Abstract
Background: Leukocytosis has recently been implicated as an adverse prognostic feature for thrombosis in both ET and PV. Such an association would be therapeutically most relevant in the context of “low-risk” disease. In the current study, we sought to clarify the relationship between leukocytosis at diagnosis and the subsequent occurrence of either arterial or venous thrombosis, in “low-risk” patients with ET or PV.
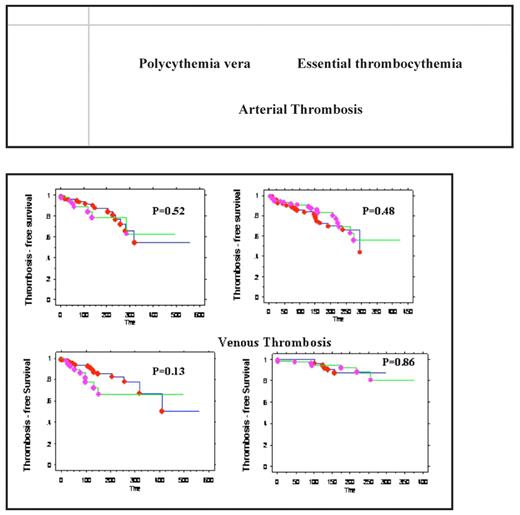
Methods: Data was abstracted from the medical records of a consecutive cohort of patients with WHO-defined ET or PV seen at the Mayo Clinic. Low-risk disease was defined by the absence of both thrombosis history and age 3 60 years. Cox proportional hazards model was utilized to determine the impact of clinical and laboratory variables on thrombosis-free survival (TFS). Arterial- or venous-specific TFS curves were constructed by Kaplan-Meier method.
Results:i) Patient characteristics and outcome A total of 407 “low-risk” patients were studied; 153 had PV (median age 48 years; females 43%) and 254 ET (median age 42 years; females 71%). A total of 46 thrombotic events (22 arterial and 24 venous) were recorded in 41 (27%) patients with PV during a median follow up of 130 months (range 2–562 months). The corresponding figures in ET were 54 total thrombotic events (41 arterial and 14 venous) in 47 (19%) patients at a median follow up of 104 months (range 0.25–424 months). Cytoreductive therapy was avoided in the presence of < 1000 x 109/L platelet count but, at the discretion of the treating physician, some patients with higher platelet counts received prophylactic cytoreductive therapy. ii) Correlation between leukocytosis and thrombosis A leukocyte count of 3 15 x 109/L at diagnosis was documented in 42 (27%) patients with PV and 21 (8%) patients with ET; 102 patients (40%) with ET had > 9.4 x 109/L leukocyte count. Leukocyte count considered as either a continuous or categorical variable (using cutoff levels of 15 x 109/L for PV and either 15 x 109/L or 9.4 x 109/L for ET) was not significantly associated with either arterial or venous thrombosis (Figure 1). iii) Correlation between other risk factors and thrombosis In univariate analysis, presence of the JAK2V617F was significantly associated with arterial thrombosis in ET (p=0.049) but significance was lost during multivariable analysis that included age as a covariate. Only advanced age was found to be significantly associated with arterial thrombosis in PV (p=0.04) and higher hemoglobin level with venous thrombosis in ET (p<0.0001).
Conclusion: The current study does not identify leukocyte count at diagnosis as a marker of increased thrombosis risk in low-risk patients with either ET or PV. Instead, the study found an association between arterial thrombosis and advanced age in PV and venous thrombosis and higher hemoglobin level in ET.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal