Abstract
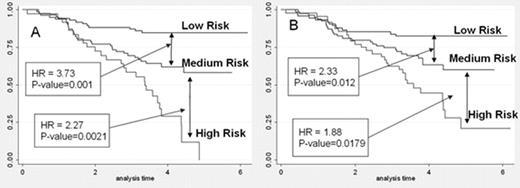
Gene expression profiling has significant potential to improve risk classification and therapeutic targeting in ALL. Our goal is to develop molecular classifiers that more reliably predict relapse or resistance to current treatment regimens in order to identify patients who may benefit from therapeutic intensification or experimental approaches. COG P9906, testing an augmented BFM regimen, enrolled 271 patients with B precursor ALL with NCI high risk features (older age/higher WBC) who had experienced very poor outcomes (45% EFS) on prior trials. Patients with favorable (trisomy 4+10/TEL-AML1) or very unfavorable (Ph+/hypodiploidy) genetics were excluded. Expression profiles (Affymetrix HG_U133Plus2) were obtained from pre-treatment leukemic blasts in 207/271 (76%) children on COG P9906; these 207 cases were representative of the overall cohort. EFS at 4 yrs was 61% and flow cytometric measures of MRD (flow MRD) at end-induction (day 28) were highly predictive of outcome. Using expression profiles, a molecular classifier predictive of EFS was modeled using a Cox regression-based supervised principal components analysis and modified score test with extensive nested cross validation. A 42 gene molecular classifier predictive of EFS differentiated this cohort into a low (4 yr EFS: 81%, n=109) and high (4 yr EFS: 50%, n=98) molecular risk group (log rank test, P< 0.0001). In multivariate analysis, the molecular risk classifier (MRC) retained prognostic significance (likelihood ratio test, p=0.0001) when adjusted for flow MRD and WBC. The best predictive model for EFS resulted when the MRC was combined with flow MRD; the resulting low (MRC low risk, MRD-; 87% EFS), medium (MRC low risk, MRD+ or MRC high risk, MRD-; 62% EFS), and high risk (MRC high risk, MRD+; 29% EFS) groups had significant outcome differences (Fig. A). As one must wait until the end of induction to obtain flow MRD to apply the combined classifier, we next determined if we could develop a molecular classifier to predict end-induction MRD in pre-treatment samples. Using a modified t-test and diagonal linear discriminant analysis with extensive cross validation, we derived a 23 gene molecular classifier predictive of end-induction MRD (ROC Accuracy: 0.80; p <0.0001). When the molecular classifier for MRD was combined with the molecular classifier for EFS, three distinct risk groups with significantly different outcomes were similarly defined (low risk: 82% EFS, medium risk: 63% EFS; high risk: 45% EFS; Fig. B). These studies demonstrate that molecular classifiers for EFS and MRD significantly enhance risk prediction in high risk B-ALL and may allow earlier intervention in induction in particularly high risk patients. Use of molecular classifiers to modify risk-adapted therapy has the highest priority in evaluating strategies to improve outcome in children with ALL and are currently being prospectively tested in COG trials.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal