Abstract
Introduction: The role of anti thymocyte globulin in GVHD prevention is well established, but it is also known that anti thymocyte globulin induces leucopenia and thrombocytopenia and as such might theoretically delay engraftment. Additionally, fast platelet engraftment is a marker for good hematopoietic stem cell graft function. We have prospectively compared the effect of Thymoglobulin on engraftment of granulocytes and platelets following a single non-myeloablative conditioning protocol in a randomized study.
Methods: 28 consecutive patients undergoing SCT were conditioned with the NST protocol (I.V.fludarabine 30mg/m2/day (days −10 to −5) and I.V. busulfex (3.2 mg\kg on days −6 and −5), with or without I.V. Thymoglobulin according to randomization (days −4 to −1). Thymoglobulin dosing schedule: a cumulative dose of 7.5 mg/kg r-ATG was given with the following program 0.5 mg/kg day −4, 2.0 mg/kg day −3, 2.5 mg/kg day −2, 2.5 mg/kg day −1. Patients were followed for engraftment of leukocytes and platelets.
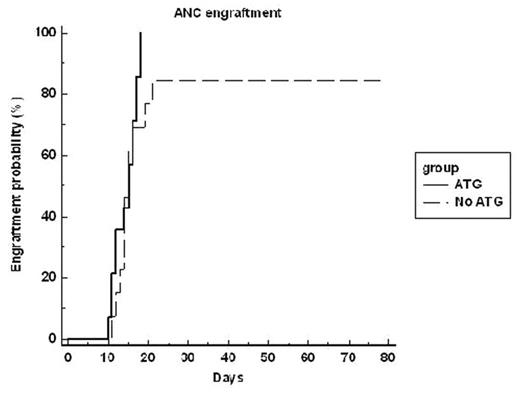
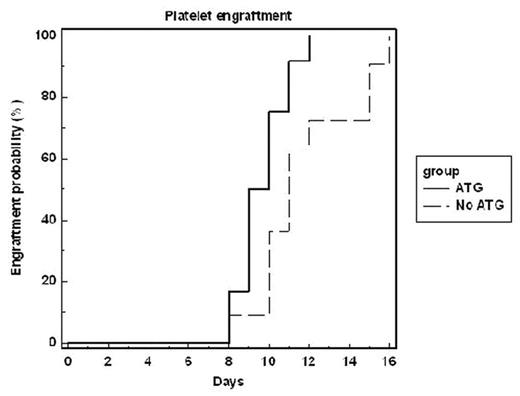
Results: only one patient rejected the graft (conditioned without Thymoglobulin, NS). In 4 patients underlying disease progression prevented engraftment of either ANC or platelets (2 per group). The median time to ANC engraftment was similar between the groups, 15±2.8 and 14±2.9 days for the Thymoglobulin and control groups respectively (figure 1, p=0.21). However, the median time for platelet engraftment was significantly shorter in patients receiving Thymoglobulin as part of the conditioning. Platelet recovery occurred 9.5±1.2 and 11±2.5 days for the Thymoglobulin and control groups respectively (figure 2, p=0.018).
Conclusions: in the non-myeloablative setting, Thymoglobulin induces faster platelet recovery and does not delay ANC engraftment.
Author notes
Disclosure:Research Funding: The study was supported by Genzyme.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal