Abstract
Background: Although some studies have validated the 2001 WHO classification of acute myeloid leukemia (AML), including the importance of multilineage dysplasia, others have suggested that multilineage dysplasia correlates with unfavorable cytogenetics but has no independent impact on prognosis. In 2008, the revised WHO classification system has expanded this category into “AML with myelodysplasia-related changes” (AML-MRC) that now includes 1) AML arising from myelodysplastic syndrome (MDS), 2) AML with MDS-related cytogenetic abnormalities, and 3) AML with multilineage dysplasia. An individual case may fall into this category by meeting any of the criteria. The goal of the current study is to clinically characterize this newly defined AML-MRC subgroup.
Methods: One-hundred consecutive AML patients diagnosed at Stanford University Hospital between 2005 and 2007 with adequate material for mutation analysis were studied. Cases were classified using the 2008 WHO criteria. Diagnostic cytogenetic findings were reviewed and patients were stratified into risk groups using Southwest Oncology Group criteria. Available flow cytometry immunophenotyping results were reviewed and all samples were tested for NPM, FLT3 (ITD and D835) and CEBPA mutations. Clinical parameters including hemogram data at time of diagnosis were reviewed. Clinical follow-up including overall survival (OS), progression free survival (PFS) and complete remission (CR) rates were retrospectively determined. Kaplan-Meier methods and univariate and multivariate Cox proportional hazards regression analysis were used to compare the clinical data.
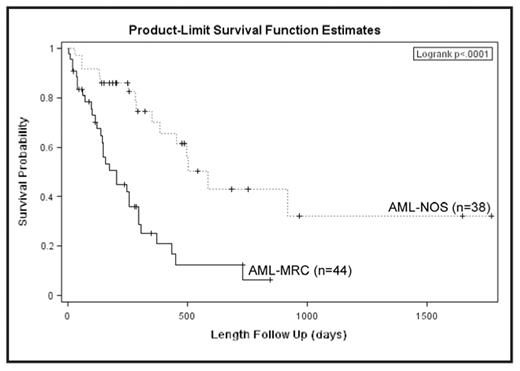
Results: The cases included 57 males and 43 females with a median age of 56 (range 17–81). Cytogenetic risk-group stratification resulted in 9 patients with favorable, 65 with intermediate and 19 with unfavorable risk status. Using the 2008 WHO criteria, there were 48 AML-MRC, 40 AML not otherwise specified (AML-NOS), 9 AML with either t(8;21), inv(16) or t(15;17), and 3 therapy related AMLs. Overall, 26 patients had a NPM1 mutation (16 of which were FLT3 mutated), 25 had FLT3-ITD, 8 had FLT3-D835 and 9 had a CEBPA mutation (3 of which were FLT3 mutated). Compared to AML-NOS, patients with AML-MRC were significantly older (59 vs 51 years, p=0.014) and presented with lower hemoglobin (9 vs 11.2 g/dL, p=0.044), lower platelets (47 vs 54 K/uL, p=0.059), unfavorable cytogenetics (14/46 vs 3/36, p=0.014) and exhibited a decreased frequency of CEBPA mutation (0/46 vs 7/40, p=0.001) as compared to AML-NOS. Based on the flow cytometry immunophenotyping, the blasts from patients with AML-MRC more frequently expressed CD14 compared to AML-NOS (10/46 vs 4/36, p=0.048). Clinical outcome data showed that patients with AML-MRC had a significantly worse OS, PFS and CR compared to AML-NOS (Figure, all p<0.0001). Even after excluding the 14 patients with unfavorable cytogenetics from the AML-MRC group, the remaining patients with AML-MRC (defined solely by the presence of multilineage dysplasia) had worse outcomes compared to all AML-NOS patients (OS, p=0.013; PFS, p=0.012; CR, p=0.0076). Among 65 patients with intermediate risk cytogenetics, the outcome difference between the AML-MRC and AML-NOS groups remained significant (OS, p=0.0292; PFS, p=0.0232), also indicating prognostic significance of multilineage dysplasia. Within the AML-MRC group, univariate analysis showed that low platelets (<20,000/mm3), FLT3-D835 mutation and MDS-related cytogenetics correlated with OS (p=0.0456, p=0.0265, p=0.002 respectively) and PFS (p=0.0478, p=0.0626, p=0.001). A multivariate Cox proportional hazard analysis, performed on the entire group, identified unfavorable cytogenetic risk group, advanced age (> 60), FLT3-ITD and AML-MRC status as significant predictors of worse OS with the following respective hazard ratios: 2.82 (95% CI, 1.52–5.26), 2.11 (1.01–4.42), 1.98 (1.01–3.90), 1.92 (1.01–3.65).
Conclusion: The newly defined WHO category of AML-MRC exhibits a significantly worse clinical outcome compared to AML-NOS and is predictive of worse overall survival in the multivariate analysis of AML patients, independent of age or cytogenetic risk group. These findings support the clinical, morphologic and cytogenetic criteria for this 2008 WHO AML category.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal