Abstract
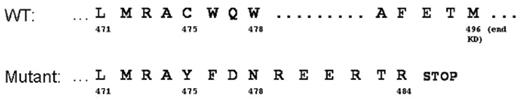
Although targeted inhibition of BCR-ABL with imatinib is an effective therapy for patients with chronic myeloid leukemia, a minority acquire mutations in the kinase domain (KD) that cause imatinib resistance. The spectrum of KD mutations thus far discovered, although quite heterogeneous, includes almost exclusively single nucleotide substitutions in key amino acids regulating drug binding or BCR-ABL function. Here, we describe a KD insertion/truncation mutation in 3 CML patients undergoing kinase inhibitor therapy. Two of these patients were being treated with imatinib (for 12 and 17 months), and one with dasatinib (for 13 months after a prior relapse while on imatinib). Suspected drug resistance was assessed by direct DNA sequencing of a BCR-ABL PCR product extending to the end of the kinase domain. Each of these 3 patients had 35 nucleotides from ABL intron 8 inserted at the normal exon 8–9 splice junction, after nucleotide 1423 (amino acid 475) of Genbank cDNA clone NM_005157. In all 3 cases, the mutation was co-expressed with wild type BCR-ABL sequence. The inserted sequence is derived from intron 8, beginning 1151 bp downstream from the normal splice donor site at the end of exon 8. This 35 bp intronic sequence is flanked by excellent consensus splice donor and acceptor sequences, suggesting alternative splicing as the likely mutational mechanism. The insertion creates a premature translational stop codon after 10 intron-encoded amino acids (figure), thus truncating 653 C-terminal amino acids including part of the KD and the entire last exon region - including a proline-rich domain, 3 nuclear localization signals, a DNA-binding domain, an actin-binding domain, and a nuclear export signal. These 3 insertion mutation cases were detected in our diagnostic clinical molecular pathology laboratory after sequencing 174 cases referred to us for suspected kinase inhibitor resistance, 78 of which contained a detectable mutation. The estimated prevalence of the exon 8/9 insertion/truncation mutation is then approximately 1.7% among patients with suspected drug resistance, and this mutation constitutes approximately 3.8% of all mutations.
Conclusion: Kinase domain insertions are an alternative (and not entirely uncommon) mutational mechanism in CML patients undergoing kinase inhibitor therapy. The functional significance in terms of kinase activity and drug resistance remains to be addressed.
Figure: Amino acid sequence of the C-terminus of the BCR-ABL kinase domain for the wild type and insertion/truncation mutant (with numbering as per GenBank cDNA clone NM_005157).
Figure: Amino acid sequence of the C-terminus of the BCR-ABL kinase domain for the wild type and insertion/truncation mutant (with numbering as per GenBank cDNA clone NM_005157).
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal