Abstract
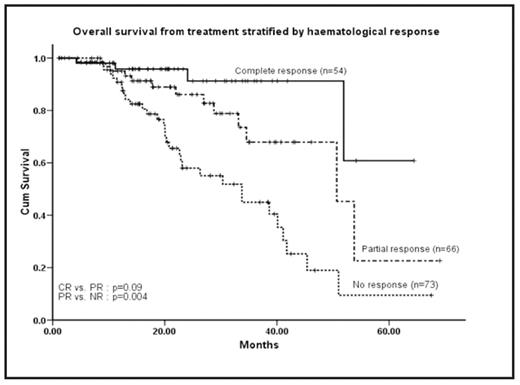
Risk-adapted oral regimen of cyclophosphamide, thalidomide, and dexamethasone (CTD) was previously reported by our group to be highly effective in patients with systemic AL amyloidosis. However, the numbers were small with limited long-term follow-up. We now report the use of this regimen in a much larger series of 202 patients with prolonged follow-up. All patients treated with CTD between 2002 – 2008 were identified from the database of the UK National Amyloidosis Centre, London. Organ involvement and response was assessed according to international consensus criteria (Gertz et al, 2005). The course of amyloid deposits was quantified by serial I123 labelled serum amyloid P component (SAP) scintigraphy and has been reported separately. Survival was assessed by the method of Kaplan-Meier and multivariate analysis was by Cox regression. Males accounted for 58% of patients, and the light chain excess was predominately lambda (72%). Renal involvement was seen in 150 patients (75%), cardiac in 95 (47%), hepatic in 36 (15%), peripheral and/or autonomic nerve involvement in 30 (15%), pulmonary in 4 (2%), gastrointestinal tract in 15 (7%), and soft tissue in 56 (28%). Abnormalities in SAP scintigraphy were seen in 170 patients (84%). Median number of organs involved was 2. Full dose CTD was administered to 139 (69%) patients while 63 (31%) received the dose attenuated regimen. 123 (61%) patients received this chemotherapy as first line treatment. The median number of cycles delivered was 5 (range 1–15). A hematologic response occurred in 120 (62%) of 193 evaluable patients. Complete responses (CR) were seen in 49 patients (25%), near complete response (nCR) in 5 (3%) and partial responses (PR) in 66 (34%) cases. 67% of newly diagnosed and 54% of relapsed cases responded. There was no significant difference in the CR rates between newly diagnosed and relapsed cases (29 vs. 27%). Organ responses were observed in 50/120 (42%) patients - renal in 40/87 patients (46%), hepatic in 6/21 (29%), nerve in 2/16 (13%), cardiac in 4/53 (8%), gastrointestinal in 2/8 (25%), and soft tissue involvement in 7/37 (19%). Improvements on SAP scintigraphy were noted in 42 patients (21%) post-treatment. The median follow-up was 20 months (range 1 – 69 months). Median estimated overall survival (OS) from commencement of treatment and from diagnosis was 42 months and 83 months respectively. At 60 months, the median survival has not been reached for patients achieving a CR, 50 months for PR and 33 months for non-responders. There was no significant difference in OS from commencement of treatment if the patient was previously treated or not (41 vs 45 months respectively, p = 0.75). Among 120 responders, 51 patients (43%) relapsed. Median estimated time to clonal relapse (PFS) was 32 months. The PFS was 33 months for patients without prior treatment and 25 months for those treated for relapsed disease (p = 0.69). Toxicity of any grade was reported by 171 (85%) patients and was ≥ grade 3 in 21%. The commonest severe toxicity was fluid retention. Treatment-related mortality was 3%. In conclusion, this large study confirms that risk adapted CTD has comparable efficacy with other reported oral regimes, namely melphalan-dexamethasone, for the treatment of AL amyloidosis. High rates and durable clonal responses were frequently accompanied by organ responses. Treatment related mortality was low. CTD in an effective regimen for the treatment of patients with newly diagnosed AL amyloidosis and those whose clonal dyscrasias have relapsed. It has the advantages of being stem cell sparing and not requiring dose adjustment in cases of advanced renal failure.
Disclosures: Off Label Use: Thalidomide in the treatment of plasma cell dyscrasiae.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal