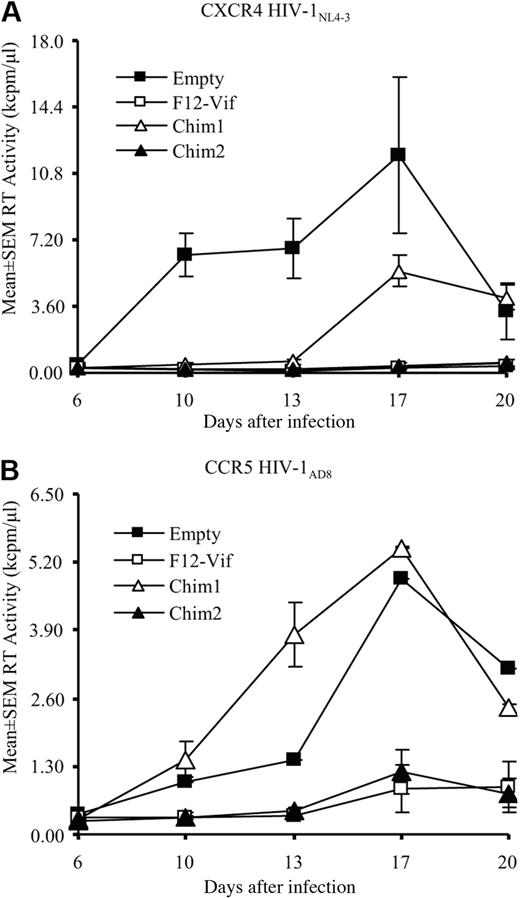
Next, we compared the potential antiviral activity of the 2 chimeras with that of F12-Vif by infecting LV-transduced CD4+ T lymphocytes with the X4 NL4-3 and the R5 AD8 molecular clones at an MOI of 0.1 (Figure 1). Chim1 weakly reduces the production of the X4 virus (Figure 1A) and has no antiviral activity against the R5 HIV strain (Figure 1B), whereas Chim2 inhibits HIV-1 replication of both viral strains to an extent comparable with that of F12-Vif (Figure 1A,B). Similar and highly reproducible findings were obtained with transduced CEM A3.01 T cells (data not shown). The lack of inhibition of Chim1 was not the result of any defects in Chim1-LV or Chim1 protein itself being this protein accumulated in stably transduced CEM A3.01 cells as much as WT-Vif was (Figure S3A). Of note and in contrast to Chim1, Chim2 expression was lower compared with the other Vifs (Figure S3A); nevertheless, it exerted antiviral activity (Figure 1). Overall, these results indicate that the anti–HIV-1 function of F12-Vif primarily resides in its C-terminal half and that there is no correlation between the intracellular level of Vif proteins and their HIV-1 inhibitory role, as was previously proposed.32
The C-terminal domain of F12-Vif possesses antiviral activity. CB-derived CD4+ T lymphocytes transduced with empty, F12-Vif-, Chim1-, or Chim2-LV were infected in triplicate cultures with either the X4 HIV-1 NL4-3 (A) or the R5 HIV-1 AD8 (B) molecular clones at an MOI of 0.1. Supernatants of the kinetic of infection were collected every 4 days, stored at −20°C, and then assessed for RT activity.
The C-terminal domain of F12-Vif possesses antiviral activity. CB-derived CD4+ T lymphocytes transduced with empty, F12-Vif-, Chim1-, or Chim2-LV were infected in triplicate cultures with either the X4 HIV-1 NL4-3 (A) or the R5 HIV-1 AD8 (B) molecular clones at an MOI of 0.1. Supernatants of the kinetic of infection were collected every 4 days, stored at −20°C, and then assessed for RT activity.
Chim3 inhibits X4 and R5 HIV-1 replication in CD4+ T lymphocytes
Based on these findings and on the fact that the C-terminal region of F12-Vif contains 5 mutated amino acids clustered within the HCCH domain at the location 127NVVRLS132 (the letters underlined and in bold represent the unique F-12-Vif–specific amino acid mutations), which is a potential good candidate for antiviral function (Figure S1A), we shortened the F12-Vif region by constructing a third chimera, Chim3. The sequence spanning from G126 to T170 of wild-type NL4-3 Vif was substituted with the corresponding sequence of F12-Vif (Figure S1B). Chim3-LV was generated similarly to the previously described LVs, and CEM A3.01 cells, CD4+ T lymphocytes, and CD34+-derived macrophages (“F12-Vif and Chim3 prevent HIV-1 replication in macrophages terminally differentiated from UCB-derived CD34+ HSCs”) were transduced and purified by NGFR selection.
The basal expression of Chim3 was compared with that of WT-Vif by Western blot. Of interest, like Chim2, the amount of Chim3 was lower than that of WT-Vif in all cell types (Figure S3B) for a faster and/or more efficient degradation into the 26S proteasome, as proved by the use of the MG132 proteasome inhibitor (Figure S3C). Furthermore, as expected, HIV-1 infection superinduced Chim3 production (Figure S3D).
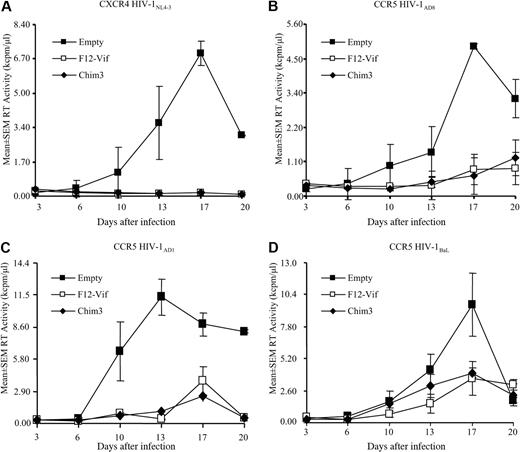
CD4+ T lymphocytes were challenged with either the X4 NL4-3 or the R5 AD8 and AD1 molecular clones and the laboratory-adapted BaL HIV-1 strains at an MOI of 0.1. Chim3 inhibited HIV-1 replication of both viral strains to the same extent as F12-Vif (Figure 2). The antiviral action of Chim3-LV was evaluated also in transduced CEM A3.01 cells, obtaining results highly reproducible and equivalent to those of primary T cells (data not shown). These findings suggest that the last 22 C-terminal amino acids of F12-Vif, which discriminate Chim2 from Chim3, are dispensable for the inhibitory function of the protein.
Chim3 inhibits HIV-1 replication analogously to F12-Vif. LV-transduced CB-derived CD4+ T lymphocytes were infected in triplicate cultures with either the X4 NL4-3 (A) or the R5 AD8 (B) and AD1 (C) molecular clones or the R5 laboratory-adapted BaL (D) HIV-1 strains at an MOI of 0.1. Culture supernatants were harvested every 4 days, stored at −20°C, and then assessed for RT activity.
Chim3 inhibits HIV-1 replication analogously to F12-Vif. LV-transduced CB-derived CD4+ T lymphocytes were infected in triplicate cultures with either the X4 NL4-3 (A) or the R5 AD8 (B) and AD1 (C) molecular clones or the R5 laboratory-adapted BaL (D) HIV-1 strains at an MOI of 0.1. Culture supernatants were harvested every 4 days, stored at −20°C, and then assessed for RT activity.
F12-Vif and Chim3 prevent HIV-1 replication in macrophages terminally differentiated from UCB-derived CD34+ HSCs
To set up an efficient experimental model for gene therapy studies in macrophages, we transduced CD34+ HSCs with the empty-, F12-Vif–, and Chim3-LVs and, after NGFR-mediated immune selection, induced their maturation to macrophages (Figure S4A).
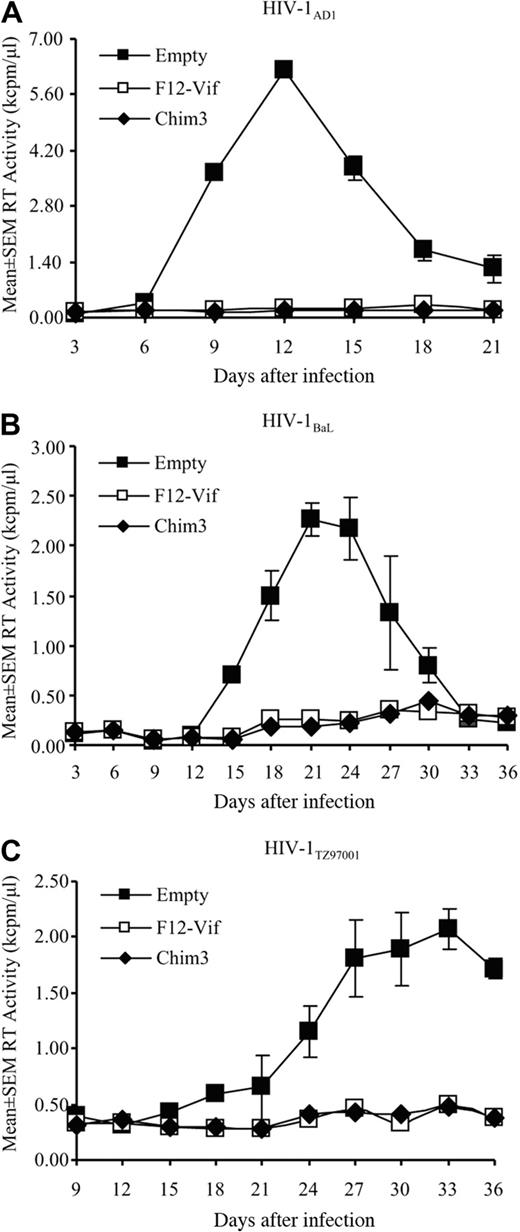
Thus, to assess whether F12-Vif and Chim3 were effective against HIV-1 also in primary macrophages, cells were challenged with 3 CCR5-tropic HIV-1 strains: the molecular clone HIV-1 AD1 (Figure 3A), the laboratory-adapted HIV-1 BaL (Figure 3B), and the primary isolate TZ97001 (Figure 3C) at an MOI of 0.01, which was the most productive MOI among those tested for macrophage infection (Figure S4B). Empty transduced cells supported productive infection, whereas F12-Vif– and Chim3-expressing macrophages were efficiently protected from replication of all viruses (Figure 3), confirming the antiviral activity of both transgenes also in the macrophagic experimental model.
Both F12-Vif and Chim3 protect macrophages from HIV-1 challenge. CD34+-derived empty, F12-Vif–, and Chim3-transduced macrophages were infected in quintuplicate cultures with 3 different R5 HIV-1 strains, the molecular clone AD1 (A), the laboratory-adapted BaL (B), and the primary isolate TZ97001 (C) at an MOI of 0.01, and the kinetics of infection were followed for 3 to 5 weeks.
Both F12-Vif and Chim3 protect macrophages from HIV-1 challenge. CD34+-derived empty, F12-Vif–, and Chim3-transduced macrophages were infected in quintuplicate cultures with 3 different R5 HIV-1 strains, the molecular clone AD1 (A), the laboratory-adapted BaL (B), and the primary isolate TZ97001 (C) at an MOI of 0.01, and the kinetics of infection were followed for 3 to 5 weeks.
Chim3 does not rescue the replication of ΔvifHIV-1 in T cells and CD34+-derived macrophages
We have previously shown that Δvif-HIV-1, which is growth-defective in nonpermissive cells because of the expression of hA3G, normally spreads in these cells when either WT-Vif or F12-Vif are expressed in trans by LV transduction.5 Both proteins indeed degrade efficiently hA3G and thus allow the replication of vif-deficient HIV-1.5 Therefore, to better characterize the functional features of Chim3 compared with those of F12-Vif, we verified whether Chim3, like F12-Vif, rescues the replication of Δvif-HIV-1 in nonpermissive cells. To this aim, we infected mock-, F12-Vif–, and Chim3-transduced CEM A3.01 cells, CD4+ T lymphocytes, and macrophages with either X4 or R5 vif-deficient HIV-1 strains at an MOI of 0.1. Strikingly, Chim3, in contrast to F12-Vif, did not recover the replication of vif-deficient viruses in the 3 different experimental settings (Figure 4A-C). These findings demonstrate that Chim3 profoundly differs from F12-Vif in relation to hA3G because it is functionally incapable of neutralizing the antiviral action of this HIV-1 cellular restriction factor.
Chim3 does not counteract the antiviral action of hA3G, by acting as a true dominant-negative factor. Kinetic of infections of CEM A3.01 cells (A), CD4+ T lymphocytes (B), and CD34+-derived macrophages (C) infected with either X4 Δvif-HIV-1 (A,B) or R5 Δvif-HIV-1 (C) at an MOI of 0.1. Values represent mean plus or minus SEM of triplicate (A,B) and quintuplicate (C) cultures. (D) Western blot analysis of cell extracts derived from HEK-293T cells transfected with a fixed amount of hA3G-HA and either WT-Vif– or Chim3-expressing plasmids at the indicated amounts of plasmid DNA. Cell extracts were prepared 48 hours after transfection. Membranes were sequentially probed with anti-HA Abs (top panel), anti-Vif (middle panel), and antiactin (bottom panel) Abs. (E) VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were produced by transient transfection of the corresponding plasmids in either empty or Chim3-transduced HEK-293T cells, in the presence of hA3G expression plasmid. SupT1 cells were infected at an MOI of 4. Seventy-two hours after viral challenge, intracellular p24Gag expression was evaluated by FACS analysis (FACSCalibur, BD Biosciences; and FlowJo software, TreeStar) using an anti-p24Gag Ab on fixed and then permeabilized cells. Values represent the mean plus or minus SEM percentage of the p24Gag content of each condition relative to that of wild-type HIV-1 (HIV-1 ■) (n = 6). (F) Western blot analysis of the level of the intracellular (left panel) and intravirion (right panel) hA3G and Vif proteins; 40 μg WCE and 1 μg p24Gag HIV-1 virion equivalent, respectively, were loaded in each conditions. The filter was sequentially probed with the different Abs as indicated.
Chim3 does not counteract the antiviral action of hA3G, by acting as a true dominant-negative factor. Kinetic of infections of CEM A3.01 cells (A), CD4+ T lymphocytes (B), and CD34+-derived macrophages (C) infected with either X4 Δvif-HIV-1 (A,B) or R5 Δvif-HIV-1 (C) at an MOI of 0.1. Values represent mean plus or minus SEM of triplicate (A,B) and quintuplicate (C) cultures. (D) Western blot analysis of cell extracts derived from HEK-293T cells transfected with a fixed amount of hA3G-HA and either WT-Vif– or Chim3-expressing plasmids at the indicated amounts of plasmid DNA. Cell extracts were prepared 48 hours after transfection. Membranes were sequentially probed with anti-HA Abs (top panel), anti-Vif (middle panel), and antiactin (bottom panel) Abs. (E) VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were produced by transient transfection of the corresponding plasmids in either empty or Chim3-transduced HEK-293T cells, in the presence of hA3G expression plasmid. SupT1 cells were infected at an MOI of 4. Seventy-two hours after viral challenge, intracellular p24Gag expression was evaluated by FACS analysis (FACSCalibur, BD Biosciences; and FlowJo software, TreeStar) using an anti-p24Gag Ab on fixed and then permeabilized cells. Values represent the mean plus or minus SEM percentage of the p24Gag content of each condition relative to that of wild-type HIV-1 (HIV-1 ■) (n = 6). (F) Western blot analysis of the level of the intracellular (left panel) and intravirion (right panel) hA3G and Vif proteins; 40 μg WCE and 1 μg p24Gag HIV-1 virion equivalent, respectively, were loaded in each conditions. The filter was sequentially probed with the different Abs as indicated.
Chim3 does not reduce the intracellular level of the restriction factor hA3G
To formally prove that Chim3 indeed does not degrade hA3G, we cotransfected HEK-293T cells with a fixed amount of HA-tagged hA3G-expressing plasmid and increasing amounts of either Chim3- or WT-Vif–expressing vectors. Forty-eight hours after transfection, the different protein levels were assessed by Western blot (Figure 4D). As expected, WT-Vif eliminated hA3G dose-dependently, whereas Chim3 was incompetent to do so even at the highest quantity of transfected DNA. In line with the results of Figure S3, Chim3 was expressed at a lower level compared with WT-Vif, despite that an identical amount of transfected plasmid DNA was used (Figure 4D, compare lanes 2 vs 5, 3 vs 6, and 4 vs 7). To determine the relative contribution of either the low level of Chim3 or the intrinsic inability of this mutant to induce hA3G degradation, or both, densitometric evaluation of the intensity of hA3G and Vif bands (actin-normalized) was carried out. After 100- and 300-ng plasmid DNA transfection, WT-Vif reduced the expression of hA3G almost completely (95%) in both conditions, whereas the Chim3-induced degradation of hA3G corresponded to 16% and 29%, respectively. Most importantly, the estimate of hA3G degradation induced by Chim3 and WT-Vif on a per Vif-molecule basis (calculated by measuring the hA3G/Vif ratio) indicated that Chim3 is approximately 6-fold less efficient than WT-Vif at both concentrations of plasmid. At the lowest plasmid concentration (10 ng), Chim3 band was almost undetectable, therefore making the quantification unreliable. Overall, these data indicate that Chim3 does not induce the disappearance of hA3G because of its intrinsic inability to do so and also, partially, for its low expression level.
Chim3 acts as a dominant-negative factor regarding hA3G degradation
To better analyze the functional defectiveness of Chim3 either alone or in the presence of WT-Vif in regards to hA3G, that is, its potential dominant negative feature, we measured the infectivity/integration level of HIV-1 virions in single-cycle infection experiments. VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 containing hA3G were generated from either empty or Chim3-expressing HEK-293T cells. SupT1 cells were infected with the resulting viruses, and virion infectivity/integration was calculated by measuring the level of intracellular p24Gag expression that, being detectable only after provirus integration, gives an estimate of HIV-1 DNA integration. The effect of hA3G and Chim3 was determined as percentage infectivity/integration values of HIV-1 carrying them relative to the empty vector alone carrying sample (Figure 4E, HIV-1 black bar). Chim3-producer cells generated a R9Δenv-HIV-1 that, once integrated, expressed a lower level of p24Gag (mean ± SEM, 47% ± 4%) compared with the virus generated from empty transduced cells (Figure 4E), indicating that Chim3 somehow prevents the HIV-1 Vif-mediated degradation of hA3G. In line with the Δvif-HIV-1 rescue experiments of Figure 4A to C, R9Δenv-Δvif-HIV-1 was, as expected, heavily impaired in its ability to integrate compared with R9Δenv-HIV-1 (Figure 4E right HIV-1 black bar, mean ± SEM, 12% ± 1%). Yet, Chim3 alone was incompetent to overcome the effect of hA3G. Rather, it further decreased the infectivity/integration level compared with control viruses (Figure 4E right bars, mean ± SEM, 6% ± 1%). Overall, these findings established that Chim3 shows a dominant-negative feature regarding hA3G. To biochemically prove this feature, we carried out Western blot experiments using cellular and viral proteins derived from 2 representative VSV-G-HIV-1 stocks used in Figure 4E to detect hA3G and Vif content. Human A3G and Vif bands (normalized with actin and p24Gag in cell and viral lysates, respectively) were quantified by densitometry. The intracellular level of hA3G was in line with the results of Figure 4D; the amount of hA3G of lane 2 was 20% higher than that of lane 1 and very close to that of lanes 3 (30% less intense) and 4 (identical) (Figure 4F). Similarly, the amount of intravirion hA3G matches with an inverse correlation the functional data of Figure 4E (Figure 4F).
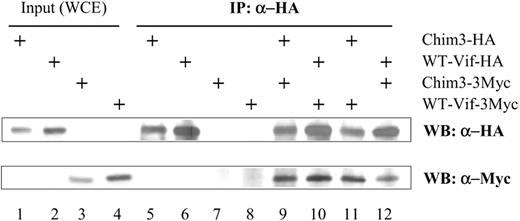
Thus, to prevent hA3G degradation, Chim3 could either escort WT-Vif to the proteosome or form nonfunctional WT-Vif/Chim3 heterodimers. To discriminate between these 2 possibilities, the filter was probed with anti-Vif Ab (Figure 4F middle panel). The results clearly established that the intensity of Vif bands in lanes 2 and 6 was equal to that of Vif in lanes 1 and 5, respectively. Therefore, the former hypothesis was ruled out. To verify the second hypothesis, we performed coimmunoprecipitation experiments using Chim3 and WT-Vif differentially tagged with HA and 3-Myc at the C-terminus (Figure 5). We were able to detect both WT-Vif and Chim3 homodimers as well as WT-Vif/Chim3 heterodimers using anti-HA Abs for immunoprecipitation (Figure 5). These results strongly suggest that Chim3 might form nonfunctional heterodimers with the incoming and newly produced HIV-1 Vif during infection.
Coimmunoprecipitation of WT-Vif/Chim3 heterodimers. A total of 500 μg cellular lysates derived from HEK-293T cells cotransfected with the tagged Vifs-expressing constructs was immunoprecipitated (IP) with the anti-HA Ab and then immunoblotted with either the anti-myc or the anti-HA Abs, as indicated. The WT-Vif and Chim3 homodimers were loaded as positive controls of the coimmunoprecipitation, and the input WCE (40 μg) as positive control of the Western blot.
Coimmunoprecipitation of WT-Vif/Chim3 heterodimers. A total of 500 μg cellular lysates derived from HEK-293T cells cotransfected with the tagged Vifs-expressing constructs was immunoprecipitated (IP) with the anti-HA Ab and then immunoblotted with either the anti-myc or the anti-HA Abs, as indicated. The WT-Vif and Chim3 homodimers were loaded as positive controls of the coimmunoprecipitation, and the input WCE (40 μg) as positive control of the Western blot.
Finally, F12-Vif producer cells generated both R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 more infectious than empty-LV producer cells (Figure S5A). In line, the level of hA3G was much lower in the 2 viruses released from F12-Vif–producer cells than those budded out from empty-producer cells, suggesting that WT-Vif and F12-Vif cooperate to eliminate hA3G (Figure S5B) and, in so doing, eventually drive higher infectivity.
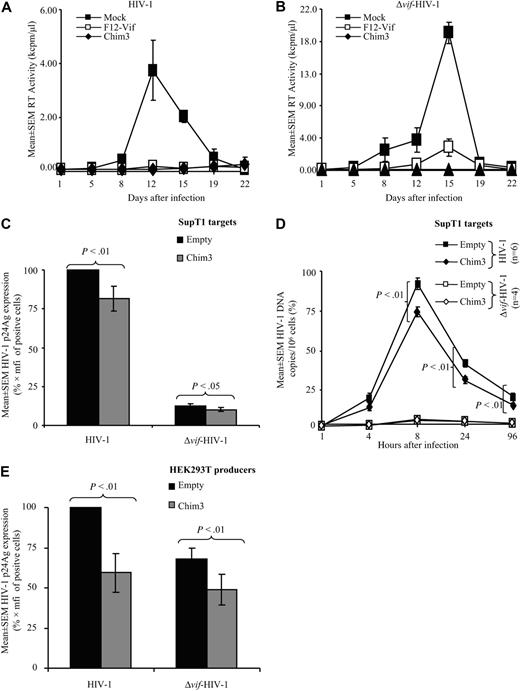
Chim3 inhibits HIV-1 replication also in permissive cells
The fact that Chim3, in the absence of WT-Vif, induced a further decrease in the integration of R9Δenv-Δvif-HIV-1 (Figure 4E) may depend on the fact that Chim3 somehow potentiates the antiviral function of hA3G. Alternatively, Chim3 could affect some other steps of the HIV-1 life cycle regardless the presence of hA3G. To verify the latter hypothesis, which is sustained by ours (A. Kataropoulou, C.B., A. Belfiore, S. Trabatti, A. Garbelli, S.P., R.L., and G. Maga, manuscript submitted 2009) and other reports showing a role of Vif on reverse transcription process,33-35 we infected mock-, Chim3- and F12-Vif–transduced SupT1 cells with NL4-3 HIV-1 and Δvif-HIV-1 at an MOI of 0.1 and 1, respectively, and followed the kinetic of infection for 22 days. Similarly to F12-Vif,5 Chim3 protected permissive cells from replication of both types of HIV-1 (Figure 6A,B). Overall, these results indicate that Chim3 prevents HIV-1 replication in an hA3G-dependent and, similarly to F12-Vif,5 also in an hA3G-independent manner.
Chim3 blocks HIV-1 replication regardless the presence of hA3G. Empty-, F12-Vif–, and Chim3-transduced permissive SupT1 cells were infected in triplicate cultures with the X4 NL4-3 molecular clone (A) or the Δvif HIV-1 (B) at an MOI of 0.1 and 1, respectively. Supernatants of the kinetic of infection were collected every 3 to 4 days, stored at −20°C, and then assessed for RT activity. Values represent mean plus or minus SEM of triplicate cultures. (C) VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were produced by transient transfection of HEK-293T cells and used at an MOI of 4 to infect either empty-LV- or Chim3-LV–transduced SupT1 cells. Seventy-two hours after viral challenge, intracellular p24Gag level was evaluated by FACS analysis using an anti-p24Gag Ab on fixed and then permeabilized cells. Values express mean plus or minus SEM percentage of the p24Gag expression of each condition (n = 5) relative to that of wild-type HIV-1 on empty transduced cells (HIV-1 ■). (D) The same viruses of panel C were used to carry out a kinetic of single round infection for the indicated time points on empty and Chim3-transduced SupT1 cells. (E) VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were produced by transient transfection of the corresponding molecular clones in either empty or Chim3-transduced HEK-293T cells. SupT1 cells were infected at an MOI of 4. Seventy-two hours after single round infection, intracellular p24Gag expression was evaluated by FACS analysis (FACSCalibur, BD Biosciences; and FlowJo software, TreeStar) using an anti-p24Gag Ab on fixed and then permeabilized cells. Values indicate mean plus or minus SEM percentage of p24Gag expression of each condition (n = 6) relative to that of wild-type HIV-1 (HIV-1 ■).
Chim3 blocks HIV-1 replication regardless the presence of hA3G. Empty-, F12-Vif–, and Chim3-transduced permissive SupT1 cells were infected in triplicate cultures with the X4 NL4-3 molecular clone (A) or the Δvif HIV-1 (B) at an MOI of 0.1 and 1, respectively. Supernatants of the kinetic of infection were collected every 3 to 4 days, stored at −20°C, and then assessed for RT activity. Values represent mean plus or minus SEM of triplicate cultures. (C) VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were produced by transient transfection of HEK-293T cells and used at an MOI of 4 to infect either empty-LV- or Chim3-LV–transduced SupT1 cells. Seventy-two hours after viral challenge, intracellular p24Gag level was evaluated by FACS analysis using an anti-p24Gag Ab on fixed and then permeabilized cells. Values express mean plus or minus SEM percentage of the p24Gag expression of each condition (n = 5) relative to that of wild-type HIV-1 on empty transduced cells (HIV-1 ■). (D) The same viruses of panel C were used to carry out a kinetic of single round infection for the indicated time points on empty and Chim3-transduced SupT1 cells. (E) VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 were produced by transient transfection of the corresponding molecular clones in either empty or Chim3-transduced HEK-293T cells. SupT1 cells were infected at an MOI of 4. Seventy-two hours after single round infection, intracellular p24Gag expression was evaluated by FACS analysis (FACSCalibur, BD Biosciences; and FlowJo software, TreeStar) using an anti-p24Gag Ab on fixed and then permeabilized cells. Values indicate mean plus or minus SEM percentage of p24Gag expression of each condition (n = 6) relative to that of wild-type HIV-1 (HIV-1 ■).
Chim3 prevents HIV-1 DNA integration in single round infection when it is expressed in target cells
To further investigate the hA3G-independent antiviral role of Chim3 with particular attention to its function when it is expressed in target cells, we evaluated the integration of HIV-1 DNA in SupT1 cells transduced with either the empty or Chim3-LVs and infected with the VSV-G pseudotyped R9Δenv-HIV-1 and R9Δenv-Δvif-HIV-1 produced in mock HEK-293T cells (Figure 6C). The mean plus or minus SEM of p24Gag expression on Chim3 target cells was assessed as percentage values relative to the value on empty vector target cells after 72 hours of infection (Figure 6C HIV-1 black bar). Chim3 in target cells reduced the integration of HIV-1 during the first round of infection also in the absence of hA3G. Results comparable with those of the intracellular p24Gag expression were obtained by calculating the HIV-1 DNA copy number by TaqMan PCR (data not shown). In addition, p24Gag-based viral normalization (Figure S6A) leads to results comparable with those obtained by MOI normalization (Figure 6C).
The infectivity/integration assay analyzed at 72 hours after infection, however, does not discriminate whether Chim3 affects the reverse transcription and/or the integration step of the HIV-1 life cycle. To elucidate this issue, we measured the copy number of HIV-1 retrotranscripts in both empty and Chim3-transduced SupT1 cells during an early kinetic of infection using VSV-G-HIV-1s (Figure 6D). After 8 hours, HIV-1 retrotranscripts are not integrated yet, thereby providing an estimate of the reverse transcription efficiency. Of note, after 8 and 24 hours, Chim3 target cells infected with R9Δenv-HIV-1 showed a statistically significant reduction of the reverse transcripts accumulation compared with empty target cells (Figure 6D). These data demonstrate that Chim3 affects the reverse transcription reaction, which consequently leads to a reduction in HIV-1 DNA integration.
Chim3 prevents HIV-1 DNA integration in single round infection when it is expressed in producer cells also in the absence of hA3G
Next, we wished to verify whether Chim3 expressed in producer cells in the absence of hA3G is still able to reduce the infectivity/integration of HIV-1. To this aim, we performed single round infectivity/integration assay using VSV-G-R9Δenv-HIV-1 and VSV-G-R9Δenv-Δvif-HIV-1 produced from empty or Chim3-LV–transduced HEK-293T cells to infect SupT1 cells (Figure 6E). Chim3 reduces, in a statistically significant manner, the infectivity/integration of both viruses (Figure 6E). These findings further exclude the possibility that Chim3-mediated reduction of infectivity (Figure 4E) depends on a Chim3 auxiliary effect on hA3G. Instead, they suggest that Chim3 exerts an intrinsic inhibitory function on RT reaction regardless of the presence of both WT-Vif and hA3G.
Moreover, as we observed lower integration of VSV-G-R9Δenv-Δvif-HIV-1 compared with VSV-G-R9Δenv-HIV-1 in transduced SupT1 cells, we wondered whether transduction itself somehow contributes to this effect. Infection of mock-transduced cells excluded this idea because also in these cells Δvif-HIV-1 integrates less efficiently compared with proficient HIV-1 (Figure S6B).
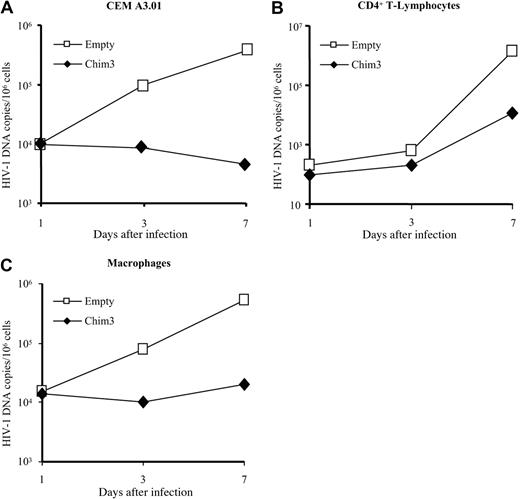
Chim3 blocks HIV-1 DNA integration during productive infection in T cells and macrophages
Finally, to confirm the Chim3-dependent HIV-1 DNA integration block also during a kinetic of infection, we determined the HIV-1 DNA copy number in CEM A3.01 cells (Figure 7A), CD4+ T lymphocytes (Figure 7B), and macrophages (Figure 7C) at 1, 3, and 7 days after viral challenge by quantitative real-time TaqMan PCR. In line with previous data, 3 days after infection, the HIV-1 DNA copy number in CEM A3.01 cells increased by almost 1-log in empty transduced cells, whereas it remained unaltered in Chim3-expressing cells and then slightly decreased at day 7 (Figure 7A). Consistently, we observed almost 2-log difference in the copy number between the empty and Chim3-transduced cells in both CD4+ T lymphocytes and macrophages after 7 days of HIV-1 infection (Figure 7B,C).
Chim3 blocks HIV-1 DNA integration in productive infection of CEM A3.01 cells, CD4+ T lymphocytes, and CD34+-derived macrophages. (A) Empty and Chim3-transduced CEM A3.01 cells were infected with the X4 HIV-1 NL4-3 molecular clone. (B) Empty and Chim3-transduced CD4+ T lymphocytes were infected with the R5 AD8 molecular clone. (C) Empty and Chim3-transduced CD34+-derived macrophages were infected with the laboratory-adapted R5 HIV-1 BaL. All cells were infected at an MOI of 0.1 for 7 days. Total DNA was extracted at the indicated time points, and the copy number of HIV-1 DNA was analyzed by quantitative real-time PCR. Values are representative of 1 of 3 independent experiments.
Chim3 blocks HIV-1 DNA integration in productive infection of CEM A3.01 cells, CD4+ T lymphocytes, and CD34+-derived macrophages. (A) Empty and Chim3-transduced CEM A3.01 cells were infected with the X4 HIV-1 NL4-3 molecular clone. (B) Empty and Chim3-transduced CD4+ T lymphocytes were infected with the R5 AD8 molecular clone. (C) Empty and Chim3-transduced CD34+-derived macrophages were infected with the laboratory-adapted R5 HIV-1 BaL. All cells were infected at an MOI of 0.1 for 7 days. Total DNA was extracted at the indicated time points, and the copy number of HIV-1 DNA was analyzed by quantitative real-time PCR. Values are representative of 1 of 3 independent experiments.
Discussion
In this study, we made progress on the gene therapy strategy we have been developing against HIV-1/AIDS based on F12-Vif mutant and its derivative Chim3 as therapeutic genes.5 First, we showed that the C-terminus of F12-Vif is endowed with anti–HIV-1 activity. Second, we confirmed the antiviral activity of F12-Vif, previously demonstrated on CD4+ T lymphocytes,5 and of Chim3, also in macrophages. Third, we established, by biochemical and functional experiments, that Chim3 acts by a dual mechanism. On one hand, Chim3 functions as a truly dominant-negative factor in regard to hA3G, thereby preserving the natural antiviral function of hA3G. On the other hand, Chim3 impairs the RT process independently of the presence of hA3G and WT-Vif.
The activity of F12-Vif and Chim3 is equally lethal against HIV-1, despite that Chim3 contains approximately one-fourth of F12-Vif amino acids. Of interest, the F12-Vif–derived 45-amino-acid region of Chim3 includes 5 mutations clustered (127NVVRLS132; the letters underlined and in bold represent the unique F-12-Vif–specific amino acid mutations) within the major loop of the HCCH Zn++-binding motif of Vif.11,12 This motif is critical for the interaction of Vif to Cullin5, being the latter part of the E3 ubiquitin ligase multiprotein complex responsible of hA3G proteasomal degradation.14 Of interest, despite that both F12-Vif and Chim3 contain this cluster, F12-Vif, but not Chim3, degrades hA3G, suggesting that probably a nonproper folding of Chim3 could explain this difference. Indeed, according to a molecular dynamics simulation of Vif structure,36 the N-terminal region of the protein seems to fold close to the Zn-binding domain. Furthermore, the ProtParam analysis we run through the ExPASy proteomics server (http://www.expasy.ch/tools/protparam.html)37 indicated that the amino acid charge distribution of F12-Vif (+15) is very similar, whereas that of Chim3 is drastically different (+8) from that of WT-Vif (+14). Charge distribution is the driving force of protein folding; therefore, the +8 value might explain why Chim3 behaves differently from WT-Vif and F12-Vif in regard to hA3G destruction. In addition, the amino acid substitution(s) present in the N-terminal region of F12-Vif, but not of Chim3, might compensate or abrogate the defect derived from the mutations present in the Zn-coordination domain. In support of the notion that the clustered mutations are crucial is also the fact that Chim3 does not bind Zn++ in a Zn++-based affinity chromatography (A. Kataropoulou, C.B., A. Belfiore, S. Trabatti, A. Garbelli, S.P., R.L., and G. Maga, manuscript submitted 2009). Furthermore, preliminary results aimed at analyzing the antiviral effect of Chim5, a chimera differing from Chim3 for the abrogation of the sixth mutation (142 V→I) within the F12-Vif 45-amino-acid region of Chim3, demonstrate that this mutation is irrelevant for the antiviral function of Chim3 (data not shown). This result reinforces the sufficiency of the 5-amino-acid cluster for antiviral activity.
Moreover, biochemical (Figure 4F) and functional (Figure 4E) analyses revealed that, despite that WT-Vif content is equal in the virions produced from both empty and Chim3-transduced HEK-293T cells, the amount of hA3G is not reduced at all. Furthermore, we demonstrated that Chim3 physically interacts with WT-Vif. Overall, these results suggest that Chim3 probably prevents hA3G degradation by forming Chim3/WT-Vif nonfunctional heterodimers.
Of major relevance, we determined that Chim3 blocks the retrotranscript accumulation and, consequently, HIV-1 DNA integration in single-cycle infections when Chim3 is expressed either in producer or, most importantly, in target cells regardless the presence of both hA3G and WT-Vif. Furthermore, Chim3 blocks HIV-1 DNA integration in T cells and macrophages after a few days after productive HIV-1 infection. Altogether, these results indicate that Chim3 affects the early steps of HIV-1 life cycle. In this regard, it has been recently described by 2 independent groups that Vif facilitates the RT reaction in vitro,33,35 and it is an integral part of the RT complex in vivo.35 The direct effect of Chim3 on RT reaction could depend on the higher affinity that Chim3 shows for the reverse transcriptase and the genomic RNA substrate, as we recently established (A. Kataropoulou, C.B., A. Belfiore, S. Trabatti, A. Garbelli, S.P., R.L., and G. Maga, manuscript submitted 2009). Indeed, we cannot exclude that Chim3, when expressed in producer cells, might alter the functionality and/or the level of RT in that location.
Our data indicate that Chim3 functions at both the early and late steps of the HIV-1 life cycle. In this regard, following a recently proposed classification of the anti–HIV-1/AIDS transgenes according to their mechanism of action, Chim3 belongs to class I, which collects transgenes inhibiting early stages of HIV-1 replication.2 These transgenes clearly provide protection from cell destruction and thereby confer a cell-growth advantage to transduced cells. Chim3-based gene therapy takes advantage of the fact that Chim3 is as little immunogenic as F12-Vif and WT-Vif are,5 foreseeing long-term persistence of transduced cells in vivo.
Finally, macrophages are among the firsT cells infected during HIV-1 transmission and contribute to cellular viral reservoirs during all stages of HIV-1 disease.19 Thus, the effectiveness of an anti–HIV-1/AIDS therapeutic gene should be determined in both CD4+ T lymphocytes and macrophages to increase the possibility of a successful approach. Thus, the macrophage-based experimental model for anti–HIV-1/AIDS gene therapy based on HSCs has a double advantage. On one hand, safety and feasibility of genetic manipulation of HSCs, and, on the other hand, anti–HIV-1 transgene efficacy in macrophages are analyzed in the same experimental setting. CD34+ HSCs undergo macrophage maturation in a manner identical to that of mock-transduced cells irrespective of the type of transgene contained within the vector, indicating that Vif genes do not alter the maturation process of macrophages. CD34+-HSC–derived macrophages therefore provide a useful experimental preclinical setting for gene therapy studies on HIV-1/AIDS.
In conclusion, our findings are relevant, as the ultimate reduction of HIV-1 DNA accumulation induced by Chim3 will allow patients living with HIV-1/AIDS to long-term control HIV-1 infection. This will eventually provide engineered HSC progenies and engineered T cells with survival advantage, which is a crucial requirement for an efficient reconstitution of the immune system, a key event to achieve the long-term control of HIV-1 replication.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr G. Vallanti for conducting preliminary experiments of the study, Drs A. Stornaiuolo and G. Musco for helpful suggestions on plasmid construction and protein analysis interpretation, respectively, Dr D. Trono for helpful suggestions and critical reading of the manuscript, and Prof F. Mavilio for initial support to this study.
This work was supported in part by TaKaRa Bio (Otsu, Japan).
Authorship
Contribution: S.P., L.A., and F.G. performed most of the experiments of the research and contributed to the conception and design of the experiments and to the interpretation of the results; R.L. performed several experiments of the research; C.O. performed some quantitative PCR analyses; G.-P.R. supervised the conception and design of experiments, the interpretation of the results, and the writing of the manuscript; and C.B. conceived and designed the experiments, supervised the crude data, interpreted the results, and wrote the manuscript.
Conflict-of-interest disclosure: The authors are employees of MolMed S.p.A. C.B. is inventor of the patent pub. no. WO/2006/111866.
Correspondence: Chiara Bovolenta, MolMed S.p.A., via Olgettina 58 Milano, 20132 Italy; e-mail: chiara.bovolenta@molmed.com.
References
Author notes
*S.P., L.A., and F.G. contributed equally to this study


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal