There is increasing evidence to suggest that the Wnt signaling pathway plays a critical role in the pathogenesis of myeloma bone disease. In the present study, we determined whether increasing Wnt signaling within the bone marrow microenvironment in myeloma counteracts development of osteolytic bone disease. C57BL/KaLwRij mice were inoculated intravenously with murine 5TGM1 myeloma cells, resulting in tumor growth in bone and development of myeloma bone disease. Lithium chloride (LiCl) treatment activated Wnt signaling in osteoblasts, inhibited myeloma bone disease, and decreased tumor burden in bone, but increased tumor growth when 5TGM1 cells were inoculated subcutaneously. Abrogation of β-catenin activity and disruption of Wnt signaling in 5TGM1 cells by stable overexpression of a dominant-negative TCF4 prevented the LiCl-induced increase in subcutaneous growth but had no effect on LiCl-induced reduction in tumor burden within bone or on osteolysis in myeloma-bearing mice. Together, these data highlight the importance of the local microenvironment in the effect of Wnt signaling on the development of myeloma bone disease and demonstrate that, despite a direct effect to increase tumor growth at extraosseous sites, increasing Wnt signaling in the bone marrow microenvironment can prevent the development of myeloma bone disease and inhibit myeloma growth within bone in vivo.
Introduction
There have been many advances in our understanding of the biology of multiple myeloma and the associated bone disease, yet a number of critical questions remain unanswered and myeloma remains an incurable malignancy. One such question, with important therapeutic implications, is the exact nature of myeloma bone disease—specifically the dysregulation of both osteoclastic bone resorption and osteoblastic bone formation. Histomorphometric studies have demonstrated that bone resorption is increased in patients with multiple myeloma, and for many years, the osteoclast was considered to be the primary mechanism involved in the development of myeloma bone disease.1,–3 Although early stages of multiple myeloma have been associated with an increase in osteoblast recruitment, a very marked impairment of bone formation due to reduced osteoblast number and activity is a common feature in later stages of the osteolytic bone disease.3,–5 This has been confirmed in recent studies that demonstrate that markers of bone formation are decreased in patients with multiple myeloma.6,7 Although the cellular and molecular mechanisms involved in this reduction of osteoblast activity are poorly understood, it is clear that the regulation of bone formation plays a critical role in the pathogenesis of myeloma bone disease and represents an important therapeutic target for the treatment of this destructive bone disease
The Wnt signaling pathway plays a key role in the regulation of bone mass, and there is increasing data to suggest a role for this pathway in the development of multiple myeloma.8 Human genetic bone diseases and in vivo mouse models provide strong evidence for the function of the Wnt signaling pathway in bone biology. Inactivating mutations in the gene for LRP5 result in osteoporosis-pseudoglioma syndrome in humans, whereas “gain of function” mutations in LRP5 are associated with a syndrome of hereditary high bone density.9,–11 Overexpression of β-catenin in osteoblasts has been demonstrated to induce a high bone mass phenotype.12 Transgenic mice overexpressing the soluble antagonist of Wnt, Dickkopf 1 (Dkk1), in osteoblasts develop severe osteopenia, whereas deletion of a single allele of Dkk1 caused an increase in bone mass.13,14 In multiple myeloma, patients have increased serum levels of Dkk1, which correlate with the presence of bone lesions.15 Serum taken from these patients was also demonstrated to inhibit osteoblast differentiation in vitro, and this inhibitory effect was found to be mediated by Dkk1. Furthermore, a recent study has demonstrated that inhibition of Dkk1 in a severe combined immunodeficient 11-rabbit (SCID-rab) model of myeloma reduced both osteolytic bone resorption and tumor burden.16 Myeloma cells have also been found to release sFRP2, which can inhibit osteoblast differentiation in vitro.17 Taken together, these studies provide strong evidence to suggest that soluble antagonists of the Wnt signaling pathway, Dkk1 and sFRP2, may play a role in the development of myeloma bone disease.
The aim of the present study was to determine whether increasing Wnt signaling within the bone microenvironment in myeloma can prevent the development of myeloma bone disease, using the 5TGM1 murine model of myeloma. By specific inhibition of β-catenin activity in myeloma cells combined with systemic stimulation of the Wnt signaling pathway, our results suggest that increasing Wnt signaling in myeloma has dual effects; first, to directly increase myeloma growth at nonosseous sites, and second to enhance bone formation and thus indirectly reduce tumor burden in bone, highlighting the importance of the bone marrow microenvironment in regulating myeloma growth and survival.
Methods
Reagents
Recombinant Wnt-3A was from R & D Systems (Minneapolis, MN). Dominant negative TCF4 (ΔNTCF4), in which amino acids 2 to 53 (β-catenin–binding domain) had been deleted, was kindly provided by Dr Osamu Tetsu, University of California at San Francisco.18 Unless stated otherwise, all other chemical and tissue culture reagents were from Sigma Chemical (St Louis, MO).
Cell culture
The 5TGM1-GFP myeloma cell line was cultured as described previously.19,20 Cells were plated at 5 × 105/mL and treated with 10 mM lithium chloride (LiCl) or 50 ng/mL Wnt-3A for 24 hours. Proliferation was assessed using a colorimetric MTT assay (Promega, Madison, WI) following the manufacturer's instructions.
Stable cell lines
5TGM1-GFP cells were transfected with 2 μg pcDNA3 or ΔNTCF4 by electroporation using nucleofector technology (solution V, program H023; Amaxa, Gaithersburg, MD). Cells were cultured in RPMI 1640 media as referred to in “Cell culture,” supplemented with 1.6 mg/mL geneticin (Invitrogen, Carlsbad, CA). Dead cells were removed by magnetic bead separation using a Dead Cell Removal Kit (Miltenyi Biotech, Auburn, CA), according to the manufacturer's instructions. Overexpression of ΔNTCF4 was confirmed by Western blotting for myc expression, and cells were continuously cultured in geneticin to maintain overexpression.
Real-time PCR
RNA was extracted using a RNeasy kit (Qiagen, Valencia, CA). Total RNA (1 μg) was used for first-strand cDNA synthesis using Superscript II reverse transcriptase with random hexamers (Invitrogen). Real-time polymerase chain reaction (PCR) was performed using primers and probes for axin2 (Applied Biosystems, Foster City, CA) on an Applied Biosystems 7300 Real-Time PCR System according to the manufacturer's instructions.
Western blotting
Total cell lysates for Western blots were prepared by lysing cell pellets in radioimmunoprecipitation assay (RIPA) buffer containing 1 mM EDTA. Lysates were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE), transferred to polyvinylidene difluoride membranes, and then blocked in TBS plus 5% BSA and 0.1% TWEEN for 1 hour, before incubating with anti–β-catenin (clone BDI480 and clone BDI770; Abcam, Cambridge, MA), anti-myc (Abcam), or anti–β-actin at 4°C overnight. Antigen-antibody complexes were detected using secondary antibodies conjugated to HRP and visualized by enhanced chemiluminescence (GE Healthcare, Piscataway, NJ).
TOPFLASH Wnt reporter assay
To assay for activation of β-catenin/TCF target genes, 5TGM1 myeloma cells were transiently transfected with 2 μg Wnt reporter constructs containing wild-type (TOPFLASH) or mutated (FOPFLASH) LEF/TCF-binding sites (Upstate, Charlottesville, VA) by electroporation using nucleofector technology (solution V, program H023; Amaxa). Cells were cotransfected with 0.2 μg β-galactosidase reporter vector as a control for transfection efficiency. Following transfection, cells were cultured for 24 hours; then luciferase and β-galactosidase reporter activities were assayed using the BrightGlo and β-Glo assay kits, respectively (Promega). TOPFLASH results were normalized to activity of β-galactosidase, and expressed relative to FOPFLASH values. The reporter assay results represent the average of 3 separate experiments.
5TGM1 myeloma model
Studies were conducted using weight-matched, 8- to 10-week-old female C57BL/KaLwRijHsd mice (Harlan Netherlands, Horst, The Netherlands). Studies were approved by the Institute of Animal Care and Use Committees at the University of Texas Health Science Center at San Antonio and Vanderbilt University and conducted in accordance with the National Institutes of Health (NIH) Guide for the Care and Use of Laboratory Animals.21 Mice were housed in isolator cages where autoclaved chow and acidified water were provided ad libitum. Disseminated myeloma was induced by intravenously inoculating 106 5TGM1-GFP cells in 100 μL phosphate-buffered saline (PBS) into C57BL/KaLwRij mice through the tail vein (n = 12). Mice were similarly inoculated with PBS alone (n = 6). After tumor cell inoculation, mice were randomized to receive either 200 mg/kg per day LiCl in 100 μL deionized water (d.H2O) or 100 μL d.H2O alone, by oral gavage from time of tumor inoculation until time of humane killing. Sera were assayed for monoclonal mouse IgG2bκ paraprotein as described previously,22 and whole-blood ionized calcium measurements and whole-body radiographs determined as described previously.19 Bone mineral density (BMD) measurements were obtained by dual-energy X-ray absorptiometry scan using a Lunar PIXImus imager (GE Medical Systems, Little Chalfont, United Kingdom). Solitary plasmacytomas were induced by injection of 106 5TGM1-GFP cells in 100 μL PBS subcutaneously over the flank, and mice were treated with LiCl (n = 5) or d.H2O (n = 5) for the same duration as described previously for disseminated myeloma. Once tumors were palpable, serial measurements of tumor diameters in 3 dimensions were made at daily intervals using electronic calipers and tumor volumes calculated as described by LeBlanc et al.23 In another series of experiments, 106 5TGM1-pcDNA or 5TGM1-ΔNTCF4 cells were inoculated into C57BL/KaLwRij mice by intravenous tail vein (n = 8 per group). Mice inoculated with 100 μL PBS served as control (n = 6). Mice in either group were randomized to receive 200 mg/kg per day LiCl or d.H2O, by oral gavage from time of tumor inoculation until time of humane killing. Sera were assayed for mouse IgG2bκ as described previously.22 To examine dynamic changes in bone formation, mice were injected intraperitoneally with 20 mg/kg calcein green on days 21 and 25 after inoculation. A separate cohort of C57Bl/KaLwRij mice was inoculated subcutaneously with either 106 5TGM1-pcDNA or 5TGM1-ΔNTCF4 cells (n = 5 per group) to induce plasmacytomas and tumor volumes calculated as described above.
Bone histologic and cytochemical analyses
Fixed and decalcified long bones and spines were paraffin embedded and consecutive 4-μm-thick sections were stained with hematoxylin and eosin (H&E) and for tartrate-resistant acid phosphatase (TRAP) activity. For visualization of calcein labeling, spines were fixed in 70% ethanol and embedded in methylmethacrylate without prior decalcification. Sections (6-μm thick) were cut and viewed unstained by epifluorescence microscopy. Histomorphometric analysis was performed as described previously.19,24 Subcutaneous tumors were fixed and paraffin-embedded sections were stained with H&E. Consecutive sections of long bones and subcutaneous tumors were stained for β-catenin using a 1:50 dilution of 2 independent monoclonal antibodies to β-catenin or isotype control (clone 14/β-catenin [BD Biosciences, San Jose, CA]; clone BDI480 [Abcam]). Sections of subcutaneous tumors were stained for Ki67 using a 1:200 dilution of a polyclonal antibody to Ki67 (Abcam). Antibodies were detected using a DAKO LSAB visualization system (Glostrup, Denmark), following the manufacturer's instructions. Following Ki67 immunostaining, sections were scored blind to generate a proliferation index (percentage of Ki67-positive cells from the total cells). Five fields were assessed per tumor at 40× magnification. Images were acquired using an Olympus BX41 microscope, with 40×/0.75 NA or 20×/0.5 NA objectives and an Olympus DP71 camera using DP Controller 3.1.1.267 software (Olympus, Center Valley, PA).
Microcomputed tomography (microCT) analysis
Tibiae were fixed in formalin, and each bone was scanned at an isotropic voxel size of 12 μm using a microCT40 (SCANCO Medical, Bassersdorf, Switzerland). In analyzing the reconstructed images, contours were drawn within the cortices around the metaphyses, such that the total volume (TV) included only trabecular bone at 0.2 mm below the growth plate and extending 0.12 mm. Bone volume (BV) included all bone tissue that had a material density greater than 438.7 mgHA/cm3, thereby giving a measure of BV/TV. The same threshold setting for bone tissue was used for all samples. For analysis of cortical bone lesions, the region of interest was the entire metaphysis including the cortices and extending 0.25 mm from the growth plate. The cross-sectional images of this region were exported in tiff format and imported into AMIRA 3-D graphics software (Mercury Computer Systems, Chelmsford, MA). Using a consistent threshold, AMIRA generated 3-D renderings of the metaphyses. Rotating the virtual bone through 360°, the number of osteolytic lesions were counted, which completely penetrated the cortical bone and were greater than 100 μm in diameter.
Flow cytometry
Bone marrow was flushed from the tibia and femur of 5TGM1 myeloma–bearing mice. Spleens from myeloma-bearing mice were homogenized in tissue culture media. Cell suspensions were filtered through a 70-μm filter and then analyzed for GFP fluorescence using a 3 laser BD LSRII (Becton Dickinson, San Jose, CA).
Statistical analysis
Statistical significance was determined using a Mann-Whitney U test for nonparametric data and considered significant given P less than or equal to .05. Data are presented as means (± SEM) unless otherwise stated.
Results
LiCl inhibits the development of myeloma bone disease in vivo
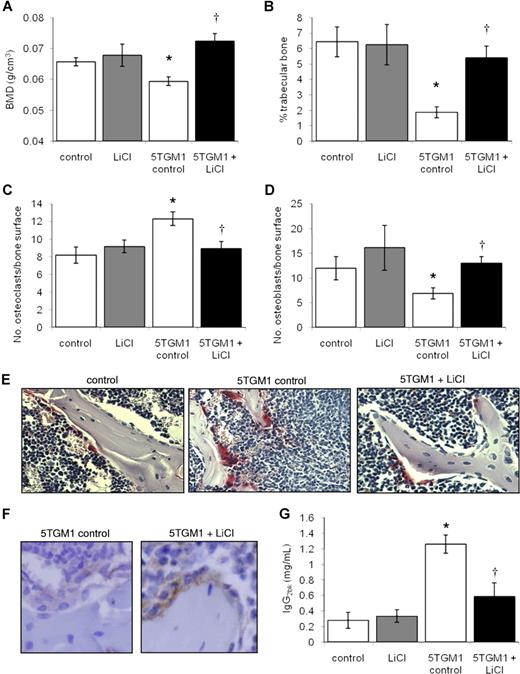
To test the hypothesis that increasing Wnt signaling in the bone marrow microenvironment would counteract the effects of myeloma bone disease, we used LiCl to activate the Wnt signaling pathway in the well-characterized 5TGM1 murine model of myeloma.19,20,22,25 LiCl is known to increase Wnt signaling by inhibition of glycogen synthase kinase 3β (GSK-3β).26,–28 The dosing schedule used in the present study has previously been demonstrated to result in serum LiCl levels within therapeutic concentrations for inhibition of GSK-3β and activation of Wnt signaling in mice of the same age as used in this investigation.29 Intravenous inoculation of 5TGM1 myeloma cells resulted in the development of myeloma bone disease, associated with a generalized osteolysis; significant decrease in BMD, trabecular bone volume, and osteoblast number; and increase in osteoclast number. Although in some instances, development of 5TGM1 myeloma is associated with splenomegaly, this was not observed in this study. Treatment of 5TGM1 myeloma–bearing mice with LiCl resulted in a significant increase in BMD and trabecular bone volume in the tibia of myeloma-bearing mice, compared with vehicle-treated 5TGM1 myeloma–bearing mice (Figure 1A,B). Identical results were found in the femora and spine (data not shown). Histomorphometric analyses revealed that LiCl treatment of myeloma-bearing mice resulted in a significant increase in osteoblasts and a reduction in TRAP-positive osteoclasts lining the trabecular bone surfaces (Figure 1C-E). LiCl had no significant effects on these parameters in non–tumor-bearing mice. LiCl treatment was associated with a clear increase in β-catenin expression in osteoblasts in vivo (Figure 1F). In addition to preventing the development of the characteristic bone disease, LiCl treatment also resulted in a significant reduction in tumor burden within bone, assessed histomorphometrically (79.06% ± 11.1% decrease compared with untreated myeloma-bearing mice), and a significant reduction in serum IgG2bκ titers (Figure 1G).
LiCl inhibits the development of myeloma bone disease in vivo. Bone mineral density is significantly increased in 5TGM1 myeloma–bearing mice following treatment with LiCl (A). Histomorphometric analysis demonstrated an increase in trabecular bone volume (B), a decrease in osteoclast number (C), and an increase in osteoblast number (D) in 5TGM1 myeloma–bearing mice following treatment with LiCl. Histologic sections of tibiae from non–tumor-bearing mice, 5TGM1 myeloma–bearing mice, and 5TGM1 myeloma–bearing mice treated with LiCl demonstrated increased osteoclasts lining the trabecular bone surface in 5TGM1 myeloma–bearing mice, and a reduction in osteoclast number in myeloma-bearing mice treated with LiCl. Osteoclasts were identified by TRAP staining. Original magnification, ×200. (E). Immunohistochemistry demonstrated an increase in β-catenin expression in osteoblasts lining the bone surface in myeloma-bearing mice treated with LiCl compared with control. Original magnification, ×400 (F). Treatment with LiCl significantly reduced serum IgG2bκ concentrations in 5TGM1 myeloma–bearing mice (G). Data are expressed as means (± SEM). *P < .05 compared with nontumor control. †P < .05 compared with 5TGM1 control.
LiCl inhibits the development of myeloma bone disease in vivo. Bone mineral density is significantly increased in 5TGM1 myeloma–bearing mice following treatment with LiCl (A). Histomorphometric analysis demonstrated an increase in trabecular bone volume (B), a decrease in osteoclast number (C), and an increase in osteoblast number (D) in 5TGM1 myeloma–bearing mice following treatment with LiCl. Histologic sections of tibiae from non–tumor-bearing mice, 5TGM1 myeloma–bearing mice, and 5TGM1 myeloma–bearing mice treated with LiCl demonstrated increased osteoclasts lining the trabecular bone surface in 5TGM1 myeloma–bearing mice, and a reduction in osteoclast number in myeloma-bearing mice treated with LiCl. Osteoclasts were identified by TRAP staining. Original magnification, ×200. (E). Immunohistochemistry demonstrated an increase in β-catenin expression in osteoblasts lining the bone surface in myeloma-bearing mice treated with LiCl compared with control. Original magnification, ×400 (F). Treatment with LiCl significantly reduced serum IgG2bκ concentrations in 5TGM1 myeloma–bearing mice (G). Data are expressed as means (± SEM). *P < .05 compared with nontumor control. †P < .05 compared with 5TGM1 control.
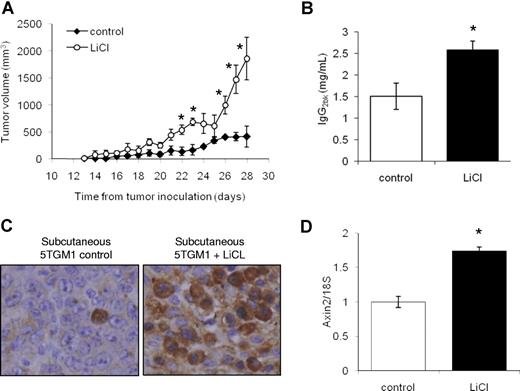
LiCl increases subcutaneous plasmacytoma growth
To determine whether LiCl has direct effects on myeloma growth in vivo, independent from the bone microenvironment, mice were inoculated subcutaneously with 5TGM1 myeloma cells and treated with LiCl using the same dosing schedule as described above. LiCl significantly increased subcutaneous tumor volume (Figure 2A) and whole tumor wet weight at humane killing by 283% (± 60%) as compared with vehicle-treated subcutaneous tumor-bearing mice. Treatment with LiCl was also associated with a significant increase in serum IgG2bκ titers (Figure 2B). Immunohistochemistry demonstrated a clear increase in β-catenin expression in myeloma cells in the excised 5TGM1 plasmacytomas from mice treated with LiCl (Figure 2C). Identical results were found using a different antibody (clone BDI480, data not shown). Real-time PCR analysis revealed a significant increase in expression of the β-catenin target gene, axin2, in RNA isolated from LiCl-treated, but not control (vehicle-treated), subcutaneous plasmacytomas (Figure 2D).
LiCl increases subcutaneous myeloma growth. Treatment with LiCl significantly increased subcutaneous tumor volume (A) and serum IgG2bκ concentrations (B). Immunohistochemistry staining of sections from subcutaneous tumors demonstrated an increase in β-catenin expression in myeloma cells from those mice treated with LiCl. Original magnification, ×400 (C). Real-time PCR demonstrated an increase in axin2 expression in mRNA isolated from subcutaneous tumors treated with LiCl (D). Data are expressed as means (± SEM). *P < .05 compared with untreated control.
LiCl increases subcutaneous myeloma growth. Treatment with LiCl significantly increased subcutaneous tumor volume (A) and serum IgG2bκ concentrations (B). Immunohistochemistry staining of sections from subcutaneous tumors demonstrated an increase in β-catenin expression in myeloma cells from those mice treated with LiCl. Original magnification, ×400 (C). Real-time PCR demonstrated an increase in axin2 expression in mRNA isolated from subcutaneous tumors treated with LiCl (D). Data are expressed as means (± SEM). *P < .05 compared with untreated control.
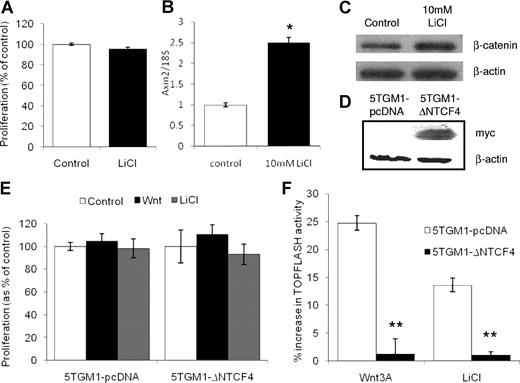
LiCl increases β-catenin activity in 5TGM1 myeloma cells in vitro
To further investigate the effects of LiCl on 5TGM1 myeloma cells, in vitro studies were performed to study proliferation and β-catenin activity. Although LiCl was found to have no significant effect on 5TGM1 cell proliferation (Figure 3A), the same dose of LiCl was found to significantly increase expression of axin2 (Figure 3B) along with expression of unphosphorylated β-catenin (Figure 3C). To confirm the specificity of unphosphorylated β-catenin expression, 2 different antibodies were used.30 Results shown are using clone BDI480, and identical results were found with clone BDI770 (data not shown). To determine the effect of specific blockade of Wnt signaling in myeloma cells, 5TGM1 myeloma cells were stably transfected with myc-tagged ΔNTCF4 or pcDNA3, and expression of ΔNTCF4 was confirmed by Western blotting for myc expression (Figure 3D). Overexpression of ΔNTCF4 had no significant effect on the growth rate of 5TGM1 myeloma cells in vitro, or proliferation in response to LiCl or Wnt 3A (Figure 3E). In contrast, overexpression of ΔNTCF4 completely prevented the increase in β-catenin activity as determined by TOPFLASH activity in response to treatment with both LiCl and Wnt3A (Figure 3F), confirming that Wnt signaling is abrogated in 5TGM1-ΔNTCF4 cells.
LiCl increases β-catenin activity in 5TGM1 myeloma cells in vitro. LiCl (10 mM) had no significant effect on 5TGM1 myeloma cell proliferation (A), but significantly increased axin2 mRNA expression (B) and expression of β-catenin (C). 5TGM1 myeloma cells were stably transfected with myc-tagged ΔNTCF4 or pcDNA (D). Wnt3A or LiCl treatment had no effect on proliferation of 5TGM1-pcDNA or 5TGM1-ΔNTCF4 cells (E). Overexpression of ΔNTCF4 completely blocked the increase in β-catenin activity as measured by TOPFLASH reporter activity (F). Data are expressed as means (± SEM). *P < .05 compared with control. **P < .01 compared with 5TGM1-pcDNA.
LiCl increases β-catenin activity in 5TGM1 myeloma cells in vitro. LiCl (10 mM) had no significant effect on 5TGM1 myeloma cell proliferation (A), but significantly increased axin2 mRNA expression (B) and expression of β-catenin (C). 5TGM1 myeloma cells were stably transfected with myc-tagged ΔNTCF4 or pcDNA (D). Wnt3A or LiCl treatment had no effect on proliferation of 5TGM1-pcDNA or 5TGM1-ΔNTCF4 cells (E). Overexpression of ΔNTCF4 completely blocked the increase in β-catenin activity as measured by TOPFLASH reporter activity (F). Data are expressed as means (± SEM). *P < .05 compared with control. **P < .01 compared with 5TGM1-pcDNA.
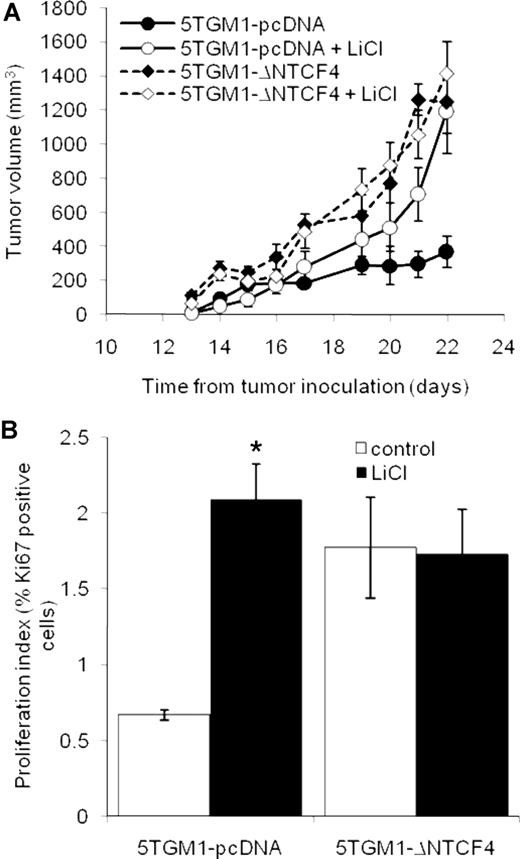
Inhibition of Wnt signaling prevents the response to LiCl in subcutaneous 5TGM1 tumors
To determine whether the LiCl-induced increase in the growth of subcutaneous 5TGM1 tumors was due to direct activation of Wnt signaling in myeloma cells, we investigated the response in subcutaneous tumors induced by 5TGM1-ΔNTCF4 cells in which the Wnt signaling pathway is blocked, compared with 5TGM1-pcDNA cells in which the Wnt signaling pathway is intact. Although we found no difference in the in vitro growth rates, there were significant differences in tumor volume and proliferation index between 5TGM1-pcDNA and 5TGM1-ΔNTCF4 subcutaneous tumors (Figure 4A,B). Despite the difference in growth rates, it was possible to determine the response of these subcutaneous tumors to LiCl as a significant increase in tumor volume was observed in LiCl-treated 5TGM1-pcDNA plasmacytomas, but not in LiCl-treated 5TGM1-ΔNTCF4 plasmacytomas (Figure 4A). To investigate further the direct effect of LiCl on proliferation in vivo, we quantitated expression of the Ki67 antigen, which is expressed by proliferating cells in all phases of the cell cycle. LiCl significantly increased myeloma cell proliferation by 221% (± 35%) in 5TGM1-pcDNA subcutaneous tumors, but had no effect on the proliferation index in 5TGM1-ΔNTCF4 subcutaneous tumors (Figure 4B). Histologic analysis demonstrated no significant difference in the proportion of apoptotic myeloma cells between 5TGM1-pcDNA and 5TGM1-ΔNTCF4 tumors in response to LiCl (data not shown).
Overexpression of ΔNTCF4 prevents the response to LiCl in subcutaneous 5TGM1 tumors. Mice were inoculated subcutaneously with 5TGM1-pDNA or 5TGM1-ΔNTCF4 cells and treated with 200 mg/kg per day LiCl. LiCl significantly increased tumor volume in 5TGM1-pcDNA tumors, but not in 5TGM1-ΔNTCF4 tumors (A). Immunohistochemistry for Ki67 demonstrated an increase in the proliferation index of 5TGM1-pcDNA cells following treatment with LiCl, but not in 5TGM1-ΔNTCF4 cells. Proliferation index was calculated as the percentage of Ki67-positive cells among the total number of tumor cells (B). Data are expressed as means (± SEM). *P < .05 compared with control.
Overexpression of ΔNTCF4 prevents the response to LiCl in subcutaneous 5TGM1 tumors. Mice were inoculated subcutaneously with 5TGM1-pDNA or 5TGM1-ΔNTCF4 cells and treated with 200 mg/kg per day LiCl. LiCl significantly increased tumor volume in 5TGM1-pcDNA tumors, but not in 5TGM1-ΔNTCF4 tumors (A). Immunohistochemistry for Ki67 demonstrated an increase in the proliferation index of 5TGM1-pcDNA cells following treatment with LiCl, but not in 5TGM1-ΔNTCF4 cells. Proliferation index was calculated as the percentage of Ki67-positive cells among the total number of tumor cells (B). Data are expressed as means (± SEM). *P < .05 compared with control.
Increasing Wnt signaling in the bone microenvironment prevents myeloma bone disease and reduces tumor burden in bone
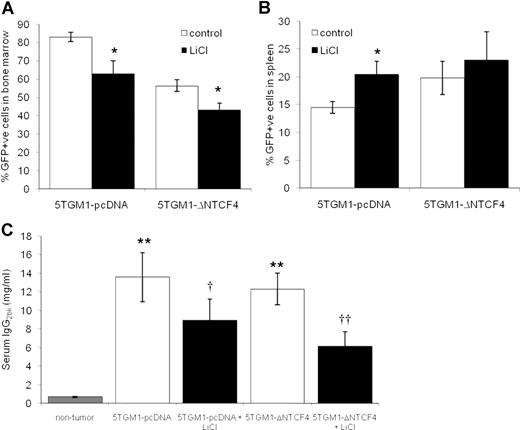
Although our data clearly demonstrate that treatment with LiCl prevents the development of myeloma bone disease in vivo, it is unclear whether this is mediated by effects on the bone marrow microenvironment or the tumor cells directly. To address this issue, we used 5TGM1-ΔNTCF4 myeloma cells in which Wnt signaling is abrogated. Mice were inoculated intravenously with GFP-expressing 5TGM1-ΔNTCF4 cells or 5TGM1-pcDNA cells and treated with LiCl from the time of tumor inoculation. Flow cytometric analysis demonstrated that mice bearing 5TGM1-pcDNA or 5TGM1-ΔNTCF4 myeloma accumulated GFP-positive cells in the bone marrow and spleen (Figure 5A,B). However mice bearing 5TGM1-ΔNTCF4 cells had a significantly lower proportion of GFP-positive cells in the bone marrow than those mice bearing 5TGM1-pcDNA myeloma. In contrast, there was a 36% increase in the proportion of GFP-positive cells in spleens of 5TGM1-ΔNTCF4 myeloma–bearing mice compared with 5TGM1-pcDNA myeloma–bearing mice, although this increase was not statistically significant. Treatment with LiCl resulted in a significant decrease in GFP-positive cells in the bone marrow of both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (Figure 5A), consistent with our previous observations that LiCl reduces tumor burden within bone. In contrast, LiCl significantly increased the proportion of GFP-positive cells in the spleen in 5TGM1-pcDNA myeloma–bearing mice, but had no effect in 5TGM1-ΔNTCF4 myeloma–bearing mice (Figure 5B). We also measured serum IgG2bκ concentrations, which reflect total myeloma burden in bone marrow and spleen. There was no significant difference in serum IgG2bκ concentrations between untreated 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice, however treatment with LiCl resulted in a significant 34% and 50% decrease, respectively (Figure 5C).
Increasing Wnt signaling in the bone microenvironment reduces myeloma tumor burden in bone. Mice were inoculated intravenously with 5TGM1-pcDNA or 5TGM1-ΔNTCF4 myeloma cells that homed to bone marrow and spleen. Single cell suspensions were isolated from bone marrow and spleen, and the proportion of GFP-positive cells was determined by flow cytometry. LiCl significantly reduced the proportion of GFP-positive cells in the bone marrow of both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (A). In contrast, LiCl significantly increased the proportion of GFP-positive bone marrow cells in the spleen of 5TGM1-pcDNA myeloma–bearing mice but not 5TGM1-ΔNTCF4 myeloma–bearing mice (B). Treatment with LiCl significantly reduced serum IgG2bκ concentrations in both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (C). Data are expressed as means (± SEM). *P < .05 compared with control. **P < .01 compared with nontumor. †P < .05, ††P < .01 compared with untreated.
Increasing Wnt signaling in the bone microenvironment reduces myeloma tumor burden in bone. Mice were inoculated intravenously with 5TGM1-pcDNA or 5TGM1-ΔNTCF4 myeloma cells that homed to bone marrow and spleen. Single cell suspensions were isolated from bone marrow and spleen, and the proportion of GFP-positive cells was determined by flow cytometry. LiCl significantly reduced the proportion of GFP-positive cells in the bone marrow of both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (A). In contrast, LiCl significantly increased the proportion of GFP-positive bone marrow cells in the spleen of 5TGM1-pcDNA myeloma–bearing mice but not 5TGM1-ΔNTCF4 myeloma–bearing mice (B). Treatment with LiCl significantly reduced serum IgG2bκ concentrations in both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (C). Data are expressed as means (± SEM). *P < .05 compared with control. **P < .01 compared with nontumor. †P < .05, ††P < .01 compared with untreated.
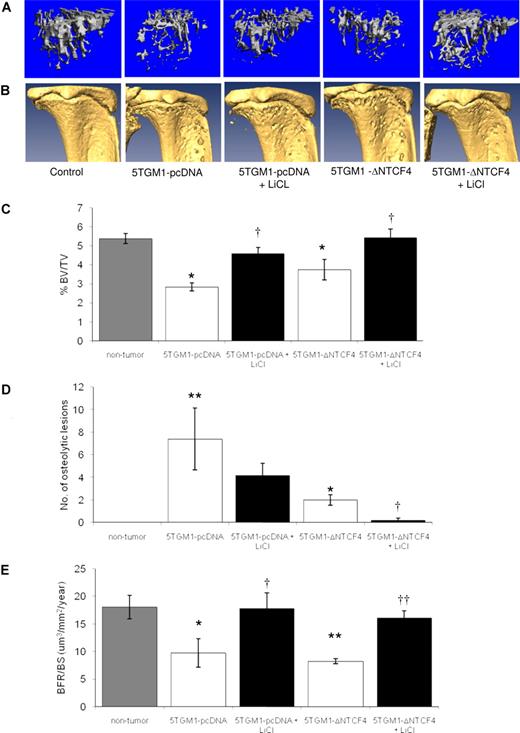
Mice bearing 5TGM1-pcDNA or 5TGM1-ΔNTCF4 myeloma developed an osteolytic bone disease, characterized by an increase in osteolytic bone lesions and osteoclast number and a decrease in trabecular bone volume, osteoblast number, and bone formation rates. The reduction in trabecular bone volume and the increase in osteolytic bone lesions were greater in 5TGM1-pcDNA myeloma–bearing mice than in 5TGM1-ΔNTCF4 myeloma–bearing mice. MicroCT analyses of the trabecular (Figure 6A) and cortical (Figure 6B) bone from the tibia demonstrated that treatment with LiCl resulted in a significant increase in trabecular bone volume (Figure 6C) and reduction in the number of osteolytic lesions (Figure 6D) in both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice. To account for the differences in tumor burden within bone between 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice, the effect of LiCl was also expressed as percentage change from control. Although there was no significant difference in the effect of LiCl on trabecular bone volume in 5TGM1-pcDNA compared with 5TGM1-ΔNTCF4 (data not shown), LiCl reduced the number of osteolytic lesions by 43.2% (± 15.6%) in 5TGM1-pcDNA myeloma–bearing mice, compared with 87.5% (± 12.5%) in 5TGM1-ΔNTCF4 myeloma–bearing mice. MicroCT analysis also revealed a decrease in trabecular number and thickness and an increase in trabecular separation in myeloma-bearing mice. LiCl reversed this decrease in trabecular number and thickness and concomitantly reduced trabecular spacing in both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (Table 1). Histomorphometric analysis revealed that LiCl treatment significantly decreased osteoclast number by 47.2% (± 11.4%) and 53.1% (± 13.3%; P < .05 compared with vehicle control), and significantly increased osteoblast number by 312.5% (± 69.2%) and 233.1% (± 45.9%; P <.05 compared with vehicle control), in 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice, respectively. As in myeloma patients, the development of myeloma bone disease in the 5TGM1 model was also associated with a significant reduction in the rates of bone formation, assessed by double calcein labeling of bone-forming surfaces. Consistent with an increase in bone volume, LiCl significantly increased bone formation in both 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice (Figure 6E).
Increasing Wnt signaling in the bone microenvironment prevents the development of myeloma bone disease. MicroCT analysis of tibiae of 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice demonstrated a significant reduction in trabecular bone volume (A,C) and increase in osteolytic bone lesions (B,D) that was prevented by treatment with LiCl. LiCl also significantly prevented the reduction in bone formation rates associated with the development of myeloma bone disease (E). Data are expressed as means (± SEM). *P < .05 compared with nontumor. **P < .01 compared with nontumor. †P < .05, ††P < .01 compared with untreated.
Increasing Wnt signaling in the bone microenvironment prevents the development of myeloma bone disease. MicroCT analysis of tibiae of 5TGM1-pcDNA and 5TGM1-ΔNTCF4 myeloma–bearing mice demonstrated a significant reduction in trabecular bone volume (A,C) and increase in osteolytic bone lesions (B,D) that was prevented by treatment with LiCl. LiCl also significantly prevented the reduction in bone formation rates associated with the development of myeloma bone disease (E). Data are expressed as means (± SEM). *P < .05 compared with nontumor. **P < .01 compared with nontumor. †P < .05, ††P < .01 compared with untreated.
Effects of increasing Wnt signaling in the myeloma bone microenvironment on trabecular structure
| . | Nontumor . | 5TGM1-pcDNA . | 5TGM1-pcDNA + LiCl . | 5TGM1−Δ NTCF4 . | 5TGM1−Δ NTCF4 + LiCl . |
|---|---|---|---|---|---|
| BV/TV, % | 5.38 ± 0.26 | 2.83 ± 0.20* | 4.60 ± 0.31† | 3.75 ± 0.54* | 5.42 ± 0.45† |
| Tb. no., 1/mm | 2.81 ± 0.07 | 2.34 ± 0.07‡ | 2.70 ± 0.13† | 2.65 ± 0.21 | 2.93 ± 0.09 |
| Tb. thickness, mm | 0.048 ± 0.001 | 0.045 ± 0.001* | 0.048 ± 0.001† | 0.043 ± 0.002* | 0.047 ± 0.001 |
| Tb. separation, mm | 0.36 ± 0.01 | 0.43 ± 0.01* | 0.38 ± 0.02† | 0.39 ± 0.03 | 0.35 ± 0.01 |
| . | Nontumor . | 5TGM1-pcDNA . | 5TGM1-pcDNA + LiCl . | 5TGM1−Δ NTCF4 . | 5TGM1−Δ NTCF4 + LiCl . |
|---|---|---|---|---|---|
| BV/TV, % | 5.38 ± 0.26 | 2.83 ± 0.20* | 4.60 ± 0.31† | 3.75 ± 0.54* | 5.42 ± 0.45† |
| Tb. no., 1/mm | 2.81 ± 0.07 | 2.34 ± 0.07‡ | 2.70 ± 0.13† | 2.65 ± 0.21 | 2.93 ± 0.09 |
| Tb. thickness, mm | 0.048 ± 0.001 | 0.045 ± 0.001* | 0.048 ± 0.001† | 0.043 ± 0.002* | 0.047 ± 0.001 |
| Tb. separation, mm | 0.36 ± 0.01 | 0.43 ± 0.01* | 0.38 ± 0.02† | 0.39 ± 0.03 | 0.35 ± 0.01 |
Trabecular bone volume (BV/TV), number, thickness and separation were calculated by microCT analysis of tibiae.
Tb indicates trabecular.
P < .05 compared with nontumor.
P < .05 compared with vehicle control.
P <.01 compared with nontumor.
Discussion
The increasing evidence for the role of Wnt signaling in the regulation of bone formation and for the role of the soluble antagonist Dkk1 in the pathogenesis of myeloma bone disease identifies the Wnt signaling pathway as a potential therapeutic target in multiple myeloma. In the present study, we demonstrate that increasing Wnt signaling in the bone marrow microenvironment can prevent the development of myeloma bone disease, by both increasing osteoblast number and bone formation, and concomitantly reducing osteoclast number. Activation of the Wnt signaling pathway was achieved by a pharmacological approach: systemic treatment with LiCl that inhibits glycogen synthase kinase 3β (GSK-3β), an enzyme responsible for the phosphorylation and subsequent proteasomal degradation of β-catenin.26,–28 The dosing schedule used in the present study has previously been demonstrated to result in serum LiCl levels within therapeutic concentrations for inhibition of GSK-3β and activation of Wnt signaling in mice of the same age as used in this investigation.29
Wnt signaling is known to increase osteoblast differentiation and bone formation in vivo.9,11,31 In support of this, we demonstrate a clear increase in β-catenin expression in osteoblasts following treatment with LiCl, suggesting that LiCl prevents the development of myeloma bone disease by increasing Wnt signaling in osteoblasts. Lithium treatment of patients with bipolar disease has been documented to result in an increase in serum parathyroid hormone and an associated hypercalcemia, however there is little evidence for a significant effect of lithium on bone mass or bone density.32,,,–36 In our experiments, there was no significant increase in ionized calcium in response to LiCl, either in non–tumor- or myeloma-bearing mice, thus excluding this potential confounding effect from the present study. LiCl had no significant effect on non–tumor-bearing mice, suggesting that the response to increasing Wnt signaling is enhanced in conditions associated with dysregulation of this pathway, such as multiple myeloma. This is supported by studies that demonstrate that the response to LiCl is greater in LRP5−/− mice compared with wild-type mice.29 Wnt signaling in osteoblasts has also been demonstrated to regulate osteoclast function, with β-catenin in osteoblasts functioning as a negative regulator of osteoclast function.12,37,38 In support of this, we show that LiCl treatment significantly reduces osteoclast number in myeloma-bearing mice. While we found strong expression of β-catenin in osteoclasts, there was no change in expression in response to LiCl treatment, suggesting that the reduction in osteoclast number may be an indirect response to increasing Wnt signaling in osteoblasts. The canonical Wnt signaling pathway is critical for the self-renewal of hematopoietic stem cells, and therefore increasing Wnt signaling in the bone marrow may promote the regeneration of the bone marrow microenvironment.39 Thus, the effects of increasing Wnt signaling in hematopoietic stem cells may also contribute to the protective effects of this approach in the treatment of myeloma bone disease.
It is well established that the Wnt signaling pathway plays a key role in bone formation, however its precise role in growth and survival of myeloma cells remains controversial. Activation of the Wnt signaling pathway through β-catenin plays a critical oncogenic role in many human malignancies, and expression of β-catenin has been demonstrated in myeloma cell lines and in malignant plasma cells from patients with multiple myeloma.40,41 However, published data are conflicting as to the function of the Wnt signaling pathway in myeloma cells. Derksen et al demonstrated that stimulation of the canonical Wnt signaling pathway increases proliferation of human myeloma cell lines.40 More recently, a small molecule inhibitor of the β-catenin/TCF interaction was found to inhibit myeloma cell proliferation, both in vitro and in a xenograft model of myeloma.42 In contrast, Qiang et al have demonstrated that although activation of Wnt signaling results in an increase in β-catenin activity in myeloma cells, this is not associated with a proliferative effect.43 In addition, they showed that activation of Wnt signaling with Wnt3A results in morphologic changes and an increase in invasion and migration of myeloma cells. Importantly, they also demonstrated that these effects were mediated through the Wnt/RhoA pathway and were independent of signaling through β-catenin.43,44 The present study combines both pharmacological and molecular approaches to target the Wnt signaling pathway in myeloma cells, both in vitro and in vivo. In agreement with Qiang et al, we found that although activation of the Wnt signaling pathway in myeloma cells results in an increase in β-catenin activity, there was no associated proliferative effect in vitro. However, our in vivo studies suggest that the role of the Wnt signaling pathway in myeloma cells may be more complex and dependent upon the microenvironment. In subcutaneous plasmacytoma tumors, increasing Wnt signaling results in an increase in tumor volume and tumor cell proliferation, associated with an increase in β-catenin expression and activation of downstream target genes. Molecular blockade of β-catenin activity by overexpression of dominant negative TCF4 in myeloma cells completely prevented the increase in subcutaneous tumor burden and proliferation, confirming that this increase was dependent upon active canonical Wnt signaling in myeloma cells. The difference between the in vitro and in vivo observations may reflect the well known limitations of using myeloma cell lines in vitro, but may also suggest a dependence of the Wnt signaling pathway upon environmental factors that are not present in the in vitro cultures and indicate the necessity for in vivo preclinical studies to fully investigate the pathogenesis of myeloma bone disease.
Although there was no difference in the in vitro growth rates, there was a difference in the tumor volumes and proliferation rates between subcutaneous tumors with intact Wnt signaling pathway (5TGM1-pcDNA) compared with those with blocked β-catenin transcriptional activity (5TGM1-ΔNTCF4). Since we have clearly demonstrated that increasing Wnt signaling results in a direct increase in tumor growth in subcutaneous 5TGM1 tumors, it is most likely that this represents an unexpected difference in the in vivo growth rates following selection of transfected cells. In support of this, there was also a trend toward an increase in tumor burden in the spleen in those mice bearing 5TGM1-ΔNTCF4 myeloma, with a small increase in both spleen weight and the proportion of tumor cells within the spleen, although this was not statistically significant. In contrast, there was a significant decrease in tumor burden within bone in those mice bearing 5TGM1-ΔNTCF4 myeloma, compared with 5TGM1-pcDNA myeloma. As the results with the subcutaneous tumors suggest that the 5TGM1-ΔNTCF4 cells grow faster in vivo, our observations in the bone marrow microenvironment suggest that myeloma cells may be dependent upon Wnt signaling to promote growth within this specialized environment, and so blockade of the Wnt signaling pathway results in a reduction in tumor burden. The bone marrow microenvironment in multiple myeloma is associated with high concentrations of Dkk1 that are critical in the pathogenesis of myeloma bone disease, and it is intriguing to speculate that the Wnt signaling pathway is regulated in myeloma cells within this specialized microenvironment to compensate for the increase in Dkk1. These data raise the possibility that response of tumor cells to the Wnt signaling pathway is highly dependent upon the microenvironment and the local balance of agonists and antagonists of this pathway.
The discovery of Dkk1 as a mediator of the reduction in osteoblastic bone formation in multiple myeloma, and the compelling evidence for the critical role of Wnt signaling in promoting osteoblast differentiation and bone formation, identifies the Wnt signaling pathway as a potential therapeutic target in multiple myeloma. In support of this, inhibition of Dkk1 using neutralizing antibodies was found to prevent the osteolytic bone disease and reduce tumor burden in SCID-rab mice engrafted with primary myeloma cells.16 In this model, myeloma growth is restricted to the rabbit bone and therefore it is not possible to discern unequivocally any effects on tumor burden from effects on the bone microenvironment.45 The 5TGM1 myeloma model is a well-characterized model of myeloma bone disease that closely reflects the human form of the disease. In addition, this model enables the study of myeloma growth in vivo, independent from the bone microenvironment, by inoculating tumor cells subcutaneously. The current study clearly demonstrates that increasing Wnt signaling within the myeloma bone microenvironment can inhibit the development of myeloma bone disease. However, our studies also demonstrate that increasing Wnt signaling can increase myeloma growth at nonosseous sites, and that this is likely due to direct stimulation of the Wnt signaling pathway and β-catenin activation. Extramedullary disease, while uncommon in patients with myeloma, is associated with aggressive disease, occurring subsequent to the development of myeloma bone disease and typically resulting in plasma cell leukemia. The mechanisms involved in the progression of myeloma beyond the bone marrow cavity are poorly understood, and current clinical approaches cannot accurately identify patients at risk of developing extramedullary disease. Although increasing Wnt signaling is clearly effective to prevent myeloma bone disease in vivo, our results raise important clinical concerns for targeting Wnt signaling as a therapeutic approach in myeloma due to the risk of increasing tumor growth outside the bone marrow microenvironment. Myeloma is primarily a skeletal disease and the striking difference between the response of myeloma cells within bone compared with subcutaneous growth raises questions as to the relevance of xenograft models of myeloma that do not take into consideration the influences of the bone milieu. The data presented herein further highlight the necessity to study multiple myeloma in vivo within this specialized host microenvironment.
Myeloma cells are dependent upon interactions with the cells of the host bone microenvironment for their growth and survival.46,47 Several studies have demonstrated the potential for indirect antitumor effects by inhibiting osteoclastic bone resorption.48,–50 In the present study, we clearly demonstrate a dramatic effect of directly targeting the Wnt signaling pathway in osteoblasts in myeloma. In addition to preventing the development of myeloma bone disease, the systemic increase in Wnt signaling was shown to decrease tumor burden within the bone microenvironment, despite increasing the growth of myeloma cells at extraosseous sites. This study demonstrates the striking potential for directly targeting the bone microenvironment in multiple myeloma by increasing bone formation and indirectly inhibiting tumor growth.
Parts of this work were presented in abstract form at the 28th annual meeting of the American Society of Bone and Mineral Research, Philadelphia, PA, September 15, 2006, and at the 49th Annual Meeting of the American Society of Hematology, Atlanta, GA, December 11, 2007.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by the San Antonio Cancer Institute and the National Cancer Institute (NCI) through P30 CA-054174-16 (C.M.E.), and by NCI through P01 CA-40035 (G.R.M.). B.O.O. is supported by KO1 CA-104180 from NCI. C.M.E. is supported by the International Myeloma Foundation.
National Institutes of Health
Authorship
Contribution: C.M.E. designed, performed, and analyzed research and wrote the paper; J.R.E. performed and analyzed research and reviewed the paper; S.T.L., J.E., B.M., S.M., and B.G. performed research; B.O.O. assisted in research design and reviewed the paper; and G.R.M. discussed the experiments and reviewed the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Claire M. Edwards, Vanderbilt Center for Bone Biology, 1235 Medical Research Bldg IV, Nashville, TN 37232-0575; e-mail: claire.edwards@vanderbilt.edu.