Abstract
α-emitting radionuclides are highly cytotoxic and are of considerable interest in the treatment of cancer. A particularly interesting approach is in radioimmunotherapy. However, α-emitting antibody conjugates have been difficult to exploit clinically due to the short half-life of the radionuclides, low production capability, or limited source materials. We have developed a novel technology based on the low-dose rate α-particle–emitting nuclide 227Th, exemplified here using the monoclonal antibody rituximab. In vitro, this radioimmunoconjugate killed lymphoma cells at Becquerel per milliliter (Bq/mL) levels. A single injection of 227Th-rituximab induced complete tumor regression in up to 60% of nude mice bearing macroscopic (32-256 mm3) human B-lymphoma xenografts at Becquerel per gram (Bq/g) levels without apparent toxicity. Therapy with 227Th-rituximab was significantly more effective than the control radioimmunoconjugate 227Th-trastuzumab and the standard β-emitting radioimmunoconjugate for CD20+ lymphoma90Y-tiuxetan-ibritumomab. Thorium-227 based constructs may provide a novel approach for targeted therapy against a wide variety of cancers.
Introduction
Monoclonal antibodies conjugated to the β-emitting isotopes, 131I and 90Y, are currently standard treatment options for patients with CD20-expressing B-cell non-Hodgkin lymphoma, and have produced long-term responses in up to 86% of patients.1–5 However, the long path lengths of the β and γ emissions from these radionuclides generate dose-limiting myelosuppression at conventional doses, and cardiopulmonary toxicities at higher doses when used with stem cell transplantation.2 Furthermore, the low energy transfer characteristics of the β-particles result in suboptimal killing of tumor cells, ultimately leading to relapse in most treated patients
α-particle radiation, on the other hand, yields high linear energy transfer and confers potent cytotoxicity within a radius of less than 100 μm of the decaying radionuclide. Monoclonal antibodies labeled with α-emitting radionuclides 213Bi, 211At, and 225Ac show promise for radioimmunotherapy.6–8 However, 213Bi and 211At are challenging to apply in clinical settings because of their short half-lives (46 minutes and 7.2 hours, respectively) and their limited production capability with currently available technology. 225Ac (t1/2=10.0 days) has been effective when conjugated to monoclonal antibodies, but the supply of source material for the preparation of this nuclide is very limited.8,9 Cationic 223Ra (t1/2=11.4 days) has recently shown considerable promise in clinical trials in patients with skeletal metastases,10 and may also be used with liposomes,11 but cannot be stably conjugated to monoclonal antibodies.12
Here, we suggest that 227Th, the precursor of 223Ra, may be an attractive radionuclide to explore for radioimmunotherapy based on its physical and chemical properties and its availability.13,14 227Th has a half-life of 18.7 days and can be produced in practically unlimited amounts from 227Ac, which is generated by thermal neutron irradiation of 226Ra.15 Consequently, long-term operating generators for 227Th can be prepared relatively easily and affordably. The long half-life of 227Th should permit conjugation, administration and targeting of a 227Th-labeled radioimmunoconjugate (RIC) before a significant amount of 223Ra is generated. The relatively long half-life of 223Ra, in turn, assures that this nuclide would be largely excreted or trapped in skeletal hydroxyapatite before decay occurs.10 Although a considerable amount of 223Ra is taken up in bone,16 this probably will not cause bone marrow toxicity at relevant levels because of the short range of the α-particles as indicated by recent evaluation of this radionuclide in animals and humans.17,18 Thus, a therapeutic window permitting treatment with 227Th with acceptable toxicity may exist. Furthermore, the relatively modest γ components of 227Th and the 223Ra series reduce the necessity for patient shielding, allowing α-radioimmunotherapy to be given on an outpatient basis. The γ-photons emitted by 227Th are suitable for imaging and may facilitate dosimetry evaluation in patients.
Since antibody that binds to the tumor target will remain in the body for a longer time than antibody that is not bound, the longer half-life of 227Th also leads to a higher tumor-to–normal organ ratio of absorbed radiation than would be delivered by a nuclide with a shorter half-life. Micrometastases and disseminated malignancies have been proposed as the most suitable indications for radioimmunotherapy with α-emitters because of the short effective ranges of α particles, since minimal disease permits more rapid targeting and has limited penetration barriers. However, the considerations above suggest that 227Th-labeled antibodies might also be effective for treatment of macroscopic tumors. These considerations motivated us to compare a standard β-emitting anti-CD20 RIC, 90Y-tiuxetan-ibritumomab, with our α-emitting counterpart, 227Th-DOTA-p-benzyl-rituximab, in a lymphoma xenograft model.
Materials and methods
Preparation of 227Th-DOTA-p-benzyl-rituximab
227Th, 227Th-p-isothiocyanato-benzyl-DOTA complexes, and 227Th-DOTA-p-benzyl-rituximab (F. Hoffman-LaRoche AG, Basel, Switzerland) were prepared as previously described.13,16,19 The specific activity of the RIC was in the range of 650 to 5300 Bq/μg. The quality of the RIC was assessed using lymphoma cells and a modified Lindmo and Bunn method.20 Cell concentrations of up to 108 Raji cells/mL were used to compensate for the modest specific activity of the RIC.13,16 The immunoreactive fractions of conjugates used in the current study were between 56% and 65%.
Measurement of cell growth
Cells of the CD20-expressing B-cell lymphoma line Raji were used. Single-cell suspensions were grown in a humidified atmosphere with 95% air/5% CO2 in RPMI 1640 (PAA, Linz, Austria) supplemented with 13% heat-inactivated FCS (PAA), 1% l-glutamine (PAA), and 1% penicillin-streptomycin (PAA). A total of 106 cells were seeded in 10 mL medium in 25-cm2 bottles at day 0. In half of the bottles, the cells were blocked by 10 μg/mL unlabeled rituximab. The 227Th-DOTA-p-benzyl-rituximab was added in amounts equivalent to 0, 100, 200, or 400 Bq/mL. At days 1, 4, 6, and 9, a 2.5-mL sample was taken for cell counting by a Coulter counter.21 Subsequently, the cells were centrifuged, medium was removed so that 5 mL was left, and 5 mL fresh medium was added. The cells were resuspended and seeded out in the same bottles. In the bottles with blocked cells, 10 μg/mL unlabeled rituximab was added.
Animals
Institutionally bred female Balb/C nu/nu (NCR) mice that were 4 to 8 weeks old and had body weights in the range of 18 to 22 g at the start of the experiment were used. The animals were maintained under pathogen-free conditions, and food and water were supplied ad libitum. All procedures and experiments involving animals in this study were approved by the National Animal Research Authority and carried out according to the European Convention for the Protection of Vertebrates Used for Scientific Purposes. Mice were anesthetized with 200 μL Tiletamin-Zolazepam mix (Virbac, Carros Cedex, France) diluted 1:5 with saline and given intraperitoneally before implantation with about 2 × 2 × 2-mm pieces of Raji B-lymphoma tumor tissue.
Biodistribution experiments
The biodistributions of 227Th-DOTA-p-benzyl-rituximab, 227Th-DOTA-p-benzyl-trastuzumab (F. Hoffman-LaRoche AG) and 125I-ibritumomab-tiuexetan (Schering AG, Berlin, Germany) were studied in mice with tumor sizes of 32 to 256 mm3 at the start of the study. Ibritumomab-tiuexetan was labeled with 125I in an IODOGEN Pre-Coated Iodination Tube (Pierce, Rockford, IL) according to the manufacturer's description. The preparations were administered by tail vein injection of 100 μL solution to each animal. A mean activity of 1100 kBq/kg, 620 kBq/kg, or 1250 kBq/kg was injected for 227Th-DOTA-p-benzyl-rituximab, 227Th-DOTA-p-benzyl-trastuzumab, and 125I-ibritumomab-tiuexetan, respectively. For 125I-ibritumomab-tiuexetan, the measured values were adjusted for the decay of 125I and 90Y. A total of 6 to 8 animals were used per time point. Autopsies were performed after cervical dislocation at various time points after injection. The weight of each tissue sample was determined, and 227Th and 223Ra were measured by their most characteristic γ rays using the solid-state photon detector GEM-50 (Ortec, Oak Ridge, TN) coupled to a digital γ-ray spectrometer (Dispec Jr; Ortec) and analyzed using the computer software Gammavision-32 Version 6.01 (Ortec). For 227Th, the 235.97 keV γ ray (11.6% probability) was chosen, and for 223Ra, the 154.21 keV γ ray (5.62% probability) was chosen. The count rates in the samples were also routinely measured using a γ counter (Crystal II Multidetector RIA System; Packard Instrument Co, Downers Grove, IL). The 125I-ibritumomab-tiuexetan samples were measured with a γ counter (Cobra-gamma; Packard Instrument Co). Samples of the injectates were used as references in the measurement procedures.
Calculation of absorbed radiation dose
The absorbed radiation doses were calculated assuming dose contributions coming only from α-particle emissions for the 227Th conjugates. Mean α-energies of 5.9 MeV for 227Th and 26.4 MeV for 223Ra with α-emitting daughters in equilibrium were used (Nuclide Explorer 2000 (1.00), Institute for Transuranium Elements, Karlsruhe, Germany). It was assumed that there was 100% absorption of the α particles in the tissues measured. The biodistribution data were normalized to an injection of 200 kBq/kg body weight for the 227Th conjugates. It was assumed that the radionuclides were uniformly distributed in the various tissues. For blood, 100% absorption of the α-particles was assumed. This is a simplification, since there will be some escape of α-particles beyond the blood in the capillaries.
To determine the dose after 90Y-ibritumomab-tiuexetan treatment, the activities of 125I-ibritumomab-tiuexetan measured at different time points, t, were divided by e−ln2/T1/2(125I)·t, where T1/2(125I)is the half-life of 125I and then multiplied by e−ln2/T1/2(90Y)·t, where T1/2(90Y)is the half-life of 90Y. It was assumed that only the β particle emissions contributed to the dose, and that the radionuclides were distributed uniformly in the tissue. A mean β- energy of 0.9336 MeV was used.22 The biodistribution data were normalized to an injection of 7.5 MBq/kg. It was assumed that there was 100% absorption of the β particles in the tissues measured.
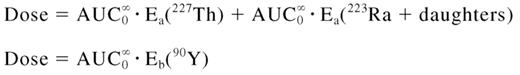
The total number of disintegrations from the time of the injection of the preparation until no activity was left in the body was calculated by area under curve (AUC) estimate of the activity concentrations in various tissues versus time.23 Thus, the total dose to each organ could be calculated by Equation 1:
Experimental therapy studies
Treatment started when macroscopically growing tumors (32-256 mm3) had formed. Control mice were injected with 100 μL NaCl or with 100 μL PBS containing 20, 100, or 250 μg cold rituximab. For radioimmunotherapy, mice were injected with 50, 200, 400, or 1000 kBq/kg 227Th-DOTA-p-benzyl-rituximab; 200 or 400 kBq/kg 227Th-DOTA-p-benzyl-trastuzumab; or 7.5, 15, or 30 MBq/kg of 90Y-tiuxetan-ibritumomab, which correspond to 50%, 100%, or 200% of the recommended clinical human dosage of 90Y-tiuxetan-ibritumomab (Schering AG). Clinical grade 90Y-tiuxetan-ibritumomab was obtained from the Department of Nuclear Medicine at the Norwegian Radium Hospital. Tumor growth and mouse survival were assessed 3 times a week in the first week before injection and throughout the first month after injection; thereafter, growth and survival were assessed 2 times a week. Mice with tumor diameters larger than 20 mm were killed. The different treatment groups were compared by the Mantley-Cox log-rank test. Treatment-induced growth delays, the differences in time to reach a size of 1000 mm3, were calculated after nonlinear regression of mean growth versus time and compared using the Student t test.
Hematologic evaluation
Balb/C nu/nu mice without tumors, weighing 25 to 30 g, were used for blood sampling at the 1- to 8-week time points. Animals used in therapy experiments and which had complete tumor regression to the treatment were compared with similar aged untreated animals at 14, 19, 30, and 36 weeks. The mice were divided into 5 groups, each containing 12 to 15 mice receiving either saline or 200, 400, or 1000 kBq/kg 227Th-DOTA-p-benzyl-rituximab. At 1, 2, 3, 4, 5, 14, and 30 weeks after injection, approximately 200 μL blood was collected from the vena saphena lateralis in 0.5-mL EDTA-coated tubes (Microtainer; Becton Dickinson, Franklin Lakes, NJ). At least 3 weeks separated each blood sampling of an individual mouse. In addition, at 6, 7, 8, 19, and 36 weeks after injection, the mice were anesthetized using sevoflurane (Abbott, Abbott Park, IL), blood was collected by heart puncture, and the mice were killed by cervical dislocation. In weeks 1 and 5 the samples were counted by a hemolysis method24 : 100 mL blood were mixed with 1 mL lysing solution (VersaLyse; Beckman Coulter, Fullerton, CA) for at least 15 minutes to remove red blood cells. Subsequently, the white blood cells were counted in an automatic viability analyzer (Vi-Cell-XR; Beckman Coulter). At all other time points, the blood samples were evaluated for complete blood counts (CBCs) according to standard procedures by the Central Laboratory, Norwegian School of Veterinary Science.
Results
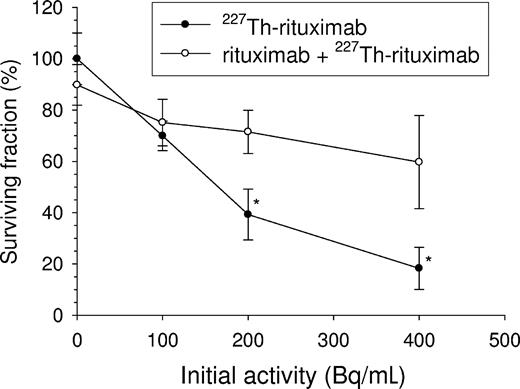
Single-cell cancer model in vitro
Incubation with 227Th-DOTA-p-benzyl-rituximab for 8 days significantly inhibited growth of CD20+ human Raji B-lymphoma cells (Figure 1). On days 1, 4, and 6 of the experiment, half of the medium was changed to simulate the elimination of RIC that occurs in the body and to supply the cells with nutrients. Cold rituximab alone had no significant effect. Cultures containing cells that were blocked with cold rituximab prior to the addition of 227Th-DOTA-p-benzyl-rituximab demonstrated some growth inhibition due to nonspecific radiation from the medium. The doubling time increased from 43 hours for untreated cells to 93 hours for cells treated with 400 Bq/mL 227Th-DOTA-p-benzyl-rituximab. It should be noted that the RIC-specific activity was low in these experiments, typically between 0.5 and 1.0 MBq/mg.
In vitro cytotoxicity. Relative number of surviving Raji cells treated with increasing activities of 227Th-p-benzyl-DOTA-rituximab. The relative cell number was calculated by dividing the number of treated cells by the number of control cells at day 8 after start of incubation. On days 1, 4, and 6, half of the medium was changed to simulate the elimination of RIC that occurs in the body and to supply the cells with nutrients. ○ shows that binding of 227Th-p-benzyl-DOTA-rituximab to the cells was blocked by incubation with cold rituximab (10 μg/mL). ● indicats without cold rituximab. *Significantly different from corresponding blocked cells (t test, P < .05). Error bars represent SE from 3 to 5 experiments.
In vitro cytotoxicity. Relative number of surviving Raji cells treated with increasing activities of 227Th-p-benzyl-DOTA-rituximab. The relative cell number was calculated by dividing the number of treated cells by the number of control cells at day 8 after start of incubation. On days 1, 4, and 6, half of the medium was changed to simulate the elimination of RIC that occurs in the body and to supply the cells with nutrients. ○ shows that binding of 227Th-p-benzyl-DOTA-rituximab to the cells was blocked by incubation with cold rituximab (10 μg/mL). ● indicats without cold rituximab. *Significantly different from corresponding blocked cells (t test, P < .05). Error bars represent SE from 3 to 5 experiments.
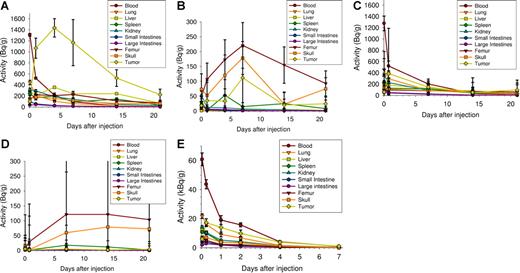
Biodistribution of RICs
To assess binding of 227Th-rituximab and retention of the daughter 223Ra in vivo, the radioactivity per gram of tissue was measured in various normal organs and in tumors at various time points after injection of 227Th-DOTA-p-benzyl-rituximab in nude mice with CD20-expressing Raji xenografts (Figure 2A,B). There was a large difference between the amount of activity of 227Th-DOTA-p-benzyl-rituximab in tumor and in normal organs. The uptake of 227Th-DOTA-p-benzyl-rituximab in Raji xenografts reached a maximum 4 days after injection (Figure 2A). Previously, we measured the biodistribution of 227Th-DOTA-p-benzyl-rituximab in Balb/C mice without tumors,16 and similar normal tissue dose-distribution profiles were observed. The control antibody trastuzumab, which does not bind to Raji cells, was also conjugated to 227Th and injected into nude mice with Raji xenografts to assess nonspecific tumor uptake (Figure 2C-D). The uptake of 227Th-DOTA-p-benzyl-trastuzumab in tumor was significantly less than with 227Th-DOTA-p-benzyl-rituximab (t test, P < .05). The daughter nuclide, 223Ra, mainly localized to bone (eg, femur and skull) for both RICs (Figure 2B,D), although some tumor retention was seen of 223Ra produced from 227Th-DOTA-p-benzyl-rituximab decaying in the tumors (Figure 2B). The activity of 125I-tiuxetan-ibritumomab in tumor was lower than the activity in blood for all time points, and after the initial uptake it decreased with similar rate as the activity in blood (Figure 2E). Thus, the tumor specificity was higher and the retention time in tumor was longer for 227Th-DOTA-p-benzyl-rituximab.
Biodistribution of RICs in mice with CD20+ Raji xenografts. Uptake and retention of 227Th-p-benzyl-DOTA-rituximab (A-B), 227Th-p-benzyl-DOTA-trastuzumab (C-D) and 125I-ibritumomab-tiuexetan (E) in tumor xenografts and normal tissues were measured at various time points after injection into athymic mice bearing Raji xenografts. The activity per gram was measured using the 236-keV line of 227Th (A,C) and a germanium detector. (B,D) Activity per gram of 223Ra measured using the 154-keV line of 223Ra. The measured 227Th activities were normalized to an injection of 200 kBq/kg body weight. The activity of 125I was measured using a γ counter and normalized to an injection of 7.5 MBq 90Y/kg body weight. Error bars represent SE. A total of 6 to 8 mice were used.
Biodistribution of RICs in mice with CD20+ Raji xenografts. Uptake and retention of 227Th-p-benzyl-DOTA-rituximab (A-B), 227Th-p-benzyl-DOTA-trastuzumab (C-D) and 125I-ibritumomab-tiuexetan (E) in tumor xenografts and normal tissues were measured at various time points after injection into athymic mice bearing Raji xenografts. The activity per gram was measured using the 236-keV line of 227Th (A,C) and a germanium detector. (B,D) Activity per gram of 223Ra measured using the 154-keV line of 223Ra. The measured 227Th activities were normalized to an injection of 200 kBq/kg body weight. The activity of 125I was measured using a γ counter and normalized to an injection of 7.5 MBq 90Y/kg body weight. Error bars represent SE. A total of 6 to 8 mice were used.
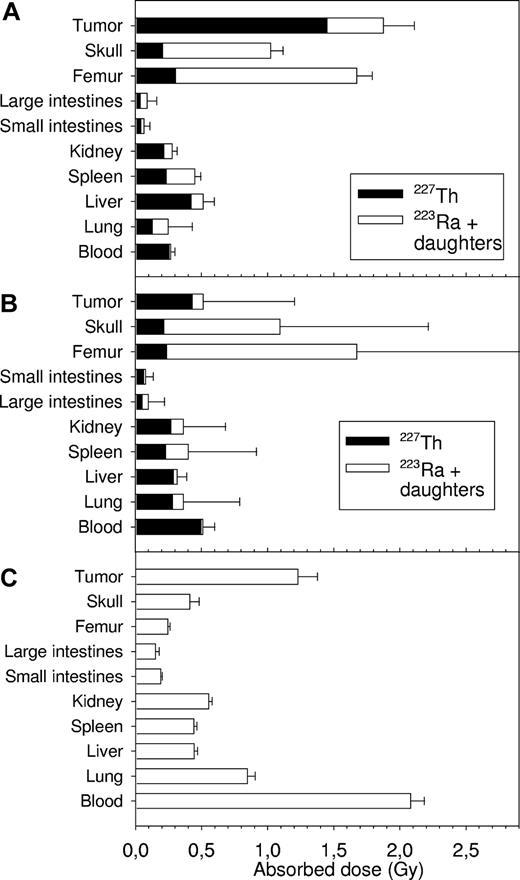
The radiation doses to normal tissues and to tumor for 227Th-DOTA-p-benzyl-rituximab (Figure 3A) and 227Th-DOTA-p-benzyl-trastuzumab (Figure 3B) were determined by calculating the area under the biodistribution curves and multiplying the resulting cumulated activity with the mean α-particle energy from 227Th or 223Ra and daughters. It was assumed that only α particles contributed to dose and that the radium daughters decayed in the same tissue as radium. When normalized to 200 kBq injected dose per kilogram of body weight, the doses to tumor were approximately 0.5, 2, and 4 Gy for injected dosages of 50, 200, and 400 kBq/kg 227Th-DOTA-p-benzyl-rituximab, respectively. Injection of 227Th-DOTA-p-benzyl-trastuzumab resulted in a significantly lower radiation dose to tumor than injection of 227Th-DOTA-p-benzyl-rituximab. The radiation doses to other tissues were similar to the doses obtained with 227Th-DOTA-p-benzyl-rituximab.
Absorbed doses to tumor xenografts and normal tissues. Cumulated activities were calculated from biodistribution curves and multiplied with the mean energy of the α particles from 227Th or from 223Ra and daughters in order to estimate the absorbed dose after injection of 227Th-p-benzyl-DOTA-rituximab (A) or 227Th-p-benzyl-DOTA-trastuzumab (B). For 90Y-ibritumomab-tiuexetan (C), cumulated activities were calculated from the biodistribution curves of 125I-ibritumomab-tiuexetan adjusted for decay of 125I. The activities of 227Th-p-benzyl-DOTA-rituximab and 227Th-p-benzyl-DOTA-trastuzumab were normalized to an injection of 200 kBq/kg and the activities of 90Y-ibritumomab-tiuexetan were normalized to an injection of 15 MBq/kg. Data are mean (± SE).
Absorbed doses to tumor xenografts and normal tissues. Cumulated activities were calculated from biodistribution curves and multiplied with the mean energy of the α particles from 227Th or from 223Ra and daughters in order to estimate the absorbed dose after injection of 227Th-p-benzyl-DOTA-rituximab (A) or 227Th-p-benzyl-DOTA-trastuzumab (B). For 90Y-ibritumomab-tiuexetan (C), cumulated activities were calculated from the biodistribution curves of 125I-ibritumomab-tiuexetan adjusted for decay of 125I. The activities of 227Th-p-benzyl-DOTA-rituximab and 227Th-p-benzyl-DOTA-trastuzumab were normalized to an injection of 200 kBq/kg and the activities of 90Y-ibritumomab-tiuexetan were normalized to an injection of 15 MBq/kg. Data are mean (± SE).
For 90Y-tiuxetan-ibritumomab (Figure 3C), the doses to normal tissues and to tumor were calculated using the biodistribution curves of 125I-tiuxetan-ibritumomab. It was assumed that all the β-particles were absorbed by the tumor and that the mean β-energy was 933.6 keV.23 The radiation doses to tumor were 0.6, 1.2, and 2.5 Gy for injected dosages of 7.5, 15, and 30 MBq/kg 90Y-tiuxetan-ibritumomab. For a given tumor radiation dose, the doses to normal tissues were compared: the radiation doses to the liver and the spleen were similar, while the radiation doses to the blood, lung, kidney, and intestines were more than 100% higher for 90Y-tiuxetan-ibritumomab than for 227Th-DOTA-p-benzyl-rituximab. For the skull and the femur, the radiation doses were more than 80% lower for 90Y-tiuxetan-ibritumomab than for 227Th-DOTA-p-benzyl-rituximab.
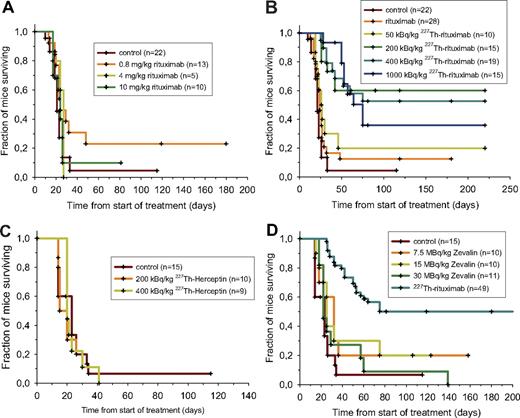
Therapy of mice with Raji lymphoma xenografts
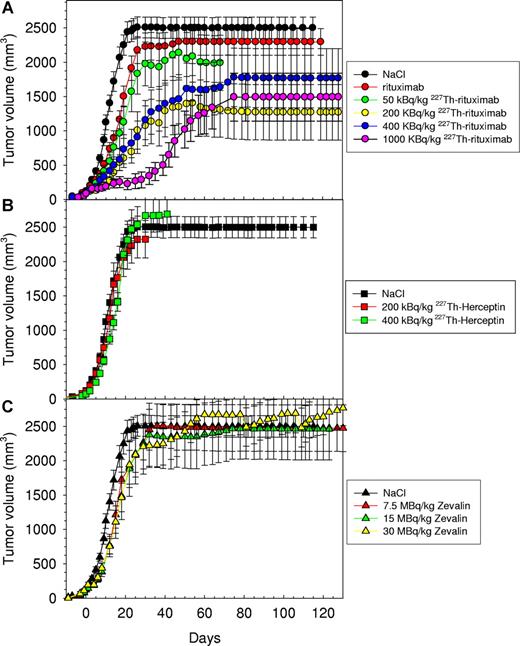
The efficacy of 227Th-DOTA-p-benzyl-rituximab for treating macroscopic tumors was assessed by measuring the growth of Raji lymphoma xenografts after radioimmunotherapy and comparing the results with control groups treated with saline, cold rituximab, 227Th-DOTA-p-benzyl-trastuzumab, and the β-emitting RIC 90Y-tiuxetan-ibritumomab (Figures 4–5). Treatment with 200 to 1000 kBq/kg 227Th-DOTA-p-benzyl-rituximab resulted in a pronounced delay in tumor growth and in a significant increase in survival compared with all other treatments (Table 1; Figures 4,Figure 5–6). Treatment with 50 kBq/kg 227Th-DOTA-p-benzyl-rituximab and cold rituximab had no significant effect on tumor growth or mean survival. The efficacy of the 227Th-DOTA-p-benzyl-rituximab treatment improved in a significant and dosage-dependent fashion in the range from 50 to 200 kBq/kg, but there was no further increase in therapeutic effect from 200 to 400 kBq/kg. By using 1000 kBq/kg 227Th-DOTA-p-benzyl-rituximab, a significant increase in growth delay as compared with 200 kBq/kg (t test, P=.003) was obtained, although the long-term survival tended to be lower for 1000 kBq/kg than for 200 kBq/kg (Table 1).
Effect of α-based radioimmunotherapy on growth of Raji xenografts. Mean tumor size versus time after intravenous injection of cold rituximab, 50, 200, and 400 kBq/mL 227Th-p-benzyl-DOTA-rituximab (A); intravenous injection of 200 and 400 kBq/mL 227Th-p-benzyl-DOTA-trastuzumab (B); or intravenous injection of 7.5, 15, and 30 MBq/kg 90Y-ibritumomab-tiuexetan (C). The data for cold rituximab were pooled from groups of mice injected with 20, 100, and 250 μg rituximab. Error bars represent SE. The tumors were not removed from the calculation of mean tumor size when the mice were censored.
Effect of α-based radioimmunotherapy on growth of Raji xenografts. Mean tumor size versus time after intravenous injection of cold rituximab, 50, 200, and 400 kBq/mL 227Th-p-benzyl-DOTA-rituximab (A); intravenous injection of 200 and 400 kBq/mL 227Th-p-benzyl-DOTA-trastuzumab (B); or intravenous injection of 7.5, 15, and 30 MBq/kg 90Y-ibritumomab-tiuexetan (C). The data for cold rituximab were pooled from groups of mice injected with 20, 100, and 250 μg rituximab. Error bars represent SE. The tumors were not removed from the calculation of mean tumor size when the mice were censored.
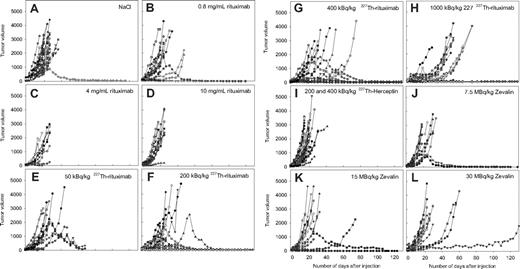
Effect of α-based radioimmunotherapy on growth of individual Raji xenografts. Individual tumor sizes versus time after intravenous injection of NaCl (A); 20, 100, and 250 μg cold rituximab (B-D); 50, 200, 400, and 1000 kBq/mL 227Th-p-benzyl-DOTA-rituximab (E-H); intravenous injection of 200 and 400 kBq/mL 227Th-p-benzyl-DOTA-trastuzumab (I); or intravenous injection of 7.5, 15, and 30 MBq/kg 90Y-ibritumomab-tiuexetan (J-L).
Effect of α-based radioimmunotherapy on growth of individual Raji xenografts. Individual tumor sizes versus time after intravenous injection of NaCl (A); 20, 100, and 250 μg cold rituximab (B-D); 50, 200, 400, and 1000 kBq/mL 227Th-p-benzyl-DOTA-rituximab (E-H); intravenous injection of 200 and 400 kBq/mL 227Th-p-benzyl-DOTA-trastuzumab (I); or intravenous injection of 7.5, 15, and 30 MBq/kg 90Y-ibritumomab-tiuexetan (J-L).
Growth delay and median survival for all treatments
| Treatment . | Growth delay, d ± SE* . | Median survival, d ± SE . |
|---|---|---|
| NaCl | — | 21 ± 1 |
| rituximab (pooled) | 3 ± 1 | 44 ± 10 |
| 50 kBq/kg 227Th-rituximab | 5 ± 1 | 26 ± 3 |
| 200 kBq/kg 227Th-rituximab† | 17 ± 1 | > 119 |
| 400 kBq/kg 227Th-rituximab† | 15 ± 1 | > 81 |
| 1000 kBq/kg 227Th-rituximab† | 40 ± 7 | 75 ± 11 |
| 200 kBq/kg 227Th-trastuzumab | 0 ± 6 | 15 ± 2 |
| 400 kBq/kg 227Th-trastuzumab | 2 ± 1 | 20 ± 1 |
| 7.5 MBq/kg Zevalin® | 2 ± 2 | 33 ± 4 |
| 15 MBq/kg Zevalin® | 3 ± 1 | 26 ± 1 |
| 30 MBq/kg Zevalin® | 3 ± 1 | 23 ± 3 |
| Treatment . | Growth delay, d ± SE* . | Median survival, d ± SE . |
|---|---|---|
| NaCl | — | 21 ± 1 |
| rituximab (pooled) | 3 ± 1 | 44 ± 10 |
| 50 kBq/kg 227Th-rituximab | 5 ± 1 | 26 ± 3 |
| 200 kBq/kg 227Th-rituximab† | 17 ± 1 | > 119 |
| 400 kBq/kg 227Th-rituximab† | 15 ± 1 | > 81 |
| 1000 kBq/kg 227Th-rituximab† | 40 ± 7 | 75 ± 11 |
| 200 kBq/kg 227Th-trastuzumab | 0 ± 6 | 15 ± 2 |
| 400 kBq/kg 227Th-trastuzumab | 2 ± 1 | 20 ± 1 |
| 7.5 MBq/kg Zevalin® | 2 ± 2 | 33 ± 4 |
| 15 MBq/kg Zevalin® | 3 ± 1 | 26 ± 1 |
| 30 MBq/kg Zevalin® | 3 ± 1 | 23 ± 3 |
— indicates not applicable.
Delay in days to reach a mean tumor size of 1000 mm3 as compared with treatment with NaCl.
Growth delay significantly different from NaCl and rituximab (t test, P < .05) and median survival significantly different from NaCl and rituximab (Mantley-Cox log rank test, P < .001).
Effect of α-based radioimmunotherapy on survival of athymic mice with Raji xenografts. The mice were intravenously injected with saline, 20, 100, and 250 μg cold rituximab (A); 50, 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab (B); 200 and 400 kBq/kg 227Th-p-benzyl-DOTA-trastuzumab (C); or 7.5, 15, and 30 MBq/kg 90Y-ibritumomab-tiuexetan (D). Mice with tumor diameters greater than 20 mm were killed. Median survival times of treated groups were compared with control and cold rituximab (pooled) using the Mantley-Cox log-rank test: P < .001 for 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab. The rest of the treatments were not significantly different from the control group (NaCl). The groups receiving 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab had also significantly longer survival than the group receiving 20 μg cold rituximab (P < .05, Mantley-Cox log-rank test). The groups receiving 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab treatment groups were pooled in panel D, and the pooled group had significantly longer survival than all the 90Y-ibritumomab-tiuexetan treatment groups (P < .01, Mantley-Cox log-rank test). One mouse in the 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab group died after 42 days. n indicates the number of mice per treatment.
Effect of α-based radioimmunotherapy on survival of athymic mice with Raji xenografts. The mice were intravenously injected with saline, 20, 100, and 250 μg cold rituximab (A); 50, 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab (B); 200 and 400 kBq/kg 227Th-p-benzyl-DOTA-trastuzumab (C); or 7.5, 15, and 30 MBq/kg 90Y-ibritumomab-tiuexetan (D). Mice with tumor diameters greater than 20 mm were killed. Median survival times of treated groups were compared with control and cold rituximab (pooled) using the Mantley-Cox log-rank test: P < .001 for 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab. The rest of the treatments were not significantly different from the control group (NaCl). The groups receiving 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab had also significantly longer survival than the group receiving 20 μg cold rituximab (P < .05, Mantley-Cox log-rank test). The groups receiving 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab treatment groups were pooled in panel D, and the pooled group had significantly longer survival than all the 90Y-ibritumomab-tiuexetan treatment groups (P < .01, Mantley-Cox log-rank test). One mouse in the 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab group died after 42 days. n indicates the number of mice per treatment.
There was no significant effect of cold rituximab (Figures 5B-D, 6A). The highest dosage of cold rituximab used (10 mg/kg) is comparable to the clinical dosage used in humans (8.7 mg/kg).25 One animal treated with isotonic NaCl exhibited tumor shrinkage (Figure 5A). We speculate that tumor regression in this animal was related to an immunologic reaction induced by a wound on the tumor.
Radiolabeled trastuzumab, which targets HER2/neu, did not bind specifically to Raji tumors (Figure 2C) and had no significant therapeutic effect (Table 1; Figures 4B, 5I, 6C).
The commercially available β-emitting RIC, 90Y-tiuxetan-ibritumomab, which also targets CD20 presenting cells, had significantly less effect than 227Th-DOTA-p-benzyl-rituximab on tumor growth and survival (Table 1; Figures 4, 5J-L, 6D). However, despite the fact that treatment with 90Y-tiuxetan-ibritumomab resulted in successful inhibition of tumor growth in some cases (Figure 5J-L), it was much less striking than the effects of 200 to 400 kBq/kg of 227Th-DOTA-p-benzyl-rituximab. There was also a tendency to improved survival after treatment with 90Y-tiuxetan-ibritumomab, but the effect was not statistically significant when compared with the control group.
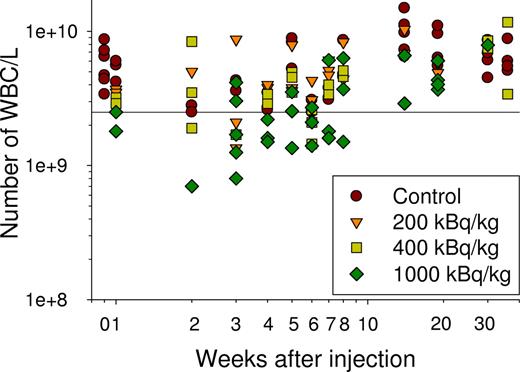
Toxicity of 227Th-DOTA-p-benzyl-rituximab
There was a dosage related reduction in the white blood cell (WBC) count after treatment with 227Th-DOTA-p-benzyl-rituximab (Figure 7). The WBC nadir was around 3 weeks following injection with maximum 1-log reduction in WBC count. In the control mice, the WBC count varied from 2.5 × 109 to above 10 × 109 per L blood. In the group receiving a therapeutic dosage of 200 kBq/kg, bone marrow suppression was modest, and after 4 weeks, the WBC count was within the range of the control mice. The mice receiving 400 kBq/kg showed more signs of bone marrow suppression, but after 7 weeks, the WBC count was within the range of the control mice. In the group receiving 1000 kBq/kg, the hemotoxicity was more pronounced, and 1 of 37 animals had to be killed due to fatigue and weight loss. However, only 2 mice in the 2- to 3-week time interval had lower WBC counts than 1.3 × 109/L, and the WBC count for animals in the 1000 kBq/kg group reached the level of the control mice after 14 weeks. The number of platelets was within the reference limits for most of the samples. A total of 3 mice in the group receiving 1000 kBq/kg had slightly lowered platelet counts 3 weeks after treatment (not shown). In conclusion, even at the highest dosage level, the hematologic toxicity was moderate.
Assessment of bone marrow toxicity of 227Th-p-benzyl-DOTA-rituximab. The number of WBCs was counted each week for 8 weeks and at 14, 19, 30, and 36 weeks after injection of NaCl and 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab. In weeks 1 and 5, the number of WBCs was counted using a hemolysis procedure; in all other time points, CBCs were obtained. (Horizontal line is lowest value of controls.)
Assessment of bone marrow toxicity of 227Th-p-benzyl-DOTA-rituximab. The number of WBCs was counted each week for 8 weeks and at 14, 19, 30, and 36 weeks after injection of NaCl and 200, 400, and 1000 kBq/kg 227Th-p-benzyl-DOTA-rituximab. In weeks 1 and 5, the number of WBCs was counted using a hemolysis procedure; in all other time points, CBCs were obtained. (Horizontal line is lowest value of controls.)
Discussion
We have demonstrated that 227Th-DOTA-p-benzyl-rituximab targets CD20-expressing Raji B-lymphoma tumor cells in vitro and in vivo, successfully inhibits tumor growth, and improves survival in mice, even though very small amounts of isotope were used. Since the therapeutic efficacy was so high with 200 kBq/kg 227Th-DOTA-p-benzyl-rituximab, the minimal required activity was probably between 50 to 200 kBq/kg, which can be extrapolated to 2.5 to 10 MBq for a 50-kg patient. Treatment with 227Th-DOTA-p-benzyl-rituximab was significantly superior to treatment with clinically relevant dosages of 90Y-tiuxetan-ibritumomab and rituximab. The upper dosage with rituximab and the middle dosage with 90Y-tiuxetan-ibritumomab correspond to the recommended dosages for clinical use in humans on a milligram per kilogram (mg/kg) and mega-Becquerel per kilogram (MBq/kg) scale, respectively. The safe human dosage of 227Th-DOTA-p-benzyl-rituximab is not known, and therefore a range of dosages was explored with this compound. The range of dosages selected for testing with 227Th-DOTA-p-benzyl-rituximab was based upon reported dosages in preclinical radioimmunotherapy with 225Ac,8 and the knowledge that 250 kBq/kg of the thorium daughter 223Ra is hematologically safe in humans.18 Also, in our study there was no evidence of delayed bone marrow toxicity, including myelodysplasia, even at the highest dosage level of 227Th-DOTA-p-benzyl-rituximab.
The in vitro cell growth data demonstrated that it was possible to obtain specific single-cell killing with low dose rate α radioimmunotherapy with 227Th. The mean number of α-particle hits per lymphoma cell necessary to inactivate more than 99% of the cells incubated with 211At-rituximab has been calculated to be from 15 to 50.26,27 Figure 1 shows that 400 Bq/mL of 227Th-DOTA-p-benzyl-rituximab significantly inhibited cell growth. At this activity concentration, 22 μBq was bound to each cell,16 corresponding to 1.9 α-disintegrations per day, or about 15 after 8 days. However, the amount of RIC bound to the cells will decrease with increasing incubation time.26 Furthermore, only a third of the α-particles are expected to hit the nucleus of lymphoma cells, assuming a cellular radius of 5.5 to 8.5 μm and a nuclear radius of 4.5 to 7 μm.28 Thus, with an initial activity of 400 Bq/mL, the nucleus of each cell was on the average hit by approximately 5 targeted α-particles in 8 days. In addition, the cells were hit by α-particles from unbound RIC, from RIC bound to neighboring cells, and from α-particles from daughter nuclides generated during the incubation period. However, it is likely that some of the cells were not affected because of the long half-life of 227Th. These cells divide with a speed similar to that of the control cells. Furthermore, the number of viable cells was probably overestimated, since cells undergoing early phases of apoptosis, necrosis, and mitotic catastrophe could not be distinguished from viable cells. Consequently, low dose rate α-radioimmunotherapy has significant cytotoxicity against single cells and, probably, micrometastatic disease.
To assess the ability to treat macroscopic tumors, 227Th-DOTA-p-benzyl-rituximab was injected into nude mice bearing macroscopic (32-256 mm3) human B-lymphoma xenografts. There was a large difference between the amount of activity of 227Th-DOTA-p-benzyl-rituximab in tumor and in normal organs, which indicates a large therapeutic window. From Figure 2, it can be estimated that a 0.5-g tumor receives 820 million α-hits if 200 kBq/kg 227Th-DOTA-p-benzyl-rituximab is injected. The density of the cells is approximately 1 mg/mm3, and the cell radius is approximately 7 μm (data not shown). We assume that 50% of the tumor is intercellular space. Thus, such a tumor would consist of 175 million cells, which corresponds to a mean of 4.7 α-particle hits per tumor cell nuclei if all α-particles are absorbed by tumor cell nuclei and an α-particle only impacts 1 nucleus. The uptake in the periphery of a large tumor is higher than in the central region of the tumor, but redistribution of RIC from inactivated cells in the periphery to viable cells in the core during the course of treatment may counteract heterogeneous tumor uptake.
Treatment with 1000 kBq/kg 227Th-DOTA-p-benzyl-rituximab had a significantly better effect on the early phase of tumor growth than 200 and 400 kBq/kg 227Th-DOTA-p-benzyl-rituximab, while the effect on long-term survival tended to be better at 200 kBq/kg. This apparent contradiction might be related to the higher hematologic toxicity of the 1000 kBq/kg dosage. It may be beneficial for long-term tumor control to have active immune cells, while short-term tumor control is more dependent on dosage level.
Several tumors had large necrotic cores, as determined by hematoxylin-eosin (HE) staining and microscopy. About 50% of the tumors had necrotic cores in the control mice, while approximately 90% of the tumors had necrotic cores in the mice treated with 227Th-DOTA-p-benzyl-rituximab. Thus, the high potency of 227Th may be attributed, at least in part, to its long half-life. Retention of the daughter nuclides, which also are α-emitters, in the tumor tissue may also have contributed to the favorable therapeutic effect.
Low-dose rate α-radioimmunotherapy seems to be beneficial against macroscopic tumors as well as single tumor cells. There may be both advantages and disadvantages of using low dose rates. Disadvantages may include tumor tissue repair due to proliferation and possible DNA repair, although the latter is less likely since α radiation causes mainly irreparable double-strand breaks in the DNA.29 The therapeutic level of 227Th found to be effective in this study was quite modest. The amount of 223Ra generated would probably not limit the use of 227Th, as indicated by the modest toxicity shown in recent clinical data on 223Ra in patients with prostate and breast cancer.10
The β-emitting, commercially available RIC 90Y-tiuxetan-ibritumomab, which also targets CD20 presenting cells, had significantly less effect than 227Th-DOTA-p-benzyl-rituximab. The uptake of 125I-ibritumomab-tiuxetan in tumor was significantly lower than the uptake of 227Th-DOTA-p-benzyl-rituximab. The immunoreactivity of 125I-ibritumomab-tiuxetan was 57%, which is acceptable. The tumor uptake in percentage of injected dose per gram 7 days after injection was 26% for 227Th-DOTA-p-benzyl-rituximab, 3% for 125I-ibritumomab-tiuxetan, and 19% for 125I-rituximab (data not shown). Thus, labeling of rituximab with 125I did not alter the tumor uptake significantly, indicating that 90Y-tiuxetan-ibritumomab is not as suitable for therapy of mice with lymphoma xenografts as radiolabeled rituximab. Consistently, Ma et al had to administer single injections of 278 to 370 MBq/kg 90Y-tiuxetan-ibritumomab to achieve a significant increase in median survival time in a Ramos xenograft model.30 The standard patient dosage of 90Y-tiuxetan-ibritumomab is 15 MBq/kg. It is noteworthy that 227Th-rituximab was significantly more effective than the clinically proven 90Y-tiuexetan-ibritumomab.
The recently developed method yielding stable constructs of 227Th-DOTA-p-benzyl-IgG in therapeutic quantities, and the demonstration of safe, efficacious use against a macroscopic tumor model, using modest dosages of isotope, suggest that clinical use of such targeted drugs is feasible. The 18.72-day half-life of 227Th would allow the drugs to be manufactured at a central radiopharmacy and shipped throughout the world. Because of the extraordinary potency of the α-emitting 227Th radionuclide, a limited amount of radioactivity would be required for therapeutic human use, permitting an economic and safe outpatient use. In addition, the half-life of 227Th may allow time to maximize the uptake in macroscopic tumors.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are indebted to Solveig Garman-Vik, Thomas Halvorsen, and Marita Martinsen, Department of Tumor Biology; Hanne Mali Thesen Møllergård, Department of Radiation Biology, for assistance with the animal work; to Miriam Valan, Algeta ASA, for assistance with measurements with the germanium detector; and the Central Laboratory at the Norwegian School of Veterinary Science for assistance with blood analyses. We thank Dag Rune Olsen, Department of Radiation Biology, Rikshospitalet Radiumhospitalet HE, for useful suggestions on data analysis. We are grateful to Kari Bjering and Arne Kolstad, Departments of Nuclear Medicine and Oncology, Rikshospitalet-Radiumhospitalet HF, for providing us with 90Y-tiuxetan-ibritumomab.
This work was supported in part by the MEDKAP program, the Norwegian Research council. O.W.P. is supported by National Institutes of Health grant R01 CA76287.
Authorship
Contribution: J.D and R.H.L. designed the experiments. J.D. wrote the manuscript. J.D., J.B., and A.K.H. performed the research. J.D. did the data analysis. J.B. and R.H.L. performed research and contributed the 227Th RICs. Ø.S.B., R.H.L., and T.J.J. contributed to the experimental design and writing of the manuscript. K.B.M., J.B., R.H.L., and J.D. performed research and did quality control of the 227Th RICs. O.W.P. contributed in writing the manuscript.
Conflict-of-interest disclosure: J.B. is employed by Algeta ASA, who owns the patent for using 227Th for radioimmunotherapy and has provided research support for this study. R.H.L. and Ø.S.B. are founders of Algeta ASA and have a significant stock interest. Ø.S.B. and O.W.P. are members of the scientific advisory board of Algeta ASA. J.D. and T.J.J. have a small amount of stocks in Algeta ASA. The remaining authors declare no competing financial interests.
Correspondence: Jostein Dahle, Department of Radiation Biology, the Norwegian Radium Hospital, Montebello, 0310 Oslo, Norway; e-mail: jostein.dahle@rr-research.no.