Abstract
Background: The 2001 WHO classification of myeloid neoplasms distinguished 2 forms of MDS associated with >=15% ring sideroblasts and <5% marrow blasts: refractory cytopenia with multilineage dysplasia and with ring sideroblasts (RCMD-RS) vs. refractory anemia with ring siderblasts (RARS, erythroid-restricted dysplasia). However, the real prognostic value of separating RCMD-RS from RCMD with <15% ring sideroblasts and from RARS is uncertain, and the WHO has proposed merging RCMD-RS and RCMD in the 2008 classification revision. Furthermore, the WHO-based Prognostic Scoring System (WPSS), proposed by Malcovati and colleagues in 2005 as a dynamic system that overcomes some of the limitations of the 1997 International Prognostic Scoring System (IPSS), has undergone limited independent external validation to date and its applicability to sideroblastic MDS in particular is unclear. We assessed the validity of the 2008 WHO reclassification and the WPSS for MDS cases associated with >=15% ring sideroblasts and a normal blast proportion.
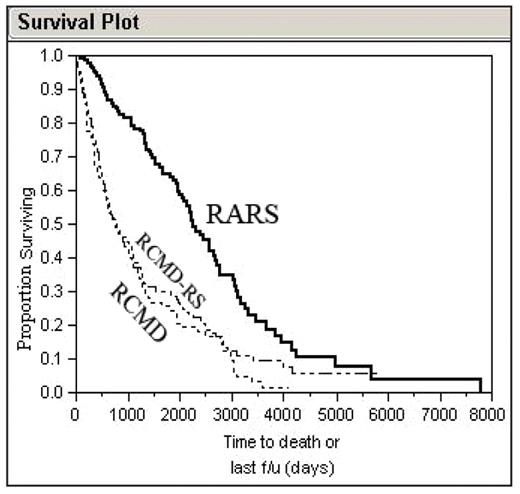
Methods: We reviewed WPSS and IPSS component parameters at diagnosis and the clinical outcomes of 465 patients (68% males, median age 72) evaluated at our institution over a 13-year period: 140 with RARS, 114 with RCMD-RS, and 211 with RCMD. Patients were assigned a WPSS score and risk category (very low-risk group=0 points; low=1; intermediate=2, high=3 or 4) by summing 3 subscores: 2001 WHO classification (0 for RARS, 1 point for RCMD or RCMD-RS), IPSS cytogenetic risk group (0=good, 1=indeterminate, 2=poor), and red cell transfusion dependence (0=no, 1=yes). Survival was assessed by Kaplan-Meier estimates, and prognostic factors examined by proportional hazards analysis.
Results: The median time until death or last followup was 26 months, and 70% of patients were known to have died. The median survival by WHO MDS subtype was 75 months for RARS, 25 months for RCMD-RS, and 26 months for RCMD (Log-Rank p<0.0001 for RARS vs. either RCMD-RS or RCMD; p=0.60 for RCMD vs. RCMD-RS ). Both the WPSS and IPSS predicted overall survival in patients with ring sideroblasts. Median survival for the patients grouped by WPSS risk category was 89 months for very low risk (n=95), 41 for low risk (n=198), 31 for intermediate risk (n=82), and 11 for high risk (n=91) (p<0.0001, except for low risk vs. intermediate risk, p=0.31). (Very high risk WPSS scores cannot be achieved without excess marrow blasts, and such patients were excluded from this analysis.) Median survival by IPSS was 73 months for low-risk, 33 months for intermediate-1, and 8 months for intermediate 2 (p<0.0001). The IPSS’ predictive power was unchanged if patients with secondary MDS were included or excluded (the IPSS was based on a review of 816 patients with apparently de novo MDS).
Conclusions: These data support the WHO’s proposal to merge RCMD and RCMD-RS, and suggest that the adverse prognostic significance of multilineage dysplasia renders the presence of ring sideroblasts unimportant. The WPSS is a valid prognostic tool in patients with MDS associated with ring sideroblasts, but in this subgroup both the WPSS and IPSS stratify patients into 3 risk groups, and the WPSS does not offer additional value over the IPSS.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal