As is the case in most human cancers, loss of function or deletion of the p53 tumor suppressor gene signals bad news in chronic lymphocytic leukemia (CLL).1 The reasons for this are complex, but clearly the majority of current treatments induce apoptosis via a p53-dependent pathway. Although p53 has been traditionally considered a transcription factor, there is growing evidence that it also causes extranuclear effects that can induce powerful cellular responses independent of de novo gene transcription.2 In this issue of Blood, Steele et al present compelling evidence that CLL cells preferentially employ a transcription-independent mechanism of apoptosis. They demonstrate that treatment-induced p53 is predominantly found in the mitochondrial fraction of cell extracts and is associated with the antiapoptotic protein Bcl-2. Furthermore, they show that the p53 transcription-blocking agent pifithrin α can enhance chlorambucil- and fludarabine-mediated apoptosis. This result is somewhat counterintuitive, but the authors conclude that the net effect of p53-induced transcription is the blockade of a transcription-independent apoptotic pathway. Therefore, selective inhibition of p53-mediated transcription by pifithrin α results in increased cell killing.
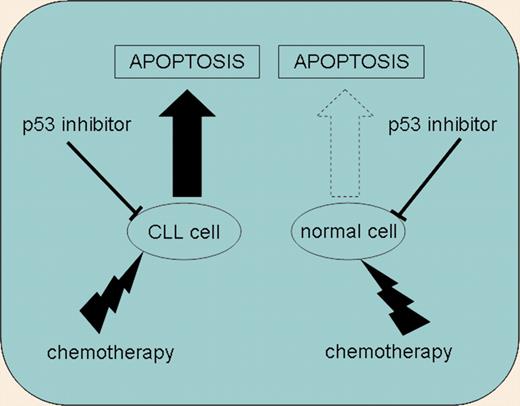
The combination of chemotherapy with p53 inhibitors enhanced CLL-cell apoptosis. In contrast, normal T cells were resistant to this combination of agents.
The combination of chemotherapy with p53 inhibitors enhanced CLL-cell apoptosis. In contrast, normal T cells were resistant to this combination of agents.
These results are intriguing but defy simple interpretation. For instance, it is not clear whether the effects of pifithrin α are truly the consequence of blocked transcription. It may be tempting to simplistically consider that pifithrin α blocks the transcription of the ubiquitin ligase MDM2, thereby stabilizing p53 and preventing its degradation.3 Indeed, this paper presents evidence for pifithrin α–mediated inhibition of MDM2. However, p53 is capable of inducing/repressing hundreds of genes, so a painstaking dissection of global gene expression profiles induced by pifithrin α in CLL would seem necessary. This approach may yield a list of “likely suspects” that can be specifically inhibited using the gene silencing methodologies that are now available for the manipulation of CLL cells. Furthermore, a number of alternative explanations beyond transcriptional repression are possible. Pifithrin α may simply prevent p53 nuclear import, thereby sequestering it in the cytoplasm where it is free to interact with Bcl-2 family proteins. In this regard, the coimmunoprecipitation of Bcl-2 and p53 from CLL cell extracts presented here is intriguing. Can cytoplasmic p53 displace Bax from a Bcl-2/Bax complex, thereby triggering the Bax conformational change observed in this study? Alternatively, it has recently been suggested that p53 can even act directly on the mitochondrial permeability transition pore complex in order to induce apoptosis.4 All of these possibilities can be tested experimentally, and so it seems inevitable that further revelations will be forthcoming in the near future.
This work has raised a number of very interesting biologic questions, but the key clinical question is, can we exploit p53 transcription blockers to augment current chemotherapeutics? The answer at the moment is a guarded “maybe.” Promisingly, pifithrin α has been shown to be relatively nontoxic to normal tissue in mouse models,5 and this present study shows little evidence of pifithrin α–mediated apoptosis in normal human T cells. However, additional studies involving the coadministration of standard chemo-therapies are clearly warranted. Another concern is that this strategy may only be effective when the CLL cells have a functional p53 pathway. p53 dysfunction is much more prevalent in advanced-stage and drug-resistant patients, so the clinical utility of this approach may be limited in this context.
Despite the unresolved questions and the probable clinical caveats, this paper provides fascinating new insights into the biological machinery of CLL cells. It seems likely that we will be able to exploit this new knowledge in the future to develop more effective treatments for this common but as yet incurable disease.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal