Myeloid differentiation factor-2 (MD-2) is a lipopolysaccharide (LPS)-binding protein usually coexpressed with and binding to Toll-like receptor 4 (TLR4), conferring LPS responsiveness of immune cells. MD-2 is also found as a soluble protein. Soluble MD-2 (sMD-2) levels are markedly elevated in plasma from patients with severe infections, and in other fluids from inflamed tissues. We show that sMD-2 is a type II acute-phase protein. Soluble MD-2 mRNA and protein levels are up-regulated in mouse liver after the induction of an acute-phase response. It is secreted by human hepatocytic cells and up-regulated by interleukin-6. Soluble MD-2 binds to Gram-negative but not Gram-positive bacteria, and sMD-2 secreted by hepatocytic cells is an essential cofactor for the activation of TLR4-expressing cells by Gram-negative bacteria. Soluble MD-2 opsonization of Gram-negative bacteria accelerates and enhances phagocytosis, principally by polymorphonuclear neutrophils. In summary, our results demonstrate that sMD-2 is a newly recognized type II acute-phase reactant, an opsonin for Gram-negative bacteria, and a cofactor essential for the activation of TLR4-expressing cells. This suggests that sMD-2 plays a key role in the host innate immune response to Gram-negative infections.
Introduction
Recognition of bacteria and bacterial molecules is a key step in the initiation of an innate immune response in animals and in humans. Several host humoral and cell-surface proteins are implicated in the innate immune recognition of endotoxin (lipopolysaccharide, LPS), for example. These include LPS-binding protein (LBP), CD14, Toll-like receptor 4 (TLR4), and the myeloid differentiation factor-2 (MD-2).1,,–4 Mice deficient in any one of these proteins display a similar hyporesponsiveness to LPS challenge.5,,–8
MD-2 is a glycoprotein of approximately 17-25 kDa coexpressed with TLR4 at the surface of various cell types, principally those of the myeloid and endothelial lineages.9,10 MD-2 mRNA is found in a variety of tissues.11 Despite of the absence of a transmembrane domain, it is found attached to the cell surface via its interaction with TLR4 through specific and recently identified epitopes.2,9,12,13 The sequence events by which LPS interacts with the various proteins of its receptor complex has recently been unravelled. LPS first binds CD14, which transfers it to a hydrophobic pocket within the MD-2 glycoprotein, resulting in TLR4-dependent activation of cells.5,13,–15
MD-2 also exists as a soluble protein (sMD-2) secreted by various cell types, mainly as a large disulfide-bound multimeric glycoprotein but also as oligomers and monomers.9,16,17 However, only sMD-2 monomers seem to bind to LPS and confer responsiveness to TLR4 expressing cells.18,19 Little is known about the sMD-2 secretory pathway. MD-2 possesses a consensus sequence for a secretory signal peptide consisting of a 16-amino-acid NH2-terminal hydrophobic stretch.2 An alternatively spliced MD-2 variant inhibiting TLR4 expression has been described in mice but not in humans.20
Soluble proteins are essential in the host response to microbial infections. Some of these proteins, such as LBP and soluble CD14, are cofactors for the activation of cells by bacterial molecules.3,21 Others function as opsonins (LBP, serum amyloid protein A, complement, and mannose-binding lectins), or are directly bactericidal, such as the bactericidal permeability-increasing (BPI) protein and complement, for example.22,,,–26 It is noteworthy that many of these proteins are acute-phase proteins.24,27,,,–31
We have recently reported a marked increase in sMD-2 activity in plasma from patients with sepsis, and, to a lesser extent, in plasma from patients with an acute exacerbation of rheumatoid arthritis.32 Increased levels of sMD-2 in septic plasma were subsequently confirmed.33 sMD-2 has also been detected in other body fluids, including urine and lung edema fluid from patients with sepsis.32 It has been proposed that high concentrations of sMD-2, like soluble CD14 and high-density lipoproteins, may act as a sink for LPS.34 The relative concentration of monomer versus polymer in human body fluids is unknown. The origin and the reasons for increased levels of plasma sMD-2 remain to be determined.
Herein, we tested the hypothesis that sMD-2 is an acute-phase protein and opsonizes Gram-negative bacteria. We found that sMD-2 was regulated as a type II acute-phase protein and bound to Gram-negative bacteria. It acted as a coactivator for Gram-negative bacterial activation of TLR4-expressing cells and increased Gram-negative bacterial phagocytosis by polymorphonuclear neutrophils and monocytes, 2 essential mechanisms in the innate immune response to Gram-negative bacteria. Soluble MD-2, however, did not show a bactericidal effect.
Methods
Cells, bacteria, and reagents
THP-1 and HepG2 cells were obtained from the American Type Culture Collection (Manassas, VA), HepaRG cells were obtained from M. Strubin (University of Geneva, Geneva, Switzerland), and human embryonic kidney (HEK) 293 cells from D. Trono (Ecole Polytechnique Federale de Lausanne, Lausanne, Switzerland). HEK293 cell line stably expressing human TLR4 receptor (TLR4-HEK293) was established with a TLR4 expression plasmid obtained from M. Rothe (Amgen, Thousand Oaks, CA). Escherichia coli and Staphylococcus aureus isolates from patients with clinically relevant infections were obtained from P. Rohner (Clinical Microbiology Laboratory, University Hospitals of Geneva, Geneva, Switzerland). E coli K12 W3110 and Bacillus subtilis bacteria were obtained from P. Genevaux (University of Geneva). The production, the purification, and the characterization of recombinant human FLAG and poly–His-tagged soluble MD-2 have been described elsewhere.32 Anti–human MD-2 18H10 and anti–human TLR4 15C1 mAbs have been characterized previously.32,35 Ultrapure E coli K12LCD25 LPS was purchased from InvivoGen (San Diego, CA). Cells were stimulated with 10 ng/mL recombinant human interleukin (IL)-6 (R&D Systems, Minneapolis, MN), 1 ng/mL IL-1β (R&D), or 10 μM dexamethasone (Sigma-Aldrich, St Louis, MO).
Acute-phase response in mice
Liver cDNA from IL-6 knockout (−/−) C57BL/6 mice and C57BL/6 littermates treated with 100-μL injections of turpentine or normal saline in each hind limb was obtained from C. Gabay (University of Geneva).28 Wild-type C57BL/6 mice injected with turpentine or normal saline for 8 hours were euthanized after 8 hours. Livers were isolated and fixed with formaldehyde and embedded in paraffin. Animal care and experimental protocol were approved by our institutional ethics committee for animal experiments and the veterinary office (Geneva, Switzerland).
Quantitative real-time polymerase chain reaction
Total RNA was extracted from cells using the TRIzol reagent (Invitrogen, San Diego, CA), and treated by DNase (Ambion, Austin, TX). Reverse transcription was performed using equivalent volumes of random primers and oligo-DT using reverse transcriptase and RNasin treatment (Promega, Madison, WI). Quantitative real-time polymerase chain reaction (RT-PCR) was performed using the IQ5 thermocycler (Bio-Rad Laboratories, Hercules, CA). Sybrgreen (Bio-Rad) was used for the amplification of mouse md-2 cDNA (sense primer, 5′-ATG TTG CCA TTT ATT CTC TTT TCG ACG-3′; antisense primer, 5′-ATT GAC ATC ACG GCG GTG AAT GAT-3′) and β-actin (sense, 5′-GAG AGG GAA ATC GTG CGT GAC ATC-3′; antisense, 5′-GAA TGT AGT TTC ATG GAT GCC-3′) based on previously published work.5 When qPCR was performed with Sybrgreen, melting curves were performed to check for the presence of a single amplicon. The following TaqMan probes were used to detect amplification by qPCR of the following cDNAs: human md-2, Hs00209771_m1; human il-8, Hs00174103_m1; and human gapdh, Hs99999905_m1 (Applied Biosystems, Foster City, CA).
Immunohistochemistry
Paraffin-embedded liver sections (5 μm) were rehydrated using sequential Neo-clear (Merck, Whitehouse Station, NJ) and ethanol baths and were permeabilized for 30 minutes at room temperature using phosphate-buffered saline (PBS) containing 0.2% Triton X-100 (Sigma) and 0.5% human serum albumin (HAS; ZLB Behring, Bern, Switzerland). MD-2 immunodetection was performed using a 1:100 dilution of IMG-415, a monoclonal antibody (mAb)-recognizing mouse MD-2 (Biocarta, San Diego, CA), and mouse albumin using 1:200 dilution of affinity-purified goat-anti-mouse albumin antibody (Ab; A90-134A polyclonal Ab; Bethyl Laboratories, Inc, Montgomery, TX), in PBS containing 3% human serum albumin (ZLB Behring), followed by a 1:250 dilution of affinity-purified FITC-labeled anti-murine IgG secondary polyclonal antibody (Jackson ImmunoResearch Laboratories, West Grove, PA) and 1:500 dilution of affinity-purified, Texas Red–labeled anti-goat IgG secondary polyclonal antibody (Jackson ImmunoResearch Laboratories). For controls primary antibodies were substituted for their isotype controls (mouse IgG1; BD Biosciences, San Jose, CA, and goat IgGs, Santa Cruz Biotechnology, Santa Cruz, CA) at the same concentrations as primary antibodies. Liver sections were analyzed by confocal microscopy using a LSM-510 Meta microscope coupled to the LSM Image Browser 4.2 (Zeiss, Feldbach, Switzerland).
Transient transfection and reporter gene assay
One kilobase pair of the 5′ region of human md-2 gene (MD-2 promoter) was cloned from human genomic DNA into a pGL-3 luciferase reporter plasmid (Promega; pMD-2-Luc vector). Vectors were amplified using Ultra-efficient E coli (Invitrogen) and purified using HiSpeed plasmid purification kit (QIAGEN, Hilden, Germany). The pMD-2-Luc vector was transiently cotransfected with pRL-TK plasmid (Promega) in HepG2 cells using Fugene6 (Roche, Basel, Switzerland). After 24 hours, transfected cells were stimulated for 6 hours with IL-6, IL-1β, and dexamethasone. Firefly and Renilla reniformis luciferase luminescence was revealed using the Dual-Luciferase assay (Promega) and measured using a TD20/20 luminometer (Turner Design, Sunnyvale, CA). Luciferase activity was expressed as relative light intensity ratio of firefly over R reniformis luciferase activity.
Western blots
HepG2 cells (5 × 105) were seeded in each well of 6-well plates and grown to 60% confluence in RPMI medium containing 10% fetal calf serum (FCS). Culture medium was then replaced with RPMI containing 1% FCS, and cells were treated with IL-6, IL-1β, and dexamethasone. Conditioned supernatants were then collected and cells were immediately lysed in sodium dodecyl sulfate (SDS) loading buffer (Invitrogen). Proteins were separated using SDS gel in reducing conditions and electroblotted onto nitrocellulose membranes (Bio-Rad). Membranes were blocked 1 hour in pH 7.6 Tris-buffered saline containing 0.1% Tween 20 (TBST) and 5% human serum albumin (ZLB Behring). Membranes were then incubated overnight at 4°C in blocking buffer containing 0.8 μg/mL rabbit anti–human MD-2 FL-160 polyclonal antibody (Santa Cruz Biotechnology). Membranes were then incubated with 1/25 000 dilution of a horseradish peroxidase (HRP)-conjugated mouse anti–rabbit monoclonal antibody in TBST/5% nonfat dry milk (NFDM). Immunoblotted proteins were revealed using the SuperSignal West Femto maximum sensitivity substrate (Pierce, Rockford, IL) on films. Membranes were then stripped using 0.2% NaOH at room temperature for 4 minutes and reblocked 1 hour in TBST/5% HSA to be reblotted with anti-α-actin antibody (“housekeeping” protein for normalization the MD-2 signal in cell lysate). Stripped membranes were incubated with 0.2 ng/mL HRP-conjugated anti–human α-actin mAb C-2 (Santa Cruz) in TBST/5% NFDM. His-tagged and FLAG-tagged recombinant human soluble MD-2 (rhusMD-2) served as positive control. Immunoblotting with anti-MD-2 and anti-FLAG M2-HRP-conjugated mAb (Sigma-Aldrich) revealed the same single 23-kDa band. In cell lysate, the polyclonal anti-MD-2 antibody (FL160) revealed 3 immunoreactive bands: 17, 23, and 25 kDa, corresponding to MD-2 isoforms with various levels of glycosylation.16,19,36 The 23-kDa band was the only MD-2 isoform detected in HepG2 supernatant, corresponding exactly to the molecular mass of the rhusMD-2 band (data not shown).
Soluble MD-2 bioactivity assay
Soluble MD-2-dependent activation of TLR4-HEK293 by LPS has been described previously.32 Here, we used this assay to determine whether sMD-2 contained in HepG2 supernatants and detected by Western blot was bioactive (ie, supported the LPS activation of TLR4-HEK293 cells). A one-tenth dilution of HepG2 cell supernatant stimulated or unstimulated for 24 hours with IL-6, IL-1β, or dexamethasone was used in this assay. The MD-2-dependence of cell activation by LPS was tested using the 18H10 blocking anti-human MD-2 mAb (10 μg/mL).32 After 21 hours of LPS treatment (30 ng/mL) on TLR4-HEK293 cells, conditioned supernatants were collected and assayed for the production of IL-8 by enzyme-linked immunosorbent assay (ELISA; Pierce). The same assay was used to determine whether sMD-2 mediated bacterial activation of TLR4-expressing cells. In brief, TLR4-HEK293 cells were plated in 96-well plates and incubated for 21 hours at 37°C with 3.2 multiplicity of infection (MOI) heat-killed E coli wild type, E coli K12, S aureus, or 200 ng/mL K12 E coli LPS as a control, in the presence or absence of 1 μg/mL rhusMD-2. ELISA was used to measure IL-8 levels in conditioned supernatants.
sMD-2 binding to bacteria
Wild-type E coli and B subtilis bacteria were collected in their logarithmic phase of growth in Luria broth (LB), washed, heated for 30 minutes at 80°C, and finally resuspended in PBS. Heat-killed bacteria (107) were incubated with incremental concentrations of His-tagged rhusMD-2 or with an irrelevant His-tagged mouse IL-6 protein and incubated for 1 hour at room temperature. Bacteria were then washed once with PBS and incubated for 1 hour on ice with a mouse anti-polyHis mAb (QIAGEN), followed by a 1/200 dilution of an APC-conjugated goat anti-mouse IgG antibody (Molecular Probes, Leiden, the Netherlands) for 30 minutes on ice. Bacteria were finally analyzed by flow cytometry (FL-4 channel, FACScalibur; BD Biosciences).
Bactericidal test
E coli K12 were grown in LB at 37°C overnight, centrifuged, and resuspended to obtain an OD600nm of 0.05, corresponding to 2.5 × 107 colony-forming units/mL. rhusMD-2 (10 μg/mL) was added to the bacterial suspension and incubated on a rotating agitator at 37°C. Growth curves were determined by measuring hourly the OD600nm of bacterial suspension. Quantitative cultures of bacterial suspensions were also performed at various times using the serial dilution method by counting colony-forming units on solid agar plates.
Phagocytosis assay
The phagocytosis assay was adapted from previous studies.24,37,38 In brief, leukocytes from human heparinized blood obtained by venipuncture in healthy subjects were isolated using a gelatin gradient (Physiogel; Braun Medical, Emmenbrücke, Switzerland). Red blood cells were lysed with a 0.15 M ammonium chloride shock. Fluorescent E coli (5 × 108/mL; BODIPY FL bioparticules; Invitrogen) were incubated for 1 hour at 37°C in PBS containing 0.1% human serum albumin (ZLB Behring) with or without added rhusMD-2 (10 or 20 μg/mL), or in PBS supplemented with 2% normal human decomplemented plasma (opsonization period). In some experiments, an anti-TLR4 mAb (10 μg/mL) was added to the leukocytes before initiating the phagocytic assay. Bacteria were then centrifuged at 1000g for 15 minutes at 4°C and washed once in PBS. To test phagocytosis, 3 × 106 fluorescent E coli were added to 106 leukocytes, corresponding to a bacteria-to-cell ratio of 3:1. Phagocytosis was performed at 37°C for 5, 10, and 20 minutes, in the same buffers as those used for the opsonization period. Cells were then put on ice, centrifuged at 1000 rpm for 4 minutes at 4°C, washed once with ice-cold PBS, and resuspended in HBSS. To only quantify internalized E coli, extracellular fluorescence was quenched with 0.05% Trypan blue (Invitrogen).24,37,38 Polymorphonuclear neutrophil, monocyte, and lymphocyte populations were gated according to their forward and side-scatter characteristics, and their CD14 expression (PE-labeled anti-CD14 mAb; Sigma), and analyzed by flow cytometry (FL-1 channel, BD). In some conditions, 100 μM cytochalasin D (Sigma), a phagocytosis inhibitor, was added to leukocytes 1 hour before adding fluorescent E coli.38 The amount of phagocytosis was quantified using both “percentage of positive fluorescent cells” after trypan blue quenching, with a predefined M1 gate, and a phagocytic index (PI). PI was defined as follows: (geometric mean of fluorescence of gated cells × percentage of positive cells)/100, as described previously.38
Results
Liver MD-2 mRNA and protein synthesis after induction of an acute phase in mice
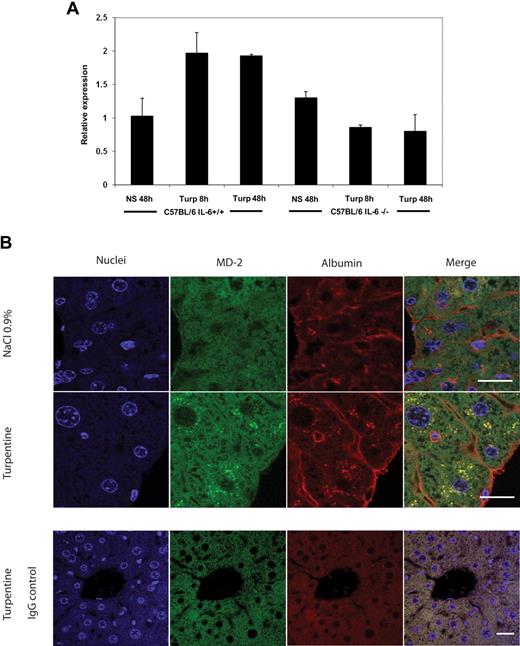
A classic acute-phase response was induced by paw injection of turpentine in C57BL/6 mice and in IL-6−/− mice on the C57BL/6 background.28 MD-2 mRNA (qPCR measurements of liver cDNA) increased 2-fold in liver from wild-type C57BL/6 mice harvested 8 and 24 hours after turpentine injection. IL-6−/− C57BL/6 mice failed to induce liver MD-2 mRNA expression (Figure 1A). A marked increase in the MD-2 signal in the perinuclear region of hepatocytes, consistent with a localization in the reticuloendoplasmic and Golgi apparatus was observed 8 hours after turpentine treatment of wild-type C57BL/6 mice (Figure 1B). The cellular origin of MD-2 in liver during acute phase was the hepatocyte, because it colocalized with albumin (Figure 1B). No staining was observed with isotype controls after turpentine treatment, showing the specificity of the MD-2 and albumin staining (Figure 1B). These experiments indicated that hepatocytes in vivo responded to the induction of an acute phase by increasing both MD-2 mRNA and protein, a response that was IL-6–dependent.
MD-2 is up-regulated in the liver from turpentine-treated mice and is dependent on IL-6. (A) MD-2 mRNA levels were measured in liver from C57BL/6 IL-6+/+ and C57BL/6 IL-6−/− mice 8 and 48 hours after paw injection of turpentine (turp) or normal saline (NS). Messenger RNA levels were measured by quantitative RT-PCR. Mean plus or minus SD MD-2 mRNA levels were normalized with the expression β-actin mRNA and expressed as arbitrary units. One experiment, 3 animals per group. (B) The MD-2 protein (green) is increased in liver from C57BL/6 wild type mice treated 8 hours with turpentine compared with mice treated with normal saline (NaCl 0.9%). MD-2 is up-regulated by hepatocytes because it colocalizes (merge, yellow) with albumin (red). The increased fluorescence is located in the perinuclear region of hepatocytes. No specific staining was observed with isotype controls in liver from turpentine-treated animals (bottom row). Bar equals 20 μm. Results were similar in 6 animals (3 per group).
MD-2 is up-regulated in the liver from turpentine-treated mice and is dependent on IL-6. (A) MD-2 mRNA levels were measured in liver from C57BL/6 IL-6+/+ and C57BL/6 IL-6−/− mice 8 and 48 hours after paw injection of turpentine (turp) or normal saline (NS). Messenger RNA levels were measured by quantitative RT-PCR. Mean plus or minus SD MD-2 mRNA levels were normalized with the expression β-actin mRNA and expressed as arbitrary units. One experiment, 3 animals per group. (B) The MD-2 protein (green) is increased in liver from C57BL/6 wild type mice treated 8 hours with turpentine compared with mice treated with normal saline (NaCl 0.9%). MD-2 is up-regulated by hepatocytes because it colocalizes (merge, yellow) with albumin (red). The increased fluorescence is located in the perinuclear region of hepatocytes. No specific staining was observed with isotype controls in liver from turpentine-treated animals (bottom row). Bar equals 20 μm. Results were similar in 6 animals (3 per group).
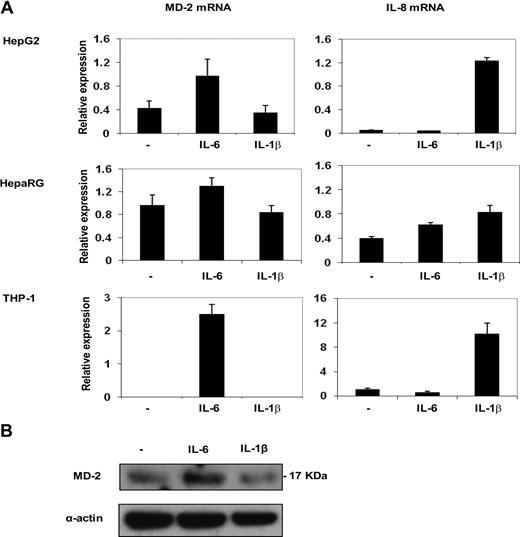
Human MD-2 expression was regulated by IL-6 but not by IL-1β
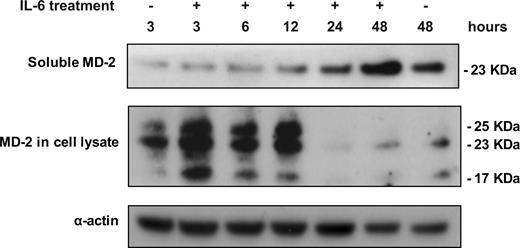
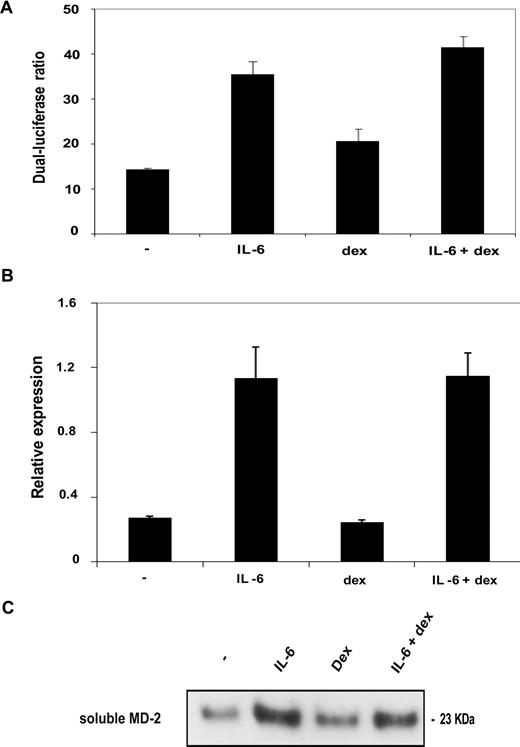
To confirm that MD-2 behaved as an acute-phase protein (APP), human hepatocytic cell lines were stimulated with IL-6 and IL-1β. Traditionally, both cytokines up-regulate type I APPs, whereas types II APPs respond only to IL-6.29 Both MD-2 mRNA and MD-2 protein in cell lysate were induced after 6-hour stimulation by IL-6 in HepG2 and HepaRG cell lines, as well as in the promonocytic cell line THP-1 (Figure 2A,B). Whereas IL-1β was able to stimulate cells to express IL-8, it induced neither MD-2 mRNA nor protein. A time course of IL-6 stimulation of HepG2 cells showed that maximal cellular MD-2 production started at 3 hours, reached a plateau between 6 and 12 hours, and then decreased (Figure 3). Soluble MD-2 secretion started after 12 hours of IL-6 stimulation and was maximal after 48 hours (Figure 3). Unstimulated HepG2 cells constitutively secreted a small amount of sMD-2 (Figure 3), but THP-1 cells did not (data not shown). Similar results were obtained in HepG2 cells stimulated with IL-6 when measuring either endogenous MD-2 mRNA or MD-2 promoter activity (Figure 4, A,B). Glucocorticoids have been shown to modulate IL-6-dependent production of some APPs. In the case of MD-2, dexamethasone did not stimulate the expression of MD-2 mRNA, did not increase MD-2 promoter activity in HepG2 cells, and did not influence sMD-2 protein secretion (Figure 4). Dexamethasone did not synergize with IL-6 either (Figure 4).
MD-2 expression is up-regulated by IL-6 but not IL-1β. (A) MD-2 mRNA and IL-8 mRNA levels in HepG2, HepaRG, and THP-1 cells stimulated for 6 hours with 10 ng/mL IL-6 and 1 ng/mL IL-1β. Messenger RNA levels were measured by quantitative RT-PCR. Mean plus or minus SD MD-2 mRNA levels were normalized with the expression of GAPDH mRNA and expressed as arbitrary units. This experiment was performed in triplicates and representative of 3 different experiments. (B) Western blot of MD-2 protein (17 kDa) in whole cell lysates from HepG2 cells stimulated with IL-6 and IL-1β. This experiment is representative of 3 different experiments.
MD-2 expression is up-regulated by IL-6 but not IL-1β. (A) MD-2 mRNA and IL-8 mRNA levels in HepG2, HepaRG, and THP-1 cells stimulated for 6 hours with 10 ng/mL IL-6 and 1 ng/mL IL-1β. Messenger RNA levels were measured by quantitative RT-PCR. Mean plus or minus SD MD-2 mRNA levels were normalized with the expression of GAPDH mRNA and expressed as arbitrary units. This experiment was performed in triplicates and representative of 3 different experiments. (B) Western blot of MD-2 protein (17 kDa) in whole cell lysates from HepG2 cells stimulated with IL-6 and IL-1β. This experiment is representative of 3 different experiments.
IL-6 up-regulates soluble MD-2 production and secretion by HepG2 cells. HepG2 cells were stimulated with IL-6 for 3, 6, 12, 24, and 48 hours. Western-blot of sMD-2 in HepG2 supernatants (23 kDa), MD-2 in HepG2 cell lysates (17, 23, 25 kDa), and α-actin as a loading control. This experiment is representative of 3 different experiments.
IL-6 up-regulates soluble MD-2 production and secretion by HepG2 cells. HepG2 cells were stimulated with IL-6 for 3, 6, 12, 24, and 48 hours. Western-blot of sMD-2 in HepG2 supernatants (23 kDa), MD-2 in HepG2 cell lysates (17, 23, 25 kDa), and α-actin as a loading control. This experiment is representative of 3 different experiments.
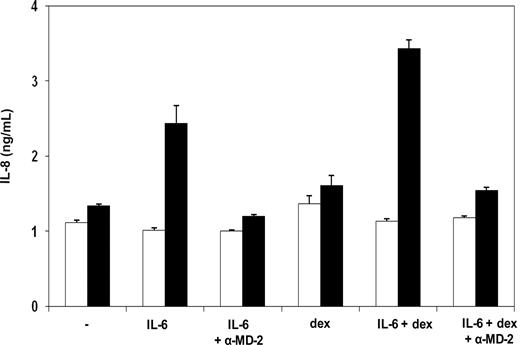
MD-2 expression is not regulated by dexamethasone in HepG2 cells. (A) Effect of IL-6 and dexamethasone on the expression of a luciferase reporter gene driven by the MD-2 promoter transfected in HepG2 cells. HepG2 cells transfected with an MD-2 promoter driving the firefly luciferase reporter gene were stimulated for 6 hours with IL-6 (10 ng/mL) and dexamethasone (dex, 10 μM). Firefly luciferase activity was normalized with renilla luciferase activity. Mean values plus or minus SD are shown. This experiment was performed in triplicates and is representative of 3 different experiments. (B) Effect of IL-6 and dexamethasone on the expression of MD-2 mRNA in HepG2 cells. MD-2 mRNA expression (normalized with GAPDH mRNA) was measured by quantitative RT-PCR in HepG2 cells stimulated for 6 hours with IL-6 (10 ng/mL) and dexamethasone (dex, 10 μM). Mean values plus or minus SD are shown. This experiment was performed in triplicates and is representative of 3 different experiments. (C) Effect of IL-6 and dexamethasone on the secretion of sMD-2 protein by HepG2 cells. Western blot of sMD-2 (23 kDa) in supernatant of HepG2 cells stimulated for 24 hours with IL-6 (10ng/mL) and dexamethasone (10μM). This experiment was performed in triplicates and is representative of 3 different experiments.
MD-2 expression is not regulated by dexamethasone in HepG2 cells. (A) Effect of IL-6 and dexamethasone on the expression of a luciferase reporter gene driven by the MD-2 promoter transfected in HepG2 cells. HepG2 cells transfected with an MD-2 promoter driving the firefly luciferase reporter gene were stimulated for 6 hours with IL-6 (10 ng/mL) and dexamethasone (dex, 10 μM). Firefly luciferase activity was normalized with renilla luciferase activity. Mean values plus or minus SD are shown. This experiment was performed in triplicates and is representative of 3 different experiments. (B) Effect of IL-6 and dexamethasone on the expression of MD-2 mRNA in HepG2 cells. MD-2 mRNA expression (normalized with GAPDH mRNA) was measured by quantitative RT-PCR in HepG2 cells stimulated for 6 hours with IL-6 (10 ng/mL) and dexamethasone (dex, 10 μM). Mean values plus or minus SD are shown. This experiment was performed in triplicates and is representative of 3 different experiments. (C) Effect of IL-6 and dexamethasone on the secretion of sMD-2 protein by HepG2 cells. Western blot of sMD-2 (23 kDa) in supernatant of HepG2 cells stimulated for 24 hours with IL-6 (10ng/mL) and dexamethasone (10μM). This experiment was performed in triplicates and is representative of 3 different experiments.
Soluble MD-2 produced by IL-6-stimulated HepG2 cells was bioactive
We next tested whether soluble MD-2 produced by IL-6-treated HepG2 cells supported the activation of TLR4-HEK293 cells by LPS and by Gram-negative bacteria.32 Supernatants of HepG2 cells stimulated with IL-6 consistently increased levels of IL-8 in LPS-treated TLR4-HEK293 cells (Figure 5). This effect was blocked by an anti-huMD-2 mAb.
Soluble MD-2 secreted by HepG2 cells is bioactive. TLR4-HEK293 cells were stimulated with LPS (filled bars) or not (empty bars) in the presence of supernatants from HepG2 cells stimulated for 24 hours with IL-6 (10 ng/mL) and dexamethasone (10 μM). In some conditions, the 18H10 anti-huMD-2 blocking monoclonal antibody (α-MD-2) was added to cell cultures. IL-8 production by TLR4-HEK293 cells was measured in conditioned supernatant by ELISA. Bars correspond to mean values of 5 independent experiments performed in duplicate. Values are expressed as mean plus or minus SEM.
Soluble MD-2 secreted by HepG2 cells is bioactive. TLR4-HEK293 cells were stimulated with LPS (filled bars) or not (empty bars) in the presence of supernatants from HepG2 cells stimulated for 24 hours with IL-6 (10 ng/mL) and dexamethasone (10 μM). In some conditions, the 18H10 anti-huMD-2 blocking monoclonal antibody (α-MD-2) was added to cell cultures. IL-8 production by TLR4-HEK293 cells was measured in conditioned supernatant by ELISA. Bars correspond to mean values of 5 independent experiments performed in duplicate. Values are expressed as mean plus or minus SEM.
Soluble MD-2 bound to Gram-negative bacteria but was not bactericidal
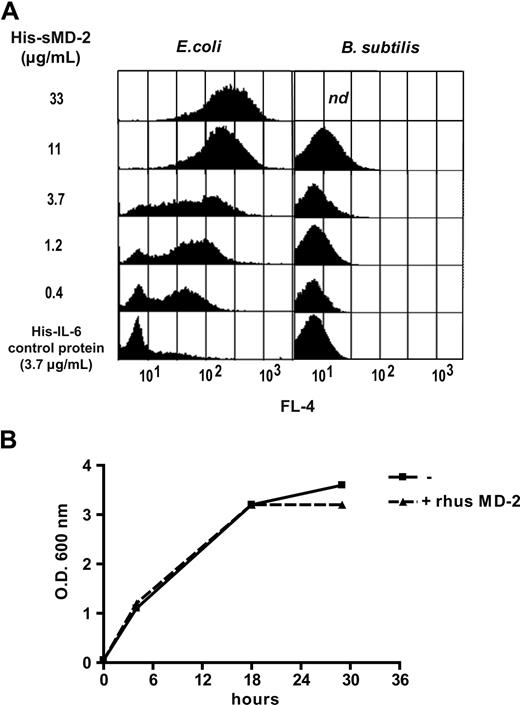
Recombinant husMD-2 bound to E coli in a dose-dependent manner, but not to Gram-positive B subtilis (Figure 6A). No binding to bacteria was observed with an irrelevant HIS-tagged protein. Even though rhusMD-2 bound to live E coli, it did not influence bacterial growth, even at a concentration of 10 μg/mL, showing that MD-2 did not have a bactericidal effect (Figure 6B). Results with E coli growth curves were confirmed using quantitative cultures (data not shown).
Recombinant human soluble MD-2 binds to E coli but has no bactericidal effect. (A) Soluble MD-2 binding to E coli and B subtilis. Wild-type heat-killed E coli (left) and B subtilis (right) were incubated with increasing concentrations of His-tagged recombinant human sMD-2. Soluble MD-2 binding to bacteria was measured by FACS using an APC-conjugated monoclonal anti-polyHis antibody detecting MD-2 bound to bacteria. A negative control was an irrelevant His-tagged protein (murine IL-6). This is one experiment representative of 3 similar experiments; n.d. indicates not done. (B) Soluble MD-2 does not influence the growth of E coli. E coli K12 were cultured in the presence or absence of 10 μg/mL recombinant human soluble MD-2. Bacterial growth was determined using OD600 absorbance of the culture medium. This experiment was repeated twice with the same results.
Recombinant human soluble MD-2 binds to E coli but has no bactericidal effect. (A) Soluble MD-2 binding to E coli and B subtilis. Wild-type heat-killed E coli (left) and B subtilis (right) were incubated with increasing concentrations of His-tagged recombinant human sMD-2. Soluble MD-2 binding to bacteria was measured by FACS using an APC-conjugated monoclonal anti-polyHis antibody detecting MD-2 bound to bacteria. A negative control was an irrelevant His-tagged protein (murine IL-6). This is one experiment representative of 3 similar experiments; n.d. indicates not done. (B) Soluble MD-2 does not influence the growth of E coli. E coli K12 were cultured in the presence or absence of 10 μg/mL recombinant human soluble MD-2. Bacterial growth was determined using OD600 absorbance of the culture medium. This experiment was repeated twice with the same results.
sMD-2 was a cofactor for the activation of TLR4-expressing cells to Gram-negative bacteria
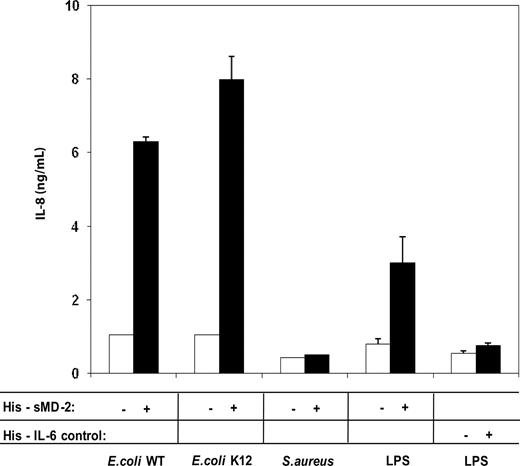
We next investigated whether sMD-2 modulated cell activation by bacteria. Heat-killed Gram-negative and Gram-positive bacteria were coincubated with soluble recombinant human sMD-2 and cultured with TLR4-HEK293 cells (Figure 7). Soluble MD-2 supported cell activation to wild-type E coli and E coli K12 but not to S aureus. These results indicated that sMD-2 was an essential cofactor for the activation of TLR4-expressing cells to Gram-negative but not to Gram-positive bacteria. As little as 0.1 μg/mL recombinant human sMD-2 was sufficient to support cell activation in the presence of Gram-negative bacteria (data not shown).
Soluble MD-2 enhances TLR4-expressing cell response to whole Gram-negative, but not Gram-positive bacteria. TLR4-HEK293 cells were cultured with 3.2 multiplicity of infection (MOI) heat inactivated bacteria (E coli K12, E coli wild type, S aureus, and E coli K12 LPS as a positive control) in the presence (filled bars) or absence (empty bars) of 1 μg/mL polyHis-tagged recombinant human soluble MD-2 or an irrelevant poly-His-tagged protein (murine IL-6). IL-8 secretion in conditioned supernatants was measured by ELISA. Mean values plus or minus SD are shown. This is one representative experiment of 3 experiments.
Soluble MD-2 enhances TLR4-expressing cell response to whole Gram-negative, but not Gram-positive bacteria. TLR4-HEK293 cells were cultured with 3.2 multiplicity of infection (MOI) heat inactivated bacteria (E coli K12, E coli wild type, S aureus, and E coli K12 LPS as a positive control) in the presence (filled bars) or absence (empty bars) of 1 μg/mL polyHis-tagged recombinant human soluble MD-2 or an irrelevant poly-His-tagged protein (murine IL-6). IL-8 secretion in conditioned supernatants was measured by ELISA. Mean values plus or minus SD are shown. This is one representative experiment of 3 experiments.
sMD-2 was an opsonin for Gram-negative bacteria
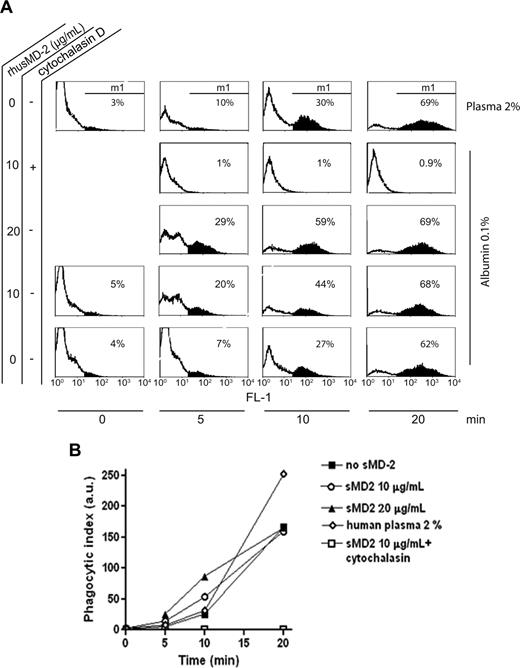
To test whether sMD-2 behaved as an opsonin, fluorescent E coli were incubated with freshly isolated human circulating leukocytes. Cells were incubated with 0.1% human serum albumin (corresponding to a 2% plasma concentration), with the addition of either 10 or 20 μg/mL rhusMD-2. The addition at the end of the incubation period of Trypan blue (quenching the extracellular fluorescence) allowed us to quantify only the intracellular (internalized) fluorescent E coli. Soluble MD-2 increased the rate of E coli phagocytosis by polymorphonuclear neutrophils (Figure 8). In 4 independent experiments with 3 different blood donors, the addition of 10 or 20 μg/mL sMD-2 to fluorescent E coli increased the rate of bacterial phagocytosis by polymorphonuclear neutrophils. This enhancing effect was maximal between 5 and 10 minutes after exposure of E coli to phagocytes. This opsonization effect of sMD-2 was similar to that measured with normal human plasma at least for these short incubation times. After a 10-minute incubation of fluorescent E coli with leukocytes, the PI in neutrophils was 21 (± 4) arbitrary units (a.u.) in a buffer containing albumin versus 63.8 (± 26) a.u. with the addition of 20 μg/mL rhusMD-2 (p = .046, paired t test, based on 3 independent experiments). TLR4 blockade markedly decreased sMD-2-dependent phagocytosis of fluorescent E coli at the 5- and 10-minute time points (93% and 81% PI inhibition, respectively), an effect that was lost after 20 minutes. After 10 minutes, the PI of monocytes and the percentage of fluorescent monocytes (FM) were slightly increased with the addition of sMD-2 (albumin, no sMD-2: PI = 245 and 44% FM; 10 μg/mL sMD-2: PI = 302 and 52% FM; 20 μg/mL sMD-2: PI = 334 and 53% FM; 2% plasma: PI = 291 and 48% FM; 10 μg/mL sMD-2 in the presence of cytochalasin D: PI = 0.59 and 0.6% FM). No phagocytosis was observed in lymphocytes, irrespective of the presence or absence of sMD-2 or plasma (data not shown). In all conditions, phagocytosis was maximal after 20 minutes and entirely inhibited by cytochalasin D at all time points. Taken together, these results indicated that sMD-2 bound to Gram-negative bacteria increased the amount and accelerated the rate of internalization of Gram-negative bacteria by professional phagocytes such as polymorphonuclear neutrophils and monocytes, a classic characteristic of opsonins.
Soluble MD-2 enhances the phagocytosis of Gram-negative bacteria by polymorphonuclear neutrophils. Fluorescent E coli were incubated with freshly isolated human circulating leukocytes for 5, 10 and 20 minutes in 2% plasma or in the presence of absence of 10 or 20 μg/mL of recombinant human soluble MD-2 in albumin 0.1%. Polymorphonuclear neutrophils were gated by FACS according to their forward and side-scatter characteristics and CD14 expression. At the end of incubation times, extracellular fluorescence was quenched using Trypan blue. The percentage of cells becoming fluorescent (E coli internalization) was determined using another gate (M1). The geometric mean of cells becoming fluorescent was also measured. Cytochalasin D was used as an inhibitor of phagocytosis. Representative experiments of 4 similar experiments performed with 3 different blood donors. (A) Flow cytometric analysis of fluorescent E coli phagocytosis by human polymorphonuclear neutrophils. (B) Time course of phagocytosis of fluorescent E coli by polymorphonuclear neutrophils expressed as a phagocytic index (PI). The PI was defined as follows: (geometric mean of fluorescence of m1-gated cells x percent positive cells)/100. 0.1% human serum albumin (HSA) only (no sMD-2), ■; 10 μg/mL sMD-2 in 0.1% HSA, ○; 20 μg/mL in 0.1% HSA, ▴; 2% human plasma, ◇; 10 μg/mL sMD-2 in 0.1% HSA and cytochalasin D, □.
Soluble MD-2 enhances the phagocytosis of Gram-negative bacteria by polymorphonuclear neutrophils. Fluorescent E coli were incubated with freshly isolated human circulating leukocytes for 5, 10 and 20 minutes in 2% plasma or in the presence of absence of 10 or 20 μg/mL of recombinant human soluble MD-2 in albumin 0.1%. Polymorphonuclear neutrophils were gated by FACS according to their forward and side-scatter characteristics and CD14 expression. At the end of incubation times, extracellular fluorescence was quenched using Trypan blue. The percentage of cells becoming fluorescent (E coli internalization) was determined using another gate (M1). The geometric mean of cells becoming fluorescent was also measured. Cytochalasin D was used as an inhibitor of phagocytosis. Representative experiments of 4 similar experiments performed with 3 different blood donors. (A) Flow cytometric analysis of fluorescent E coli phagocytosis by human polymorphonuclear neutrophils. (B) Time course of phagocytosis of fluorescent E coli by polymorphonuclear neutrophils expressed as a phagocytic index (PI). The PI was defined as follows: (geometric mean of fluorescence of m1-gated cells x percent positive cells)/100. 0.1% human serum albumin (HSA) only (no sMD-2), ■; 10 μg/mL sMD-2 in 0.1% HSA, ○; 20 μg/mL in 0.1% HSA, ▴; 2% human plasma, ◇; 10 μg/mL sMD-2 in 0.1% HSA and cytochalasin D, □.
Discussion
Herein, we show that sMD-2 is a novel type II APP and an opsonin for Gram-negative bacteria. APPs are defined as plasma proteins produced by the liver, with levels increasing during inflammatory diseases by at least 25% of their normal levels.29,39 An important increase in levels of some of these APPs has been reported during severe infections and sepsis.29 Many of these proteins play an important role in the so-called stress response and in the innate immune response to bacteria.40 They are classified as type I and II APPs. Classic type I APPs, such as the C-reactive protein (CRP) and the serum amyloid A (SAA) protein, are up-regulated by IL-6 and IL-1β, frequently in a synergistic manner.41 Type II APPs, such as fibrinogen and α2-microglobulin, are regulated by IL-6, but not by IL-1β.29 It is noteworthy that 2 proteins binding Gram-negative bacterial LPS are APPs: LBP (a type I APP) and soluble CD14 (a type II APP).27,28
The glycoprotein MD-2 is usually coexpressed with TLR4, the signaling component of the LPS receptor, and binds TLR4 at the surface of various cell types.42 MD-2 may play a role in the trafficking of TLR4 to the cell surface, at least in murine cells.5 Other molecules may participate in the surface expression of TLR4.43,–45 MD-2 binds LPS with high affinity and is essential to confer LPS responsiveness to TLR4-expressing cells.46,47 The MD-2 crystal structure was recently published.13,14 These studies showed that Lipid IVa and the LPS antagonist eritoran insert into a hydrophobic pocket. However, the exact interaction between a “wild-type” hexa-acylated LPS and MD-2 remains unknown. The MD-2 epitopes binding to TLR4 were also identified.13,14
A soluble form of MD-2 has also been detected in culture supernatants of cells expressing MD-2.17 It possesses a classic N-terminal signal peptide for secreted proteins, but its secretory pathway remains largely unknown.2 Hepatocytic cells, such as HepG2 cells, were shown to produce small amounts of TLR4 mRNA but do not express TLR4 at the cell surface.48 It is therefore conceivable that a differential expression of TLR4 and MD-2 may exist in some cell types and that sMD-2 may be secreted in the absence of TLR4 expression.
Previous work has shown that MD-2 activity32 and protein33 was increased in plasma from patients with severe sepsis and septic shock. In the present study, we demonstrate that the expression of sMD-2 is regulated in hepatocytic cells by IL-6, but not IL-1β, at both mRNA and protein levels. MD-2 mRNA was also up-regulated by IFN-γ in gut epithelial cells.49 We show that the increased liver MD-2 mRNA measured in mice treated with the APP-inducer turpentine was not present in IL-6−/− littermates. These findings, together with the kinetics of secretion of sMD-2, qualify sMD-2 as a type II APP. The primary site of this induction of sMD-2 production is likely to be the liver, given that (1) sMD-2 behaves like an APP and (2) we observed a marked increase in MD-2 production by hepatocytes both in vitro and in vivo after the induction of an acute phase. Further studies are needed to determine whether an acute phase induces MD-2 up-regulation in organs other than the liver. It is noteworthy that human promonocytic THP-1 cells also responded to IL-6 by increasing MD-2 mRNA levels. It has been shown that an extrahepatic production of APPs can occur, such as in the lung50,–52 ; alveolar macrophages can produce C-reactive protein and LBP, for example.53 It is conceivable that sMD-2, found in large quantities in lung edema fluid from patients with the acute respiratory distress syndrome,32 may also be produced in organs other than the liver to participate in local innate immune defense against bacteria. This has been proposed for LBP, another locally produced APP and opsonin with LPS-binding properties.54
It has been suggested that sMD-2 may act, at high concentration, as a sink for LPS, and inhibit cell activation by endotoxin, in a fashion similar to that reported with high concentrations of LBP and soluble CD14.34,55,–57 Based on the known roles of other APPs and the LPS-binding properties of MD-2, several alternate functions of sMD-2 were considered and tested in the present study. Soluble MD-2 enhanced the activation of cells expressing TLR4, not only to purified LPS, but also to whole Gram-negative bacteria. The critical role of MD-2 in human cell activation by whole Gram-negative bacteria has recently been reported.35
We also showed that binding of sMD-2 to Gram-negative bacteria enhanced their phagocytosis by professional phagocytes such as polymorphonuclear neutrophils and monocytes. This enhancement in the phagocytic process was even more pronounced than that recently described with another APP, serum amyloid protein A.24 This novel function of soluble MD-2 as an opsonin is reminiscent of that of the acute-phase reactant LBP.23,58 Interestingly, we found that TLR4 blockade inhibited sMD-2-dependent phagocytosis by neutrophils, at least at early time points (5 and 10 minutes). At a later time point (20 minutes), neither the addition of sMD-2 nor TLR4 antagonism influenced the phagocytic process. This suggests that proteins other than sMD-2 and TLR4 participate in opsonization and internalization of Gram-negative bacteria by human phagocytes. LBP, complement and complement receptors, SAA, mannose-binding protein, sCD14 and mCD14 are likely candidates. We propose that sMD-2 acts as a soluble innate molecule sensing the presence of LPS-bearing bacteria in acute phase plasma or in other body fluids at the site of infection. The binding of sMD-2 to Gram-negative bacteria triggers and enhances both TLR4-expressing cell activation and phagocytosis during the early phase of phagocytosis. We have not tested whether Gram-negative bacterial internalization by endothelial and epithelial cells can be mediated by sMD-2. Some of these cells express TLR4 intracellularly. It is a possibility that, in these cell types, cell activation could be mediated by internalized bacteria opsonized by sMD-2 and sensed by TLR4 intracelullarly.59,–61 The opsonic activity of plasma for Gram-negative bacteria is a complex process involving several proteins, such as natural antibodies, complement, SAA, LBP, and possibly sMD-2. In the present study, we did not test the relative participation of sMD-2 in the opsonic activity of whole plasma, because a specific antibody blocking sMD-2 was not available. Finally, because the quaternary structure of sMD-2 in various fluids is largely unknown, it is difficult to speculate on the relationship between sMD-2 concentrations measured in plasma19 and those used in our in vitro studies. Active sMD-2 monomers represented ∼ 1% of the recombinant sMD-2 used in our experiments, the rest being sMD-2 multimers (data not shown). This nanomolar rhusMD-2 monomer concentration would be in accordance with levels measured by ELISA in plasma from septic patients.33 Further studies are needed to determine the proportion of monomeric vs. multimeric sMD-2 in human body fluids such as plasma.
Interestingly, several APPs share anti-bacterial functions and participate in innate immune response. As mentioned earlier, SAA is a type I APP, an opsonin for bacteria and has chemotactic properties.24,62 The mannose-binding lectin is a type II APP, an opsonin for a wide variety of microorganisms, and initiates the complement cascade.63,64 LBP is a type I APP, an opsonin for Gram-negative bacteria and a sensor for LPS to activate innate immune cells.1,23,27 Soluble CD14 is a type II APP and mediates LPS activation of CD14-negative cells.28,65
Other soluble molecules of the innate immunity have direct bactericidal effects. This is the case for bactericidal permeability-increasing (BPI) protein, cathelicidins, defensins lysozyme, and complement, for example.26,66,–68 We were unable to demonstrate a direct bactericidal effect of sMD-2 on Gram-negative bacteria. Some of these molecules, such as cathelicidins, defensins, and proteins of the complement system, are potent chemotactic molecules for blood leukocytes.69 This potential function of sMD-2 was not tested in the present work.
In summary, we show that, in addition to its role as a cell surface LPS-binding protein mediating cell activation, MD-2, in its soluble form, is a type II APP and opsonizes Gram-negative bacteria. Soluble MD-2 bound to Gram-negative bacteria mediates TLR4-expressing cell activation and enhanced the phagocytosis of opsonized bacteria, 2 essential functions of innate immunity. Our results suggest that sMD-2 plays a pivotal role in host-pathogen interactions and potentially in the pathogenesis of severe bacterial infections such as severe sepsis and septic shock.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank C. Gabay, University of Geneva, for providing us with mouse liver cDNA; R. Genolet, K. Perron, and T. Araud (University of Geneva) for stimulating discussions; and C. Deffert (University of Geneva) for her expert technical help with mice experiments.
This work was supported by research grants from the Roche Research Foundation (grant 12-2005), the Novartis Consumer Health Foundation, the Boninchi Foundation, and the Swiss National Foundation for Scientific Research (grant 3200B0-105770).
Authorship
Contribution: P.T. designed the research, performed experiments, analyzed the results, made figures, and wrote the manuscript; I.D-S. designed the research, performed experiments, and made figures; M.S. and R.C. performed experiments; G.E. contributed vital reagents; V.N. designed and performed experiments; and J.P. designed experiments, analyzed the results, and wrote the manuscript.
Conflict-of-interest disclosure: G.E. is an employee of NovImmune SA Geneva, Switzerland, whose potential products, anti-huMD-2 (18H10) and anti-huTLR4 (15C1) mAbs, were used in this work. The other authors declare no competing financial interests.
Correspondence: Prof. Jérôme Pugin, MD, Service des Soins Intensifs, Hôpitaux Universitaires de Genève, 24, rue Micheli-du-Crest, CH-1211 Geneva 14, Switzerland; e-mail: jerome.pugin@medecine.unige.ch.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal