Introduction
Primary lymphoma of the central nervous system (PCNSL), defined as diffuse large B-cell lymphoma (DLBCL) confined to the central nervous system (CNS), has recently gained attention due to its increased incidence, which is mainly due to the AIDS epidemic and has been observed in some but not all series addressing immunocompetent patients.1
As morphology does not distinguish between PCNSL and extracerebral DLBCL, the question arose whether PCNSL constitutes a distinct lymphoma entity—as considered by the new WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. This is supported by the remarkably poorer prognosis of PCNSL compared with extracerebral DLBCL (Table S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). This clinical observation provides the rationale for intense scientific efforts to elucidate the biology of PCNSL. Three major issues need to be addressed to understand the nature of PCNSL and to develop specific therapeutic regimens: (1) the histogenetic origin of the tumor cells; (2) the transforming events; and (3) the role of the microenvironment of the CNS.
Histogenetic origin of the tumor cells of PCNSL
The CD19+ (100% of cases), CD20+ (100%), CD10+ (10%-20%), bcl6+ (60%-100%), and IRF4/MUM1+ (90%-100%) immunophenotype1,2 and the presence of rearranged, somatically mutated immunoglobulin (IG) genes with evidence for ongoing mutation suggest PCNSL tumor cells are derived from a germinal center (GC) exit B cell.3-5 PCNSL harbors a remarkably high load of somatic mutations of IG genes exceeding values described for systemic DLBCL (Table S1).4,5 This may indicate a prolonged GC reaction of the tumor cells. Comparison of gene expression profiles (GEP) of PCNSL and purified nonmalignant B-cell populations demonstrated that the tumor cells of PCNSL are more closely related to memory B cells than to GC B cells.3
Characteristically, subsequent B cell–maturation steps of the tumor cells are blocked, such as IG class switch recombination (CSR). The absence of CSR was attributed to Sμ deletions and low levels of activation-induced cytidine deaminase (Table S1).6 This observation raises the hypothesis that PCNSL originates from GC B cells destined to become IgM-expressing memory B cells, which can rapidly react on further antigenic stimulation. Such a mechanism may be advantageous to protecting the highly vulnerable CNS from infections because its regenerative potential is limited.
Transforming events in PCNSL
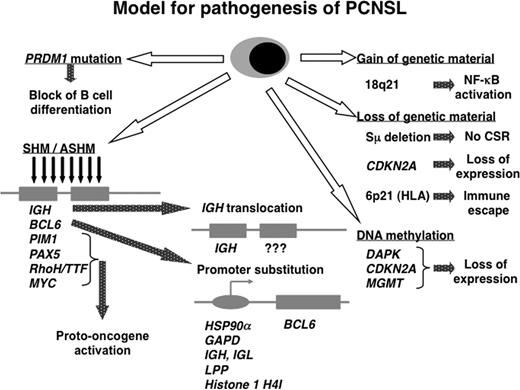
Several mechanisms may contribute to transformation in PCNSL: (1) chromosomal translocations; (2) gains and losses of genetic material; (3) ongoing aberrant somatic hypermutation (SHM); (4) mutations of tumor suppressor genes; (5) gene inactivation by DNA methylation; and (6) activation of the NF-κB complex.
Chromosomal translocations affecting the BCL6 or IG genes are recurrent in PCNSL (Table S1).7-9 In this regard and with respect to the promiscuity of BCL6 using various translocation partners, PCNSL does not differ from systemic DLBCL. With the exception of BCL6, the partner chromosomes of translocated IG genes so far have escaped identification and it remains to be determined whether PCNSL is distinct from systemic DLBCL in this respect. The most common genetic imbalances are 18q21 gains including both the BCL2 and MALT1 genes (Table S1).8,10,11 The tumor cells concomitantly express MALT1 and BCL10, which is in line with activation of the NF-κB pathway. This is further evidenced by increased transcript levels of genes of the NF-κB complex and NF-κB target genes compared with nonmalignant tonsillar centroblasts (Table S1).12 Two subgroups of PCNSL exhibiting significantly different BCL10, REL, and IAP1 transcript levels can be distinguished.12
PCNSL carries mutated oncogenes (MYC, PAX5, PIM1, Rho/TTF) due to the process of aberrant SHM with evidence for ongoing SHM (Table S1).13 While this pattern of aberrant SHM is similar to systemic DLBCL, the mean mutation frequency of PCNSL is 2- to 5-fold higher, lending further support to the suggestion that the tumor cells or their precursors are characterized by a prolonged or even ongoing GC reaction.13,14
One study established a significant correlation between deletions in 6q and shorter survival.10 In 6q, the PRDM1 gene may function as a tumor suppressor gene at least in a fraction of PCNSL in a manner similar to activated B cell (ABC)–DLBCL (Table S1).15 Deleterious splice site and frameshift mutations with abrogation of PRDM1 protein expression may contribute to lymphomagenesis by impairing terminal B-cell differentiation.
Gene inactivation by DNA methylation may also be involved in malignant transformation. Methylation of DAPK or MGMT in PCNSL was associated with loss of protein expression.16 Inactivation of CDKN2A (p14ARF and p16INK4a) was attributed to DNA methylation or homozygous deletion.17,18 Hypermethylation of the reduced folate carrier (RFC) gene may be prognostically significant in PCNSL.19
The observation that PCNSL shares characteristics with systemic DLBCL of both the ABC (IGM expression, lack of CSR, activation of the NF-κB pathway) and the GC B-cell (GCB) subtype (high IG gene mutation frequency with ongoing SHM, BCL6 expression) raises the question whether PCNSL corresponds to ABC- or GCB-DLBCL or constitutes a separate entity. In this context it should be emphasized that the ABC/GCB classification was developed for systemic DLBCL and not for DLBCL of the CNS. The answer may be clinically relevant, because extracerebral ABC- and GCB-DLBCL differ in clinical outcome.20
So far, 3 studies on GEP in PCNSL confined to 21, 13, and 23 patients, respectively, have been published.3,21,22 The number of PCNSL cases suitable for GEP is limited due to the tiny size of most stereotactic biopsies. Two of these studies concurrently concluded that PCNSL is distributed along the spectrum of systemic DLBCL including the ABC, the GCB, and the non-ABC/non-GCB subtype indicating molecular heterogeneity of PCNSL.3,21 The third study did not address this particular question.22
Overall, the 3 GEP studies published so far lack a uniform message on PCNSL biology. Tun et al22 contrasted PCNSL with non-CNS DLBCL and proposed a CNS signature specific for tumor cells of PCNSL with a differential expression of extracellular matrix- and adhesion-related pathways. Among the most significantly up-regulated genes in PCNSL were SPP1, TF, DDR1, TUBB2B, SERPINA3, S100b, and CA2. Rubenstein et al21 defined features of gene expression in PCNSL that are most distinct from systemic DLBCL. More than 460 expressed sequence tags were differentially expressed between PCNSL and nodal lymphomas with a high expression of MYC, PIM-1, and IL-4–induced genes including XBP-1 in PCNSL. Thus, both studies propose that PCNSL shows a specific CNS signature, which allows distinction from systemic DLBCL. However, there is virtually no overlap between the genes described as most differentially expressed between PCNSL and nodal DLBCL by Rubenstein and colleagues (Table S121 ) and the genes with at least 2-fold different expression between PCNSL and non-CNS DLBCL described by Tun and colleagues (Table S122 ). Our group also detected several genes differentially expressed between PCNSL and systemic DLBCL, including IGM, FN, SERPINA3, SPP1, TF, and HBA13 . Moreover, application of Tun et al's algorithm to our raw data and vice versa yielded similar lists of genes differentially expressed between PCNSL and systemic DLBCL.22 Nevertheless, interpretation of the results is quite different. PCNSL biopsies generally harbor a mixture of tumor-derived as well as brain-derived signals, which is due to the characteristic growth pattern of the tumor cells intimately intermingled with the brain parenchyma. Therefore, we wondered whether the differences identified by profiling PCNSL and systemic DLBCL samples are indeed attributable to tumor cells or might also be caused by differences in the organ-specific microenvironment. To this end, we aimed at eliminating the background signature derived from non-neoplastic CNS cells. Supervised analysis comparing GEP from normal CNS samples with normal and neoplastic B-cell samples identified 476 genes that were more highly expressed (z-score ≤ −1.8) in normal CNS. Elimination of the genes from this “CNS signature” revealed 2 clusters of genes differentially expressed between PCNSL and extracerebral DLBCL. The cluster containing the genes with higher expression in PCNSL compared with systemic DLBCL included predominantly housekeeping genes and genes encoding ribosomal proteins as well as SERPINA3, FN, and IGM. As shown by immunohistochemistry, SERPINA3 as well as TF, FN, VCAM-1, and CA2 are expressed by resident CNS cell populations, but not by the tumor cells. Thus, although all 3 GEP studies identified genes differentially expressed between PCNSL and non-CNS DLBCL, different conclusions were drawn with respect to a PCNSL-specific GEP different from non-CNS DLBCL. These divergent interpretations may be explained by (1) different platforms used for GEP, (2) different algorithms applied, (3) different methods to eliminate the background signature of the CNS, (4) the low number of cases suitable for GEP, and (5) a sample-induced bias (open resection vs stereotactic biopsies).
Furthermore, when interpreting GEP data in PCNSL, one should consider that the scenario in PCNSL is even more complex: the infiltration of the brain, which under physiologic conditions is characterized by an immunologically down-regulated phenotype by the malignant B cells, causes prominent reactive changes in resident brain-cell populations. These also modify the overall GEP but cannot be distinguished from tumor-derived signals. This is illustrated by the observation of an up-regulation of SERPINA3 in PCNSL compared with systemic DLBCL, which is detected even after elimination of the genes most significantly expressed in the normal brain.3 Further morphologic studies attributed SERPINA3 to macrophages/microglia, which have been activated in response to tumor infiltration of the brain but not to the malignant B cells.3 Ideally, the usage of purified tumor B cells would circumvent these problems and may yield a PCNSL-specific GEP.
Microenvironment
The most intriguing issue relates to the question of the selective manifestation of PCNSL in the CNS. In exceptional cases only, extracerebral relapse has been observed. It is still unresolved—and not yet adequately amenable to investigation—whether B cells enter the CNS as nonmalignant or malignant B cells (eg, during [pathogen-induced] inflammation). Efforts to identify a specific pattern of molecules and receptors involved in homing to the CNS (cell-adhesion molecules, chemokines) unequivocally failed.23 CXCR4, CXCL12, CXCR5, CXCL13, and CCR7 were expressed by the tumor cells, while cerebral endothelial cells expressed CXCL12 and CXCL13, and reactive astrocytes and activated microglia expressed CXCL12, CCR5, and CCR6 (Table S1).24,25 BAFF released by astrocytes may support the intracerebral survival of the BAFF-receptor expressing tumor B cells.26 This cell type–specific and complementary expression of chemokines and their receptors on tumor cells and resident cell populations may facilitate recruitment of B cells to the CNS, their intracerebral dissemination, and the specific interaction of tumor cells with CNS structures.
The investigation of the interaction of tumor cells with brain-cell populations is still largely restricted to morphology and does not (yet) allow a functional approach. In addition to astrocytes, microglia, and cerebral endothelium, there is evidence that neurons, oligodendrocytes, ependymal cells, and choroid plexus epithelium also have the capacity to participate in immune reactions. In this regard it is of note that genes characteristically expressed by oligodendroglia (ie, carbonic anhydrase and 2′,3′-cyclic nucleotide 3′ phosphodiesterase) were up-regulated in CNS versus non-CNS DLBCL.22 The contribution of all of these resident cell populations of the brain, which may also regulate each other, to the cross-talk between tumor cells as well as between CD4 and CD8 T cells, nonmalignant B cells, macrophages/microglia, which constitute the characteristic infiltrate, is unknown. It is tempting to speculate that the tumor cells of PCNSL may down-regulate the intracerebral immune response by anti-inflammatory cytokines such as IL-4 and IL-10, and thus may escape immune surveillance. The frequently observed loss of HLA-DQ, HLA-DR, and HLA-A due to homozygous or heterozygous 6p21.3 deletion (Table S1) may facilitate tumor-cell survival in organs characterized by a physiologically down-regulated immunophenotype.27-29 Such loss of the HLA region has been suggested to be a prerequisite of lymphomas of immunoprivileged organs contributing to escape from the immune response.27-29 In this regard, the observation of a patient with PCNSL and testicular relapse 8 years thereafter is of note; while both tumors carried identical IG gene rearrangements, the progressive loss of HLA expression on the tumor cells may have facilitated immune escape.30
A further unexplained issue relates to the preferential usage of the IGHV4-34 gene segment in PCNSL.4,5 It is still unknown whether the microenvironment of the CNS favors the expansion of lymphomas bearing particular IG genes. The high frequency of IGHV4-34 recombination (Table S1) suggests a functional role of IG encoded by this gene in PCNSL development. Antigens including viruses with a high affinity to the CNS and/or with the propensity of persistence within the brain (eg, herpes virus and polyomaviruses) may preferentially stimulate the expansion and intracerebral persistence of B cells, which produce antibodies encoded by the IGHV4-34 gene segment.5 Interestingly, the IGHV4-34 gene segment has been implicated in EBV infection. However, in immunocompetent patients, PCNSL is usually EBV-negative. So far, EBV, HHV-6, HHV-8, and SV-40 have been excluded as potential antigens.1,31-33 Alternatively, a superantigen-fostered expansion of IGHV4-34 encoded IG, which has been described as exhibiting autoreactive properties, may underlie its biased usage.4,5
Furthermore, the observation of ongoing SHM in the CNS,4,5,13 an extranodal organ, raises the question whether reactive T cells and antigen presenting cells together with an antigen remaining to be identified may create a microenvironment allowing extranodal SHM. While it cannot be excluded with certainty that transformation of the B cells may have occurred outside the CNS while the clone continued to acquire somatic mutations before leaving the GC, it is unlikely that several different tumor clones leave the GC of secondary lymphatic organs simultaneously and selectively home to the CNS. This is further illustrated by the observation of a patient with PCNSL who relapsed in the CNS 2 years after initial manifestation. IG gene analysis revealed that both tumors were derived from a common ancestor and that clonal evolution instead of subclonal selection may underlie relapse.34
Conclusions and future perspectives
Intense scientific effort has yielded answers with respect to the 3 issues raised: a GC exit B cell has been identified as the nonmalignant counterpart of the tumor cells. Important mechanisms involved in lymphomagenesis have been identified in PCNSL (Figure 1). Translocation of the BCL6 and the IG genes, amplification of 18q21, deletion of 6p21 and 6q, activation of the NF-kB complex, aberrant SHM of the oncogenes MYC, PIM1, PAX5, Rho/TTF, as well as mutations of the PRDM1 gene may contribute to malignant transformation. An issue still requiring more detailed investigation relates to GEP. So far, data on epigenetics are restricted to selected genes requiring a genome-wide approach. Normal brain tissue as control is mandatory for both approaches.
Model of pathogenesis for PCNSL. Schematic presentation of several pathways involved in the pathogenesis of PCNSL. SHM, somatic hypermutation; ASHM, aberrant somatic hypermutation; CSR, class switch recombination.
Model of pathogenesis for PCNSL. Schematic presentation of several pathways involved in the pathogenesis of PCNSL. SHM, somatic hypermutation; ASHM, aberrant somatic hypermutation; CSR, class switch recombination.
The future investigation of the biology and nature of PCNSL in the setting of large clinical trials to allow correlation with clinical data and response to therapeutic regimens will be key to providing statistically significant conclusions and identifying prognostically and therapeutically relevant biomarkers. Important challenges to be addressed include the identification of the impact of the CNS microenvironment, the precise definition of the reactions of the various brain-cell populations and their cross-talk with tumor cells and leukocytes of the associated inflammatory infiltrate, and the resulting effect on the antitumor immune response. This may provide clues to our understanding of PCNSL and foster the development of specific therapeutic regimens to improve the still poor prognosis.
The online version of this article contains a data supplement.
Acknowledgments
The authors' own research on PCNSL is supported by the Deutsche Krebshilfe/Dr Mildred Scheel Stiftung für Krebsforschung (Grant 107733) and the Deutsche Forschungsgemeinschaft (De 485/9-1).
Authorship
Contribution: All authors contributed to writing as well as to data analysis.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Martina Deckert, MD, Department of Neuropathology, University Hospital of Cologne, Kerpener Str 62, D-50924 Köln, Germany; e-mail: neuropatho@uni-koeln.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal