Abstract
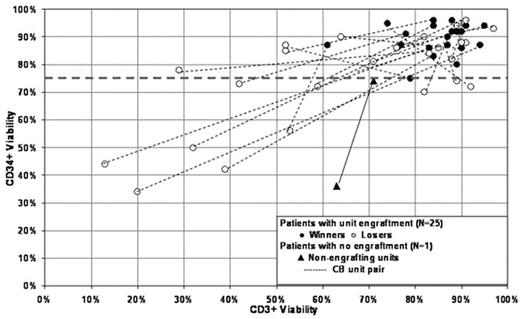
Compared to single unit historical controls double unit UCB transplantation (UCBT) has been associated with improved engraftment and survival in adult recipients, despite sustained donor engraftment of only one of the units. However, the mechanism of this advantage and unit predominance is not understood. Our hypothesis was that superior CD34+ and CD3+ viability (measured by 7-AAD staining) would be associated with unit predominance. Therefore, we evaluated 26 double unit UCBT recipients [median age 36 yrs (9–64); median weight 73 kg (40–111)] with high-risk hematologic malignancies who received myeloablative (n=15) or non-myeloablative (n=11) conditioning according to age and diagnosis. Units were 6/6 (n=2), 5/6 (n=25) and 4/6 (n=25) HLA-A, B antigen, DRB1 allele matched to the patient and ≥3/6 to each other. Flow cytometric evaluation was performed within 2 hours of thaw using CD45-FITC/CD34-PE/7-AAD/CD3-APC (dual-platform, modified ISHAGE protocol). 25/26 patients (96%) demonstrated donor engraftment by STR evaluation of day+21 bone marrow with one unit predominating (the “winner”). The % post-thaw CD34+ and CD3+ viability for the 26 double unit pairs is shown. Patients could be divided into 3 groups: 1) 10 in whom one of the 2 units had CD34+ viability ≥75% (always the winner) and the other <75% (always the loser); 2) 15 in whom both units had CD34+ viability ≥75% (either one was the winner); and 3) 1 in whom both units had CD34+ viability <75% and neither unit engrafted. CD3+ viability strongly correlated with CD34+ viability and was not an independent predictor of unit predominance. In univariate analysis infused viable CD3+ dose/kg was associated with unit predominance, while infused TNC/kg, viable CD34+/kg, CFU-total/kg, CFU-GM/kg, HLA-match and order of infusion were not. In summary, all engrafting units had CD34+ viability ≥75% and none of the units with CD34+ viability <75% engrafted (p: 0.007). Thus, in our analysis of unit predominance we have demonstrated that the % post-thaw CD34+ viability (but not the infused viable CD34+ dose) dictated the “engraftment potential” of a UCB unit, and, using the threshold of ≥75% viability, 12/52 units (23%) were unacceptable. When both CB units had CD34+ viability ≥75%, other factors (possibly related to CD3+ dose) determine unit predominance. Importantly, the finding that CD34+ viability is a marker of unit quality on the day of the transplant, if confirmed, has major implications for the clinical practice of UCBT. It suggests that double unit UCBT is superior because this approach significantly increases the chance that patients will receive at least one unit with engraftment potential.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal