Abstract
Background: Monoclonal B-cell lymphocytosis (MBL) is characterized by the presence of a circulating population of clonal B-cells where the total B-cell count is <5 × 109/L and criteria for the diagnosis of other lymphoproliferative disorders are not present. In most patients the immunophenotype is similar to that of chronic lymphocytic leukemia with co-expression of CD19 and CD5. The natural history of MBL is unclear. We used the Mayo Clinic hematopathology database to identify patients with MBL and abstracted clinical information on natural history and prognostic parameters from clinical and research records.
Methods: After IRB review and approval, we reviewed the hematopathology records of 2292 patients seen at Mayo Clinic between August 1998 and May 2006 who had a clonal B-cell population on flow cytometry phenotypically consistent with CLL and fewer than <5 × 109/L B-cells. Clinical records were then reviewed to identify patients who fulfilled the criteria for MBL (no evidence of other lymphoproliferative disorders, no adenopathy on exam). Patient characteristics, prognostic parameters, and clinical outcomes were abstracted from the clinical and research records of these patients. Cox regression analysis was used to evaluate association between prognostic markers and time to treatment.
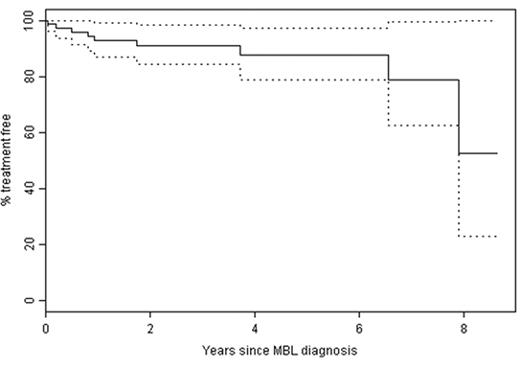
Results: A total of 118 patients meeting the criteria for MBL were identified. Median age at the time of MBL diagnosis was 69.4 years (range 39.0 – 91.4). A slight male preponderance was observed (54% male). CD38 status was available for 106 (90%) patients of whom 20% were CD38 positive using the 30% threshold to classify CD38. Cytogenetic analysis by fluorescent in situ hybridization (FISH) was available in 58 (49%) patients. Using the hierarchical classification system of Dohner and colleagues, 26 (44.8%) were 13q-, 10 (17.2%) were trisomy 12, 2 (3.4%) were 11q-, 1 (1.7%) was 17p-, and 19 were (32.8%) no defect was detected. ZAP-70 status was available for 32 patients of whom 22% were ZAP-70+ positive. IgVH gene mutation status was only available for 15 (12.7%) patients of whom 40% were unmutated. Time from MBL diagnosis to treatment is shown in Figure 1. Survival free of treatment was 92.7% (95%CI: 86.8–99.1%) at 1 year, 90.9% (95%CI: 84.2–98.2%) at 2 years, and 87.5% (95% CI: 78.7–97.4%) at 5 years. While age (p=0.68) and gender (p=0.14) were not found to be associated with time to treatment (TTT), CD38 status showed a strong relationship with TTT (p<0.001, HR: 22.7, 95% CI: 3.4–239.6).
Conclusion: The distribution of prognostic parameters (e.g. CD38, FISH) in patients with MBL appears similar to that of patients with early stage CLL. We observed a low rate of progression, with 5 year survival free of treatment greater than 87%. TTT among newly diagnosed MBL patients was associated with the CD38 status of clonal B-cells.
Author notes
Disclosure:Consultancy: Celgene (NE Kay). Research Funding: Bayer (TD Shanafelt and NE Kay) and Hospira (NE Kay) and Polyphenon E International (TD Shanafelt and NE Kay).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal