Abstract
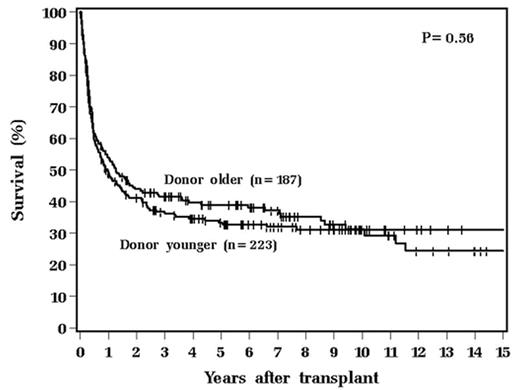
Fetomaternal and transmaternal sibling microchimerism might result in tolerance of hematopoietic stem-cell donors to recipients who were born before them. A single clinical study comparing first-born recipients and first-born donors provided evidence that birth order can have a significant impact on survival and on the incidence of acute graft-versus-host disease (GVHD) and relapse in HLA-identical sibling transplantation. In order to determine whether birth order might exert a consistent, biologically important effect, we compared survival and the incidence of acute GVHD, chronic GVHD, and relapse in recipients of HLA-identical transplants from sibling donors older than themselves to recipients with younger sibling donors. From 11/84 through 11/06, 410 first HLA-identical sibling transplants were performed. Patients were categorized by whether the sibling donor was older (n=187) or younger (n=223) than the recipient. As expected, the two groups differed with respect to patient age (P<0.001). The groups were similar with respect to gender, diagnosis, interval from diagnosis to transplant, extent of prior treatment, preparative regimen, stem-cell source, donor to patient gender, and CD34+ cell dose. Outcomes were estimated using the Kaplan-Meier Method and compared between the birth order groups using the log rank test. The incidence of acute GVHD, ≥ grade II acute GVHD, chronic GVHD, extensive chronic GVHD, relapse, survival, and disease-free survival were similar (0.39≤P≤0.85) between the two groups. The incidence of acute GVHD and survival in the two groups is shown below:
Figure
Figure
After adjustment for differences between the two groups, multivariable assessment of sibling birth order was not prognostic for survival (P=.32). Only older (P=0.029) and male donor/female recipient (P=.017) were independent prognostic adverse factors. In this large study of the HLA-identical sibling transplantation, no impact of birth order on the incidence of GVHD, relapse incidence, or survival was detected. Although (because of different methodologies) not directly contradictory to a previous study of birth order, the present results suggest that further study of the impact of birth order on outcome of HLA-identical sibling transplantation is needed. Suggestions that birth order be integrated into donor-selection algorithms or that matched unrelated donors might be preferred to high-risk HLA identical siblings are premature.
Author notes
Disclosure: No relevant conflicts of interest to declare.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal