Abstract
Background: Allogeneic hematopoietic stem cell transplantation (allo SCT) has two potential advantages over autologous SCT: a tumor-free graft and graft-versus-myeloma (GVM) effect. Allo SCT’s potential to induce long term remission has, however, been offset by high rates of transplant-related non-relapse mortality (TRM). Reduced-intensity conditioning (RIC) regimens for allo SCT are associated with lower TRM without compromising the GVM effect.
Methods: We retrospectively analyzed our experience in 69 patients (30 females and 39 males) with heavily pretreated, relapsed myeloma, who received allo SCT at our institution between1985 and 2007. Eighteen patients received myeloablative regimens (MA), while 51 received RIC regimens. MA regimens were TBI-based in 5 patients, high-dose busulfan-containing in 6 patients and high-dose melphalan containing (180–200 mg/m2) in 7 patients. RIC regimens were a combination of fludarabine (90–120 mg/m2) and melphalan (100–140 mg/m2). Median age of patients at allo SCT in both groups was 51 years. Median interval from diagnosis to allo SCT was 35.4 months in MA group, and 34.2 months in RIC group. Eight (44%) patients in MA group and 36 (70%) patients in RIC group had prior autologous SCT. Six patients (33%) in the MA group and 11 (25%) in the RIC group received allo SCT from unrelated donors (p=0.3). Median number of prior treatment regimens were 5 (range 1–10) in both groups. Stem cell source was peripheral blood in 3 patients in MA group and 41 patients in the RIC group (p=0.0001).
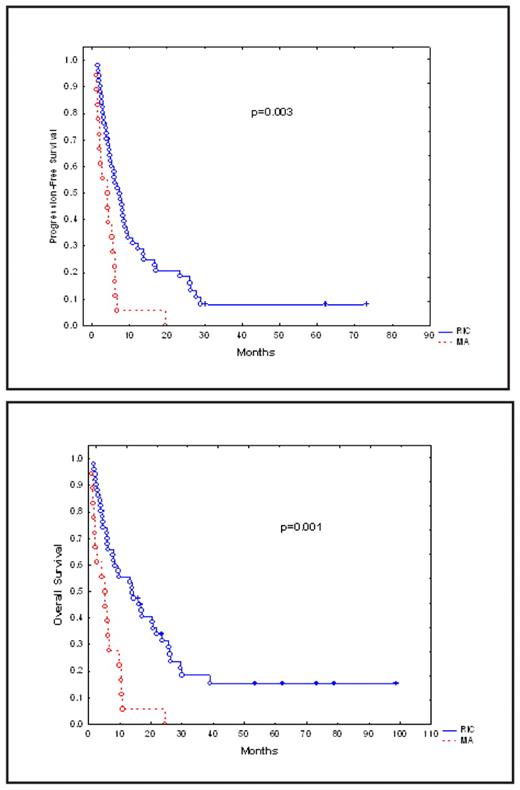
Results: Median follow-up in surviving patients was 27 months (3–98). All patients achieved engraftment. Cumulative TRM at 1 year was 56% in the MA group and 25% in the RIC group (p=0.03). Overall response rates in evaluable patients were 69% (CR=15%, PR= 54%) in MA group, and 79% (CR=23%, PR=56%) in the RIC group (p=0.47). Disease progression at 2 years was seen in 8 patients (44%) in the MA group and 25 patients (49%) in the RIC group (p=0.78). Median progression-free survival (PFS) in MA vs. RIC groups was 4.1 and 6.8 months, respectively (p=0.003) and median overall survival (OS) ) in MA vs. RIC group was 5.3 and 13.9 months, respectively (p=0.001). Cumulative Incidence of grade II–IV acute graft-vs.-host (GVHD) in MA vs. RIC groups disease was 33 vs. 27% (p=0.76); cumulative incidence of chronic GVHD in MA vs. RIC group was 54% vs. 47% (p=0.41) in evaluable patients. At the time of this analysis, 13 patients (25%) were still alive in RIC group, 7 of whom (14%) were in remission for up to 6 years post allo SCT. The most common causes of death were recurrent disease (30 patients; 43%), acute or chronic GVHD (16 patients; 23%) and opportunistic infections (5 patients: 7%).
Conclusions: Allo SCT after RIC regimens is associated with longer PFS and OS and lower TRM. There was no increase in the risk of relapse, or acute or chronic GVHD. These regimens can safely replace MA regimens and may offer greater benefit if utilized earlier in the course of disease.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal