Several hematopoietic stem-cell (HSC) regulators are controlled by ubiquitin-mediated proteolysis, so the ubiquitin pathway might modulate HSC function. However, this hypothesis has not been formally tested. Cul4A encodes a core subunit of one ubiquitin ligase. Whereas Cul4A-deficient embryos die in utero, Cul4A-haploinsufficient mice are viable but exhibit abnormal hematopoiesis (fewer erythroid and primitive myeloid progenitors). Given these data, we examined whether Cul4A+/− HSCs might also be impaired. Using bone marrow transplantation assays, we determined that Cul4A+/− HSCs exhibit defects in engraftment and self-renewal capacity. These studies are the first to demonstrate that ubiquitin-mediated protein degradation is important for HSC function. Further, they indicate that a Cul4A ubiquitin ligase targets for degradation one or multiple HSC regulators.
Introduction
Multiple regulators of hematopoietic stem-cell (HSC) function are degraded by the proteasome, including HoxA9, Gfi-1, MEF/ELF4, c-kit receptor, STAT3, β-catenin, and p21Cip1.1,,,,,–7 Notch1, another HSC regulator, modulates ubiquitination.2,8 Together, these findings suggest ubiquitin-mediated proteolysis regulates normal HSC function. Since this hypothesis has not been formally tested, we used bone marrow transplantation assays to determine in vivo whether Cul4A, which mediates ubiquitination, is required for HSC function.
Ubiquitin ligases control which proteins are degraded by the proteasome.9 They contain one or more subunits, and all contain either a HECT or a RING protein motif. Cullin-RING ubiquitin ligases, the largest known class, contain a cullin subunit with 7 known in mammals. Previous studies by our group and others showed that the Cul4A cullin ubiquitin ligase regulates proliferation and differentiation in maturing myeloid10,11 and erythroid cells.12 Cul4A is required for normal development, since Cul4A−/− mouse embryos die in utero.13 Cul4A+/− mice are viable, expressing half the wild-type level of Cul4A. Yet, they have fewer erythroid and multipotential myeloid progenitors (greater than 5-fold and 3-fold fewer, respectively) and fewer spleen colony-forming units in vivo, indicating that Cul4A is required for progenitor homeostasis.10,12 Therefore, given the requirement of Cul4A for normal hematopoiesis in progenitors and during terminal differentiation, we evaluated whether Cul4A+/− HSC function is altered using bone marrow transplantation assays.
Materials and methods
All animal procedures were approved by the IUSM IACUC. Mice were generated as described.13,14 Immunoblots, competitive repopulations, serial transplantations, and limiting-dilution competitive repopulating unit (CRU) assays were conducted as described.12,,–15 Student t test was used for statistical analyses.
Results and discussion
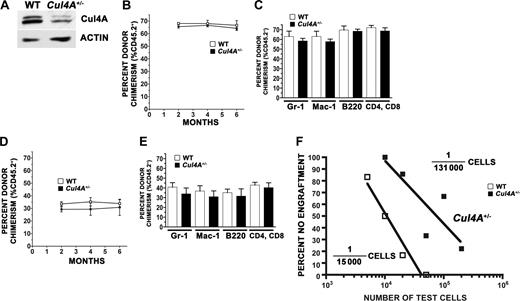
Insufficient Sca-1+c-Kit+Lin− cells, a phenotypically defined HSC population, were obtained to detect Cul4A protein, but from Lin− cells, a population enriched for HSCs, Cul4A in Cul4A+/− cells was one half that in controls (Figure 1 A). However, the frequency of Sca-1+c-Kit+Lin− cells among bone marrow low-density mononuclear cells (LDMNCs) from Cul4A+/− was the same as wild type (0.26% ± 0.03% and 0.28% ± 0.05%, respectively). Therefore, equal numbers of Cul4A+/− and wild-type bone marrow LDMNCs were compared in competitive repopulation assays.
Cul4A+/− HSCs exhibit an engraftment defect. (A) Expression of Cul4A protein in Lin− LDMNCs. LDMNCs were isolated from Cul4A+/− and wild-type littermates, and Lin− cells were obtained by negative selection (Lineage Cell Depletion Kit; Miltenyi Biotec, Auburn, CA). Cell lysates were prepared and analyzed by immunoblot as described.12,13 Quantitation of scanned film was performed using ImageJ (http://rsb.info.nih.gov/ij/; National Institutes of Health, Bethesda, MD) and normalized for β-actin loading. (B) Competitive repopulation with a 1:1 ratio of test donor cells and competitors; overall percentage donor chimerism. For Cul4A+/− or wild-type donors (C57BL/6), 5 × 105 bone marrow LDMNCs (CD45.2+) were mixed with 5 × 105 wild-type competitor cells (B6.BoyJ, CD45.1+) and transplanted into 5 to 6 lethally irradiated wild-type recipients (CD45.1+) by tail vein injection. Overall engraftment (percentage CD45.2+) for Cul4A+/− (■) or wild-type (□) test cells was measured 2 to 6 months after transplantation by flow cytometric analysis of peripheral blood with anti-CD45.1 or anti-CD45.2 antibodies conjugated with fluorescein isothiocyanate (FITC; Pharmingen, San Diego, CA). (C) Engraftment into myeloid and lymphoid lineages. For the transplantation described in panel B, engraftment of Cul4A+/− or wild-type test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was also measured using biotin-conjugated anti-Gr-1, -Mac-1, -B220, or both -CD4 and -CD8 antibodies, respectively, and then streptavidin-APC secondary antibody (Pharmingen), each in combination with the anti-CD45.1 and -CD45.2 antibodies described for panel B. Percentage CD45.2+ for Cul4A+/− (■) or wild-type (□) test cells is graphed for each lineage 6 months after transplantation. (D) Competitive repopulation with a 1/3:1 ratio of test donor cells and competitors; overall percentage donor chimerism. For Cul4A+/− or wild-type donors, 1.7 × 105 bone marrow LDMNCs were mixed with 5 × 105 wild-type competitors in a competitive repopulation analogous to that described for panel B. Overall engraftment was determined in the same way, and graphed for Cul4A+/− (■) or wild-type (□) test cells 2 to 6 months after transplantation. (E) Engraftment into myeloid and lymphoid lineages for test cells mixed 1/3:1 with competitors. For the competitive repopulation described in panel D, percentage CD45.2+ for Cul4A+/− (filled bars) or wild-type (open bars) test cells was determined as described in panel C and graphed for each lineage 6 months after transplantation. For panels B-E, mean (± SEM) is graphed. (F) Limiting dilution. From 5 × 103 to 2 × 105Cul4A+/− bone marrow LDMNCs and 5 × 103 to 5 × 104 wild-type cells were each mixed with 5 × 105 wild-type competitors and transplanted into recipients (6-7 recipients per each test cell type and amount, except only 3 recipients for 5 × 104 wild-type cells and 9 recipients for 2 × 105Cul4A+/− cells). The percentage of recipients not engrafted (overall percentage donor chimerism less than 5%) was plotted versus test cell dose. The 5% cutoff was chosen, because in control transplantations where only C57Bl/6J wild-type cells (CD45.2+) were transplanted into B6.BoyJ (CD45.1+) recipients, the background host percentage chimerism was approximately 5% 6 months after transplantation.
Cul4A+/− HSCs exhibit an engraftment defect. (A) Expression of Cul4A protein in Lin− LDMNCs. LDMNCs were isolated from Cul4A+/− and wild-type littermates, and Lin− cells were obtained by negative selection (Lineage Cell Depletion Kit; Miltenyi Biotec, Auburn, CA). Cell lysates were prepared and analyzed by immunoblot as described.12,13 Quantitation of scanned film was performed using ImageJ (http://rsb.info.nih.gov/ij/; National Institutes of Health, Bethesda, MD) and normalized for β-actin loading. (B) Competitive repopulation with a 1:1 ratio of test donor cells and competitors; overall percentage donor chimerism. For Cul4A+/− or wild-type donors (C57BL/6), 5 × 105 bone marrow LDMNCs (CD45.2+) were mixed with 5 × 105 wild-type competitor cells (B6.BoyJ, CD45.1+) and transplanted into 5 to 6 lethally irradiated wild-type recipients (CD45.1+) by tail vein injection. Overall engraftment (percentage CD45.2+) for Cul4A+/− (■) or wild-type (□) test cells was measured 2 to 6 months after transplantation by flow cytometric analysis of peripheral blood with anti-CD45.1 or anti-CD45.2 antibodies conjugated with fluorescein isothiocyanate (FITC; Pharmingen, San Diego, CA). (C) Engraftment into myeloid and lymphoid lineages. For the transplantation described in panel B, engraftment of Cul4A+/− or wild-type test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was also measured using biotin-conjugated anti-Gr-1, -Mac-1, -B220, or both -CD4 and -CD8 antibodies, respectively, and then streptavidin-APC secondary antibody (Pharmingen), each in combination with the anti-CD45.1 and -CD45.2 antibodies described for panel B. Percentage CD45.2+ for Cul4A+/− (■) or wild-type (□) test cells is graphed for each lineage 6 months after transplantation. (D) Competitive repopulation with a 1/3:1 ratio of test donor cells and competitors; overall percentage donor chimerism. For Cul4A+/− or wild-type donors, 1.7 × 105 bone marrow LDMNCs were mixed with 5 × 105 wild-type competitors in a competitive repopulation analogous to that described for panel B. Overall engraftment was determined in the same way, and graphed for Cul4A+/− (■) or wild-type (□) test cells 2 to 6 months after transplantation. (E) Engraftment into myeloid and lymphoid lineages for test cells mixed 1/3:1 with competitors. For the competitive repopulation described in panel D, percentage CD45.2+ for Cul4A+/− (filled bars) or wild-type (open bars) test cells was determined as described in panel C and graphed for each lineage 6 months after transplantation. For panels B-E, mean (± SEM) is graphed. (F) Limiting dilution. From 5 × 103 to 2 × 105Cul4A+/− bone marrow LDMNCs and 5 × 103 to 5 × 104 wild-type cells were each mixed with 5 × 105 wild-type competitors and transplanted into recipients (6-7 recipients per each test cell type and amount, except only 3 recipients for 5 × 104 wild-type cells and 9 recipients for 2 × 105Cul4A+/− cells). The percentage of recipients not engrafted (overall percentage donor chimerism less than 5%) was plotted versus test cell dose. The 5% cutoff was chosen, because in control transplantations where only C57Bl/6J wild-type cells (CD45.2+) were transplanted into B6.BoyJ (CD45.1+) recipients, the background host percentage chimerism was approximately 5% 6 months after transplantation.
The ability of Cul4A+/− and wild-type bone marrow LDMNCs to engraft lethally irradiated recipients was evaluated initially. For Cul4A+/− or wild-type donors, 5 × 105 or 1.7 × 105 “test cells” (CD45.2+) were mixed with 5 × 105 wild-type competitors (CD45.1+, a 1:1 or 1/3:1 ratio, respectively) and transplanted into wild-type recipients (CD45.1+). Engraftment into myeloid and lymphoid lineages 1 to 6 months after transplantation was measured. The percentage donor chimerism of Cul4A+/− test cells overall (Figure 1B) and for each lineage (Figure 1C) was not statistically different from the wild type. However, the average engraftment of the Cul4A+/− test cells overall and for each lineage was consistently lower, especially when one third as many test cells were transplanted (Figure 1D-E).
These small but consistent differences suggested Cul4A+/− stem cells might exhibit an engraftment defect under conditions of greater hematopoietic stress. To test this hypothesis, a limiting-dilution CRU assay was conducted. A range of test cell doses of either Cul4A+/− or wild-type donor cells was transplanted with competitors to calculate a CRU frequency 6 months after transplantation. Frequencies of 1 in 15 000 cells for wild type (consistent with published findings15 ) and 1 in 131 000 cells for Cul4A+/− were determined (Figure 1F). Therefore, the ability of Cul4A+/− HSCs to engraft under conditions of hematopoietic stress is 9-fold lower than that of wild-type cells. These studies illustrate the power of the CRU assay: (1) a limiting dilution enables quantification, (2) long-term repopulation in vivo provides the only universally accepted assay for HSCs, and (3) repopulation with competitors creates hematopoietic stress, making this assay particularly sensitive.
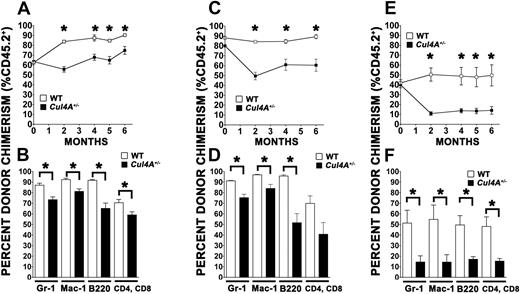
To determine the effect of Cul4A haploinsufficiency on HSC self-renewal, secondary transplantations were conducted. Primary transplant recipients of Cul4A+/− test cells and wild-type controls with similar percentage donor chimerism 6 months after transplantation (Figure 1B) were selected as donors. At 2 to 6 months after transplantation, the overall percentage donor chimerism of Cul4A+/− cells derived from the 1:1 test cell group was significantly lower than that for wild-type cells (Figure 2 A, P ≤ .02). Also, the percentage donor chimerism of Cul4A+/− myeloid and lymphoid cells was significantly lower 5 months after transplantation, consistent with an HSC self-renewal defect (Figure 2B, 0.002 ≤ P < .05).
Serial transplantation assays show that Cul4A+/− HSCs have a self-renewal defect. (A) Secondary transplantation with donors from the 1:1 primary transplantation. For the primary transplantation with a 1:1 ratio of test to competitor cells, one recipient of Cul4A+/− test cells and a wild-type control with similar percentage donor chimerism 6 months after transplantation were used as donors in secondary transplantations. For each donor, 106 bone marrow LDMNCs were transplanted into 3 to 4 lethally irradiated wild-type recipients, and overall percentage donor chimerism was measured 1 to 6 months after transplantation for Cul4A+/− (■) and wild-type (□) test cells, similar to that described in Figure 1B. *P ≤ .02. (B) Engraftment into myeloid and lymphoid lineages. For the secondary transplantation described in panel A, engraftment of Cul4A+/− (filled bars) or wild-type (open bars) test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was determined 5 months after transplantation as described in Figure 1C. *0.002 ≤ P < .05. (C) Tertiary transplantations. Tertiary transplantations were performed with donors from the secondary transplantation described in panels A and B: a recipient of Cul4A+/− test cells and a corresponding wild-type test cell recipient with closely matched percentage donor chimerism 6 months after transplantation were donors. For each donor, 106 bone marrow LDMNCs were transplanted into each of 5 to 6 wild-type recipients. Overall percentage donor chimerism was determined (as described in Figure 1B) 1 to 6 months after transplantation for Cul4A+/− (■) and wild-type (□) test cells. *P < .006. (D) Tertiary transplantation; engraftment into myeloid and lymphoid lineages. For the tertiary transplantation described in panel C, engraftment of Cul4A+/− (filled bars) or wild-type (open bars) test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was determined 6 months after transplantation as described in Figure 1C. *P < .007. The difference between Cul4A+/− and control engraftment into the T-cell lineage was not quite significant (P = .054). However, the difference in engraftment into this lineage is clearly statistically significant when fewer cells were transplanted (F). (E) Secondary transplantation with donors from the 1/3:1 primary transplantation. For the primary transplantation with a 1/3:1 ratio of test to competitor cells, 2 recipients of Cul4A+/− test cells and, for each, a wild-type control with similar percentage donor chimerism were used as donors in secondary transplantations. For each donor, 106 bone marrow LDMNCs were transplanted into 3 to 4 recipients, and overall percentage donor chimerism was measured 1 to 6 months after transplantation for Cul4A+/− (■) and wild-type (□) test cells as described in Figure 1B. *P ≤ .007. (F) Secondary transplantation with 1/3:1 donors; engraftment into myeloid and lymphoid lineages. For the secondary transplantation described in panel E, engraftment of Cul4A+/− (filled bars) or wild-type (open bars) test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was determined 6 months after transplantation as described in Figure 1C. *.001 ≤ P ≤ .02. For all graphs, mean (± SEM) is graphed.
Serial transplantation assays show that Cul4A+/− HSCs have a self-renewal defect. (A) Secondary transplantation with donors from the 1:1 primary transplantation. For the primary transplantation with a 1:1 ratio of test to competitor cells, one recipient of Cul4A+/− test cells and a wild-type control with similar percentage donor chimerism 6 months after transplantation were used as donors in secondary transplantations. For each donor, 106 bone marrow LDMNCs were transplanted into 3 to 4 lethally irradiated wild-type recipients, and overall percentage donor chimerism was measured 1 to 6 months after transplantation for Cul4A+/− (■) and wild-type (□) test cells, similar to that described in Figure 1B. *P ≤ .02. (B) Engraftment into myeloid and lymphoid lineages. For the secondary transplantation described in panel A, engraftment of Cul4A+/− (filled bars) or wild-type (open bars) test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was determined 5 months after transplantation as described in Figure 1C. *0.002 ≤ P < .05. (C) Tertiary transplantations. Tertiary transplantations were performed with donors from the secondary transplantation described in panels A and B: a recipient of Cul4A+/− test cells and a corresponding wild-type test cell recipient with closely matched percentage donor chimerism 6 months after transplantation were donors. For each donor, 106 bone marrow LDMNCs were transplanted into each of 5 to 6 wild-type recipients. Overall percentage donor chimerism was determined (as described in Figure 1B) 1 to 6 months after transplantation for Cul4A+/− (■) and wild-type (□) test cells. *P < .006. (D) Tertiary transplantation; engraftment into myeloid and lymphoid lineages. For the tertiary transplantation described in panel C, engraftment of Cul4A+/− (filled bars) or wild-type (open bars) test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was determined 6 months after transplantation as described in Figure 1C. *P < .007. The difference between Cul4A+/− and control engraftment into the T-cell lineage was not quite significant (P = .054). However, the difference in engraftment into this lineage is clearly statistically significant when fewer cells were transplanted (F). (E) Secondary transplantation with donors from the 1/3:1 primary transplantation. For the primary transplantation with a 1/3:1 ratio of test to competitor cells, 2 recipients of Cul4A+/− test cells and, for each, a wild-type control with similar percentage donor chimerism were used as donors in secondary transplantations. For each donor, 106 bone marrow LDMNCs were transplanted into 3 to 4 recipients, and overall percentage donor chimerism was measured 1 to 6 months after transplantation for Cul4A+/− (■) and wild-type (□) test cells as described in Figure 1B. *P ≤ .007. (F) Secondary transplantation with 1/3:1 donors; engraftment into myeloid and lymphoid lineages. For the secondary transplantation described in panel E, engraftment of Cul4A+/− (filled bars) or wild-type (open bars) test cells into the granulocyte, macrophage, B-cell, and T-cell lineages was determined 6 months after transplantation as described in Figure 1C. *.001 ≤ P ≤ .02. For all graphs, mean (± SEM) is graphed.
Furthermore, in tertiary transplantations the overall percentage donor chimerism of wild-type test cells was 84% to 89% 2 to 6 months after transplantation, but engraftment for Cul4A+/− cells was only 50% to 61% (Figure 2C, P < .006). Similar differences were observed for myeloid and lymphoid lineages (Figure 2D), further demonstrating that Cul4A+/− HSCs exhibit a self-renewal defect.
In addition, when primary recipients that received fewer test cells were donors for secondary transplantations, the overall percentage donor chimerism for the secondary recipients of Cul4A+/− test cells was 4- to 5-fold lower than that for wild-type cells (Figure 2E, P ≤ .007). Further, the percentage donor-derived lineage-positive cells was 3- to 4-fold lower in recipients of transplanted Cul4A+/− test cells (Figure 2F, 0.0005 ≤ P ≤ .02). Therefore, Cul4A+/− HSCs in secondary transplant recipients exhibited an even greater reduction of percentage donor chimerism when primary transplant recipients received fewer test cells.
Overall, CRU and serial transplantation assays demonstrate that Cul4A+/− HSCs have defects in both engraftment and self-renewal and indicate that Cul4A is required for normal HSC function. Also, because test donor cells were transplanted into wild-type recipients, these findings support a Cul4A+/− hematopoietic cell-autonomous, microenvironment-independent mechanism. Combined with earlier findings, these results indicate that Cul4A is required for the normal function of HSCs, progenitors, and precursors, and for terminal differentiation.10,–12
These findings suggest a Cul4A ubiquitin ligase targets a regulator of HSC function for degradation. Cul4A haploinsufficiency would cause overexpression of this protein, which apparently negatively modulates HSC function. Of the known HSC regulators targeted by ubiquitination, most appear to promote HSC function.1,,,,,–7 However, some reports suggest p21Cip1 and p27Kip1 can inhibit function. Although p21Cip1-deficient mice exhibited a self-renewal defect, down-regulating p21Cip1 in human HSCs enhanced engraftment.2,16 Whereas analyses of p27Kip1-deficient mice indicate this gene regulates progenitors, mice deficient in both p27Kip1 and MAD1 exhibited enhanced stem-cell function,2,17 suggesting that under some conditions p27Kip negatively regulates HSC function. Of these 2, p27Kip1 is known to be targeted for degradation by a Cul4A-ubiquitin ligase in erythroblasts12 and in nonhematopoietic cells,18 so p27Kip1 overexpression in Cul4A-haploinsufficient stem cells might impair engraftment and self-renewal. A Cul4A-ubiquitin ligase targets HoxA9 for degradation in myeloid cells, but in HSCs HoxA9 promotes function.11,19 None of the other Cul4A targets identified so far has known HSC regulatory functions. Nevertheless, since Cul4A-mediated regulation occurs at the protein level, direct identification of the Cul4A-ubiquitin ligase target(s) important for HSC function requires measuring protein expression levels in HSCs—technically challenging but important to understand how ubiquitin-mediated proteolysis regulates HSC function.
Bortezomib (PS-341) is the first proteasome inhibitor to enter clinical trials with cancer patients, initially those with advanced relapsed and/or refractory multiple myeloma (MM).20,21 Although bortezomib offers great promise as a treatment for MM, side effects include thrombocytopenia (40%), anemia (21%), and neutropenia (19%), suggesting adverse effects on normal hematopoiesis and possibly HSCs. Since bortezomib alters the expression of many proteins degraded by the proteasome, a greater understanding of ubiquitin ligases and their substrates could aid the refinement of therapies to target specific subsets of proteins, thereby reducing toxicity, improving efficacy, and ultimately improving therapies against MM and other cancers.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by R01 DK066603 from the National Institutes of Health, an Indiana University School of Medicine Biomedical Research Grant, the Lilly Endowment, and the Riley Children's Fund (K.T.C.). A grant from the National Institutes of Health (R01 HL077175) also provided support (L.S.H.). D.L.W. was supported, in part, by the National Institutes of Health, National Research Service Award Number T32 DK07519-Regulation of Hematopoietic Cell Production.
We thank Merv Yoder and Dave Skalnik for many insightful suggestions and stimulating discussions and Scott Johnson and Chris Shelley for important technical expertise.
National Institutes of Health
Authorship
Contribution: B.L., N.J., D.L.W., and F.-C.Y. performed research; L.S.H. designed research and critically reviewed the paper; K.T.C. designed research, performed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kristin T. Chun, Herman B Wells Center for Pediatric Research, Cancer Research Building, Rm 474, Indianapolis, IN 46202; e-mail:kchun@iupui.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal