Abstract
Relapse is the major cause of treatment failure after HSCT for relapsed AML. Maintenance therapy may provide an “adjuvant’ support for the allogeneic graft-versus-leukemia effect, decreasing the likelihood of recurrence. AZA is a DNA methyltransferase inhibitor that induces DNA hypomethylation, leading to leukemic cell differentiation and potentially increased tumor immunogenicity. FDA approved doses are however unlikely to be tolerated due to myelosuppression. We hypothesized that AZA will reduce relapse rates, and designed a phase I clinical trial to determine the safest dose and schedule combination.
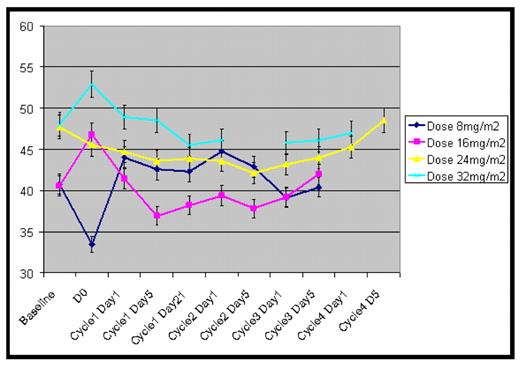
Methods. Eligible were patients (pts) with AML/MDS not in 1st complete remission (CR), not candidates for ablative regimens due to age or comorbidities. Conditioning regimen was gemtuzumab ozogamicin 2 mg/m2, fludarabine 120mg/m2, and melphalan 140mg/ m2. GVHD prophylaxis was tacrolimus/mini-methotrexate (ATG in unrelated donor HSCT). We investigated 4 AZA doses: 8, 16, 24 and 32 mg/m2 SQ daily x 5 starting on day +42, given for 1–4 28-day cycles (schedule). An outcome-adaptive method was used to determine dose and schedule (number of cycles): pts were assigned to a dose/ schedule combination on the basis of the data (organ/hematologic toxicity) from all pts treated previously in the trial. Pts in CR on transplant day+30, with donor chimerism, no grade III/IV GVHD, platelet >10,000/mm3 and ANC >500/mm3 were eligible to receive AZA. Methylation status of long interspersed nuclear elements (LINE) was analyzed by pyrosequencing as a surrogate marker of global DNA methylation (figure).
Results. 80 pts were transplanted; 44 (56%) were eligible to receive AZA: 2 refused; 42 pts. (4 too early) received it. Table shows pts characteristics. 88 cycles were delivered at 8 (n=7), 16 (n=5), 24 (n=21) and 32 mg/m2 (n=9). AZA-associated/possibly associated toxicities were grade (gd) I/II or III thrombocytopenia (n=5; n=2), gd I nausea (n=5), gd II fatigue (n=2), gd III transaminase elevation (n=1, AZA + posaconazole), conjunctival erythema (n=1), pruritus (n=1), gd I confusion (n=2), retina hemorrhage (possibly pre-existing), gd II creatinine elevation (n=1), oral ulcers (n=1), papilledema (n=1), and pulmonary hemorrhage (n=1; second HSCT, fungal pneumonia/hepatic VOD during the 1st AZA cycle, evolving with thrombocytopenia/bleeding). Reversible thrombocytopenia was more frequent at 32 mg/m2. Infections: bacteremia, n=5; respiratory, n=6; parainfluenza, n=2, CMV reactivation, n=6. Most pts were 100% donor chimeras at the start of AZA. AZA did not affect GVHD incidence (table). 10 pts have relapsed, 3 while on AZA 16 or 24 mg/m2. Median follow-up is 13 months (3–31; n=26). 12 pts have died, 8 of recurrence, 2 of GVHD, 1 of pneumonia and 1 of unknown causes. Day +100 non-relapse mortality was 6 %; 4 pts died within the first 100 days post HSCT due to relapse (n=2), pneumonia (n=1), and GVHD (n=1). Actuarial 1-year event-free and overall survival is 58% and 72%. No dose was found to significantly affect global methylation (gene specific methylation studies are ongoing). The trial has reached the dose 32 mg/m2 and the projected maximum number of cycles. Thrombocytopenia prevented escalation to the next level (40 mg/m2).
| Variables . | N (%) (range) . |
|---|---|
| Age: median (range) | 60 (24–67) |
| Median number of previous chemotherapy regimens | 2 (0 – 5) |
| Cytogenetics | |
| Good / Intermediate / bad | 1 (3%)/ 22 (58%)/ 15(39%) |
| Previous Allogeneic SCT | 7 (18%) |
| Disease status at transplant | |
| CR2/CR3 | 8/2 (26,3%) |
| First Relapse/induction failure | 12/13 (66,7%) |
| ≥ second/third relapse | 3 (7%) |
| Charlson Comorbidity Index score | |
| 0 / 1 | 4 (10,5%) / 4 (10,5%) |
| 2 / 3 | 5 (13,2%) / 7 (18,4%) |
| >3 | 18 (47.4%) |
| Donor type | |
| Sibling/unrelated | 23/15 (58/42%) |
| Cells Source:PB/BM | 73% / 27% |
| Grade II/III Acute GVHD | |
| Grade 2 / grade 3 | 6 (16,7%) / 4 (11%) |
| Chronic GVHD | 14 (46,5%) |
| Variables . | N (%) (range) . |
|---|---|
| Age: median (range) | 60 (24–67) |
| Median number of previous chemotherapy regimens | 2 (0 – 5) |
| Cytogenetics | |
| Good / Intermediate / bad | 1 (3%)/ 22 (58%)/ 15(39%) |
| Previous Allogeneic SCT | 7 (18%) |
| Disease status at transplant | |
| CR2/CR3 | 8/2 (26,3%) |
| First Relapse/induction failure | 12/13 (66,7%) |
| ≥ second/third relapse | 3 (7%) |
| Charlson Comorbidity Index score | |
| 0 / 1 | 4 (10,5%) / 4 (10,5%) |
| 2 / 3 | 5 (13,2%) / 7 (18,4%) |
| >3 | 18 (47.4%) |
| Donor type | |
| Sibling/unrelated | 23/15 (58/42%) |
| Cells Source:PB/BM | 73% / 27% |
| Grade II/III Acute GVHD | |
| Grade 2 / grade 3 | 6 (16,7%) / 4 (11%) |
| Chronic GVHD | 14 (46,5%) |
Conclusion. AZA 32 mg/m2 is safe and can be administered for at least 4 cycles to heavily pre-treated pts. with comorbidities. The safety profile indicates that longer periods of administration should be investigated. We will initiate a randomized, controlled study of AZA for one year versus best standard of care (no maintenance therapy) for similarly highrisk patients with AML/MDS.
Disclosures: De Lima:Pharmion : Research Funding.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal