Abstract
An urgent need exists to devise strategies to augment antiviral immune responses in patients with HIV who are virologically well controlled and immunologically stable on highly active antiretroviral therapy (HAART). The objective of this study was to compare the immunomodulatory effects of the cytokines interleukin (IL)–21 with IL-15 on CD8 T cells in patients with HIV RNA of less than 50 copies/mL and CD4 counts greater than 200 cells/mm.3 Patient CD8 T cells displayed skewed maturation and decreased perforin expression compared with healthy controls. Culture of freshly isolated patient peripheral-blood mononuclear cells (PBMCs) for 5 hours to 5 days with IL-21 resulted in up-regulation of perforin in CD8 T cells, including memory and effector subsets and virus-specific T cells. IL-21 did not induce T-cell activation or proliferation, nor did it augment T-cell receptor (TCR)–induced degranulation. Treatment of patient PBMCs with IL-15 resulted in induction of perforin in association with lymphocyte proliferation and augmentation of TCR-induced degranulation. Patient CD8 T cells were more responsive to cytokine effects than the cells of healthy volunteers. We conclude that CD8 T cells of patients with HIV can be modulated by IL-21 to increase perforin expression without undergoing overt cellular activation. IL-21 could potentially be useful for its perforin-enhancing properties in anti-HIV immunotherapy.
Introduction
Convincing evidence exists for a protective role of cellular immunity in HIV infection. For example, virologic control and detection of HIV-specific cytotoxic T lymphocytes (CTLs) are temporally related during primary HIV infection,1 and CD8 T-cell depletion results in widespread virus replication and disease progression in the simian immunodeficiency virus (SIV)–infected nonhuman primate model. In HIV infection, the failure of antiviral immunity has been attributed in part to qualitative CTL defects2–4 such as decreased perforin in total- and HIV-specific CD8 T cells in peripheral blood and lymphoid tissue, including gut-associated lymphoid tissues.5–8 Perforin defects are also evident in CTLs of patients who are on highly active antiretroviral therapy (HAART).2,9 The inability of most patients to keep HIV under control in the absence of potent antiretroviral therapy10,11 has led to the quest for immunotherapeutic approaches to augment antiviral cellular immunity
CD8 T cells can be identified phenotypically for their maturation status based upon expression of cell-surface maturation markers. For example, naive, central memory, effector memory, and effector subsets manifest differential expression of CD45RA and CD62L or CCR7,12 and perturbations in their distribution have been identified in HIV infection. Typically, naive and effector CD8 T cells are reduced, and effector memory subsets are expanded in patients with HIV who have only partial restoration with HAART.1–3 The major mechanism by which effector CD8 T cells kill virus-infected targets and tumor cells is via secretion of lytic molecules, namely perforin and granzymes.13,14 Lytic granules in CTLs are stored in a dense core within secretory lysosomes,15 and the membrane that encloses the granules contains lysosomal glycoproteins such as lysosome-associated membrane protein-1 (LAMP-1; CD107a), LAMP-2 (CD107b), and CD63.16 Soluble granule contents are released during exocytosis, and the incorporation of granule membrane proteins such as CD107a into the plasma membrane serve as markers of degranulation.
Preservation of memory and effector CD8 T-cell pools in vivo depends in part upon homeostatic proliferation which is regulated by cytokines and self-peptide MHC ligands for the T-cell receptor (TCR). It is now widely accepted that generation of long-term memory CD4 and CD8 T cells is dependent upon antigenic stimulation, but their survival is antigen independent and requires peripherally produced cytokines, particularly those that use the common γ-chain for signaling, such as interleukin (IL)–15.17–19 Another more recently described pleiotropic cytokine that uses the common γ-chain is IL-21, which is produced only by activated CD4 T lymphocytes and has significant sequence similarity to cytokines IL-2, IL-4, and IL-15.20–25 Based on the known T-cell–potentiating properties of IL-21 in tumor models,26,27 we hypothesized that IL-21 could augment the effector function of CD8 T cells in patients with HIV.
Patients, materials, and methods
Study subjects
Peripheral venous blood was collected from 20 patients with HIV with the following inclusion criteria: (1) age, 18 to 60 years (median, 45 years); (2) CD4-cell counts greater than 200/mm3 (range, 267-1198/mm3; median, 660/mm3); (3) plasma viral load (VL) lower than 50 HIV RNA copies/mL; and (4) HAART with 3 or more antiretrovirals for 12 or more months. All individuals signed informed consent in accordance with the Declaration of Helsinki, and as approved by the Institutional Review Board of the University of Miami. Ten healthy adult volunteers served as controls.
Reagents and mAbs
The following antihuman monoclonal antibody (mAb) reagents were purchased from BD Pharmingen (San Diego, CA): purified anti-CD3, anti-CD28, and anti-CD49d, fluorochrome-conjugated anti-CD3 (allophycocyanin [APC], Pacific blue, fluorescein isothiocyanate [FITC]); anti-CD8 (peridinin chlorophyll protein [PerCP], APC-Cy7); anti-CD62L (phycoerythrin [PE], APC); anti-CD45RA (FITC, PE Cy7, APC); anti-CD107a (FITC, PE Cy5), anti-IFNγ (PE or APC); antiperforin (FITC or PE); anti-CD25 (PE), anti-CD69 (FITC); anti-CD38 (PE); anti–HLA-DR (FITC); annexin V (PE); 7-amino-actinomycin (7-AAD) anti-pSTAT3 (PE), anti-pSTAT4 (PE), and anti-pSTAT5 (PE). APC-HIV gag MHC tetramers were purchased from Beckman Coulter (Fullerton, CA). Anti–granzyme B (PE) antibodies were purchased from Sanquin Reagents (Amsterdam, the Netherlands). Recombinant human (rh) IL-21 was a gift from ZymoGenetics (Seattle, WA). rhIL-15 was purchased from R&D Systems (Minneapolis, MN). Cycloheximide (CHX) was purchased from Calbiochem (San Diego, CA). 5,6-carboxyfluorescein diacetate succinimidyl ester (CFSE) was purchased from Molecular Probes (Eugene, OR).
PBMCs and purified CD8 T-cell cultures
Fresh peripheral-blood mononuclear cells (PBMCs) were isolated from healthy controls and patients with HIV using standard Ficoll-hypaque density centrifugation with Accu-Prep (Accurate Chemical & Scientific, Westbury, NY).28 CD3 and CD8 T cells were purified from PBMCs using the EasySep human T-cell enrichment and CD8 T-cell enrichment kits, respectively (StemCell Technologies, Vancouver, BC, Canada) according to the manufacturer's instructions. Purity of CD3 and CD8 T cells thus obtained was approximately 95%. PBMCs or purified CD3 T cells were cultured at 1 × 106cells/mL in RPMI 1640 complete medium (2 mL) in 14 mL polypropylene round-bottom tubes or in 96-well plates (200 μL) at 37°C, 5% CO2, and 100% humidity with IL-21 (50 ng/mL), or IL-15 (50 ng/mL) for periods of 5 hours and 5 days. A cytokine concentration of 50 ng/mL was chosen based on initial dose-response experiments with 10 to 100 ng/mL concentrations and published literature27,29 to achieve maximal effect on CD8 T-cell proliferation and antigen-specific CTLs. In different experiments, cells were examined for their maturation phenotype, and functional attributes were examined by flow cytometry. The cells were washed once and then fixed/permeabilized with 250 μL Cytofix/Cytoperm (BD Biosciences, San Jose, CA) according to the manufacturer's protocol30 and stained with antibodies specific for intracellular perforin and/or granzyme B. After 2 more washes, cells were resuspended in 1% paraformaldehyde (EM Science, Darmstadt, Germany) in PBS and acquired on the FACS Calibur and on an LSR II (Becton Dickinson, San Jose, CA) for 4-color or 6- and 7-color analyses, respectively.
In certain experiments, the CD3+CD8+ T cells were further differentiated based on expression of CD45RA and CD62L to distinguish 4 CD8 T-cell maturation subsets: CD45RA+CD62L+, naive (TN); CD45RA-CD62L+, central memory (TCM); CD45RA−CD62L−, effector memory (TEM); and CD45RA+CD62L−, effector (TE) CD8 T cells. Markers of immune activation were determined by the combinations of mAb reagent panels for CD3/CD8/CD38/HLA-DR at baseline and for CD3/CD8/CD25/CD69 at 24 hours following stimulation. Between 100 000 and 500 000 events were collected for each sample. Data were analyzed using Cell Quest Pro (BD Biosciences) and FLOWJO software (Tree Star, San Carlos, CA)
Analysis of lymphocyte-cell division by CFSE dye dilution
PBMCs from healthy volunteers and patients with HIV were labeled with CFSE at a concentration of 4 μM/5 × 106 cells for 10 minutes at 37°C as described previously.31 Labeling was terminated by addition of an equal volume of 100% fetal bovine serum (FBS). After 4 washes in 10% FBS in complete media, cells were cultured with appropriate stimuli for 5 days at 37°C/5% CO2. Cell division was analyzed in total CD8 T cells and CD8 T-cell subsets. In some experiments, cell proliferation analyses was performed in conjunction with perforin staining by 6-color flow cytometry using the following panel: CD3/CD8/CD45RA/CD62L/CFSE/perforin. Cells undergoing division were identified by the decrease in CFSE, resulting from dilution of the dye with each division. The medium-alone culture consisted of nonproliferating cells (CFSE bright) with less than 1% CFSE dim (proliferating) cells.
Lysosomal degranulation assay
Fresh PBMCs were reconstituted at 106/mL in complete media (RPMI 1640, 10% FCS, penicillin/streptomycin). Cells were stimulated according to published methods.32 Briefly, cells were cultured at 37°C and 5% CO2 with anti-CD28 (1 μg/mL), anti-CD49d (1 μg/mL), anti-CD107a mAb (10 μL/mL), monensin sodium salt (2 μM), brefeldin A (10 μg/mL), in the absence or presence of one of the following stimuli: IL-21 (50 ng/mL), IL-15 (50 ng/mL), and anti-CD3 (30 ng/mL) for 1, 2, or 5 hours. For blocking studies, CHX was added 30 minutes before the lysosomal degranulation assay and maintained during the period of stimulation (5 hours).
Simultaneous phosphospecific and surface mAb staining
Phosphospecific flow cytometry was performed as previously described.33 Briefly, PBMCs in RPMI 1640 with 10% FBS were stimulated with IL-21 (50 ng/mL), IL-15 (50 ng/mL), and IL-2 (1000 IU/mL) for 15 minutes at 37°C before fixation with 1.6% formaldehyde for 10 minutes, pelleted, resuspended in ice-cold methanol, and incubated for 30 minutes at 4°C. The cells were washed twice with staining medium (PBS containing 0.5% BSA and 0.02% sodium azide), resuspended at 106 cells/mL, stained for 30 minutes with a mixture of mAbs (including anti-CD3, and phospho-Stat [pSTAT3; Y705], pSTAT4, or pSTAT5 [Y694]), washed, and resuspended before acquisition. Typically, 250 000 to 300 000 events (> 1000 cells) were gathered per experiment.
Redirected cytotoxicity assay
Purified CD3 T cells from healthy donors and patients with HIV were cultured in medium with or without IL-21 or IL-15 for 24 hours as a source of effector cells and resuspended at appropriate concentrations for the desired effector–target-cell (E/T) ratio. Target cells (P815) were labeled with red fluorescent cell-linker PKH-26 Red34 (Sigma-Aldrich, St. Louis, MO) and washed 3 times in complete medium. The P815 cells were then incubated for 30 minutes on ice with 10 μg/mL of anti-CD3 mAb, resuspended in medium, and adjusted to 105 cells/mL. Effector cells were added to 100 μL target cells in 12 × 75-mm round-bottom polystyrene tubes (Falcon; BD Biosciences) to yield E/T ratios of 0:1, 6:1, 12.5:1, and 25:1, mixed by gentle tapping, centrifuged at 25°C for 4 minutes at 300 rpm (25g), incubated at 37°C for 4 hours, and stained with 5 μL 7-AAD for 10 to 15 minutes before data acquisition. A total of 100 000 events were collected per sample. Target cells were gated by side scatter, and PKH-26 fluorescence (FL2) and 7-AAD uptake was determined. Percentage of lysis was determined as [(% 7-AAD+ cells in test sample − % 7-AAD+ cells in negative control) / (100 × % 7-AAD+ cells in negative control)] × 100 as described.35,36
Apoptosis and cell-survival assay
Following culture, PBMCs from healthy volunteers and patients with HIV were washed twice with cold PBS, resuspended in 100 μL of 1 × binding buffer (10 mM HEPES [pH 7.4], 140 mM NaCl, and 2.5 mM CaCl2), and stained with 5 μL of annexin V–PE and 5 μL 7-AAD for 15 minutes at room temperature in the dark. Cells were diluted in 1 × binding buffer for acquisition by flow cytometry.37
RT-PCR
Total RNA was extracted from fresh and cultured purified CD3 T cells using the RNeasy kit (Qiagen, Valencia, CA) according to the manufacturer's instructions. The first-strand cDNA was synthesized using the Omniscript Reverse Transcription kit (Qiagen) with random hexaprimers. Perforin mRNA relative expression levels were quantified by real-time polymerase chain reaction (PCR) with the ABI/PRISM 7700 sequence detection system (Applied Biosystems, Foster City, CA), and primers and probes for perforin and the housekeeping gene, human hypoxanthine-guanine phosphoribosyl-transferase (HPRT) were obtained as assays on demand from Applied Biosystems. Each sample was examined for both perforin and HPRT in a final reaction volume of 25 μL using TaqMan Universal PCR Master Mix (Applied Biosystems), and amplification was carried out over 15 minutes at 95°C (denaturation step) followed by 40 cycles of 15 seconds at 94°C and 60 seconds at 60°C. The relative quantitation of perforin mRNA was carried out using the comparative threshold cycle (CT) method (2−ΔΔCT).38
Statistical analysis
Unpaired and paired t tests were used for analysis of differences between 2 groups. One-way analysis of variance (ANOVA) was used for analysis of differences between unstimulated and various stimulated cultures. P values less than .05 were considered statistically significant.
Results
Characterization of CTL populations in patients with HIV with undetectable virus load
Phenotype markers of CD8 T-cell maturation were evaluated in CD8 T cells in freshly isolated PBMCs from healthy controls and patients with HIV. Percentages of CD8 TN cells were lower in patients with HIV compared with healthy individuals (25.6% ± 3.3% vs 53.4% ± 5.8%; P < .001), whereas percentage of CD8 TEM cells in patients were increased (45.4% ± 3.5% vs 26.6% ± 2.9%; P = .002). As expected, in freshly isolated PBMCs, perforin was expressed by most TE and TEM subsets of CD8 T cells, followed by TCM. The CD8 TN-cell subset lacked perforin+ cells. In patients with HIV, perforin+ cells were significantly reduced compared with healthy controls in CD8 TEM (36.9% ± 7% vs 60.6% ± 7.2%; P = .002) and CD8 TCM (9.1% ± 2.2% vs 23.1% ± 3.8%; P = .04). However, there were more activated CD8 T cells that were HLA-DR+ in patients with HIV compared with healthy controls (29.5% ± 5.3% vs 7.8% ± 2.7%). Thus, the CD8 T cells of patients with HIV in this cohort exhibited a skewed maturation phenotype, lower perforin, and a higher basal state of immune activation, similar to the findings reported in other studies.1,3,39
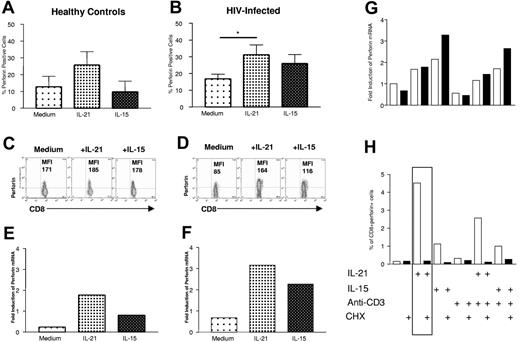
IL-21 up-regulates perforin expression in CD8 T cells
IL-2 and IL-15 are known to induce perforin gene expression in CD8 T cells.40–43 After 5 hours of culture with IL-21 or IL-15, perforin expression was up-regulated in CD8 T cells; this effect was more pronounced with IL-21 and was greater in patients with HIV than in HIV− volunteers. Percentages of perforin+ cells are shown in Figure 1A and 1B. There were more perforin+ cells in both TCM (16.6% ± 4.1% following IL-21 treatment vs 5.5% ± 1.5% in untreated cultures; P < .05) and TEM (45.6% ± 7.9% with IL-21 vs 21.1% ± 2.7% with media; P < .05) of patients with HIV (data not shown). Mean fluorescence intensity (MFI) of perforin in purified T cells cultured for 5 hours with IL-21, or IL-15 in representative healthy volunteers and patients with HIV is shown in Figures 1C and 1D. Increase in perforin MFI was greater in patient CD8 T cells than in control CD8 T cells with both IL-21 and IL-15, and the effect of IL-21 was stronger. In parallel, perforin mRNA expression by quantitative RT-PCR in purified CD3 T lymphocytes from the same individuals also showed higher perforin mRNA expression following 5 hours of culture with IL-21 (Figure 1E-F). IL-15 did not have as potent an effect as IL-21 on perforin mRNA expression in T cells in 5-hour cultures. Incubation of CD3 T cells with the protein synthesis inhibitor, CHX did not inhibit perforin mRNA (Figure 1G) but completely blocked the IL-21 and IL-15 induced perforin up-regulation (Figure 1H). These results demonstrate that IL-21 rapidly induces perforin mRNA transcription and protein synthesis.
IL-21 up-regulates perforin expression in CD8 T cells. Perforin expression (mean ± SEM) determined by intracellular flow cytometry in total CD8 T cells from healthy controls (A) and patients with HIV (B) after 5 hours of culture with medium, IL-21 (50 ng/mL), or IL-15 (50 ng/mL). *P < .05. Perforin expression determined by mean fluorescent intensity (MFI) in purified CD3 T cells from a representative healthy control (C) and patient with HIV (D) following 5 hours of stimulation with medium, IL-21, or IL-15, and corresponding perforin mRNA expression from the same healthy control (E) and patient with HIV (F) determined by quantitative RT-PCR. The effect of CHX on cytokine-induced perforin mRNA expression (G) and perforin protein expression (H) was analyzed in purified CD3 T cells that were cultured in medium or stimulated with IL-21 (50 ng/mL), IL-15 (50 ng/mL), anti-CD3 (30 ng/mL), and the combinations for 5 hours, with (solid bars) and without (open bars) CHX (10 μg/mL) treatment. Data for perforin mRNA in T cells and percentage of perforin+CD8+ T cells from 1 representative patient of 3 patients studied are shown.
IL-21 up-regulates perforin expression in CD8 T cells. Perforin expression (mean ± SEM) determined by intracellular flow cytometry in total CD8 T cells from healthy controls (A) and patients with HIV (B) after 5 hours of culture with medium, IL-21 (50 ng/mL), or IL-15 (50 ng/mL). *P < .05. Perforin expression determined by mean fluorescent intensity (MFI) in purified CD3 T cells from a representative healthy control (C) and patient with HIV (D) following 5 hours of stimulation with medium, IL-21, or IL-15, and corresponding perforin mRNA expression from the same healthy control (E) and patient with HIV (F) determined by quantitative RT-PCR. The effect of CHX on cytokine-induced perforin mRNA expression (G) and perforin protein expression (H) was analyzed in purified CD3 T cells that were cultured in medium or stimulated with IL-21 (50 ng/mL), IL-15 (50 ng/mL), anti-CD3 (30 ng/mL), and the combinations for 5 hours, with (solid bars) and without (open bars) CHX (10 μg/mL) treatment. Data for perforin mRNA in T cells and percentage of perforin+CD8+ T cells from 1 representative patient of 3 patients studied are shown.
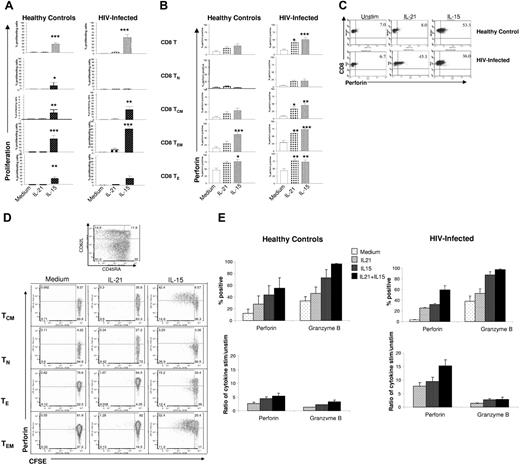
IL-21 does not induce proliferation of CD8 T cells from healthy volunteers or patients with HIV and induction of perforin expression is independent of cellular proliferation
We have previously demonstrated that CD8 T cells of patients with HIV undergo proliferation when cultured with the cytokines IL-2 or IL-15 in vitro.31 The influence of IL-21 on proliferation of CD8 T cells in healthy controls and patients with HIV was examined in 5-day cultures. CFSE-labeled PBMCs were cultured with IL-21 or IL-15 for 5 days and stained for cell-surface markers to identify different CD8 T-cell subsets. IL-21 did not induce proliferation in CD8 T cells in healthy controls or in patients with HIV (Figure 2A). In contrast, IL-15 induced significant proliferation in all CD8 T cell subsets in healthy control donors and in all subsets, except CD8 TN cells in patients with HIV. Cells cultured with cytokines for 5 days were also examined for perforin expression (Figure 2B). In healthy controls, CD8 TE and CD8 TEM subsets increased perforin with the addition of IL-15 alone and somewhat less so with IL-21. In patient PBMC cultures, however, addition of IL-21 or IL-15 resulted in a significant increase in perforin in total CD8 T cells as well as in CD8 TE, CD8 TCM, and CD8 TEM subsets. A dotplot showing the increase in perforin expression in CD8 TEM cells in IL-21– and IL-15–stimulated PBMC cultures from representative healthy controls and patients with HIV is shown in Figure 2C.
Induction of perforin expression in response to IL-21 is independent of a requirement for cellular proliferation. PBMCs from healthy controls and patients with HIV were cultured in the presence of the cytokines IL-21 (50 ng/mL) or IL-15 (50 ng/mL) for 5 days and analyzed for (A) proliferation by CFSE dye dilution and (B) perforin expression (mean ± SEM). Analysis was performed on total CD8 T cells as well as maturation subsets. Significance was determined by 1-way ANOVA, cytokine-stimulated versus unstimulated on day 5: *P < .05; **P < .01; ***P < .001. (C) A representative dotplot showing perforin expression in response to IL-21 and IL-15 in CD8 TEM cells from a healthy control and a patient with HIV. (D) Perforin expression in proliferating and nonproliferating CD8 T-cell maturation subsets of a representative patient with HIV. (E) Perforin and granzyme B expression in CD8 T cells of patients (n = 4) and healthy controls (n = 3). The top 2 panels show prercentages of perforin- or granzyme B–expressing cells; bottom panels show ratios of responses in cytokine-stimulated/unstimulated cultures. In panels A, B, and E, bars represent mean values with one standard error above the mean depicted on top of each bar. For dot plots depicted in panels C and D, numbers in each quadrant represent percentages of cells.
Induction of perforin expression in response to IL-21 is independent of a requirement for cellular proliferation. PBMCs from healthy controls and patients with HIV were cultured in the presence of the cytokines IL-21 (50 ng/mL) or IL-15 (50 ng/mL) for 5 days and analyzed for (A) proliferation by CFSE dye dilution and (B) perforin expression (mean ± SEM). Analysis was performed on total CD8 T cells as well as maturation subsets. Significance was determined by 1-way ANOVA, cytokine-stimulated versus unstimulated on day 5: *P < .05; **P < .01; ***P < .001. (C) A representative dotplot showing perforin expression in response to IL-21 and IL-15 in CD8 TEM cells from a healthy control and a patient with HIV. (D) Perforin expression in proliferating and nonproliferating CD8 T-cell maturation subsets of a representative patient with HIV. (E) Perforin and granzyme B expression in CD8 T cells of patients (n = 4) and healthy controls (n = 3). The top 2 panels show prercentages of perforin- or granzyme B–expressing cells; bottom panels show ratios of responses in cytokine-stimulated/unstimulated cultures. In panels A, B, and E, bars represent mean values with one standard error above the mean depicted on top of each bar. For dot plots depicted in panels C and D, numbers in each quadrant represent percentages of cells.
The results suggest that IL-21 induces perforin in CD8 T cells of patients with HIV in the absence of cellular proliferation. However, perforin expression among HIV-specific CD8 T cells has been reported to be linked to cell division in long-term nonprogressing patients with HIV.44 In order to conclusively determine the role of cellular proliferation in the induction of perforin expression in response to IL-21, CFSE-labeled PBMCs were analyzed for perforin expression in conjunction with maturation markers of CD8 T cells in the same cultures by multiparamater flow cytometry. As depicted in the example of a patient with HIV shown in Figure 2D, perforin expression was up-regulated in nonproliferating CD8 T cells following culture of PBMCs with IL-21, whereas with IL-15, induction of perforin expression was linked to cellular proliferation, which was maximal in the memory subsets.
Granzyme B expression in cytokine-treated CD8 T cells was also examined (Figure 2E). More cells expressed granzyme B than perforin at baseline in freshly isolated cells, and there was none or minimal effect of either cytokine after 5 hours (data not shown). After culture for 5 days, although more granzyme B+ than perforin+ CD8 T cells were present in medium- and cytokine-stimulated cultures, the fold increase in perforin was greater than for granzyme B by both IL-21 or IL-15 and their combination, as determined by the ratio of cytokine-stimulated to -unstimulated cultures.
IL-15, but not IL-21, enhances CD8 T-cell degranulation after anti-CD3 stimulation
Antigen-specific or anti-CD3 mAb–induced activation of human CD8 T cells leads to transient cell-surface expression of the degranulation marker CD107a.32 In order to identify degranulation by activated CD8 T cells, PBMCs were stimulated with soluble anti-CD3, IL-21, or both for periods of 1, 2, and 5 hours, and levels of intracellular perforin and cell-surface CD107a for each stimulus was assessed. In healthy donors, (Figure 3A; top row) the frequency of perforin+CD8+ T cells in unstimulated PBMCs decreased in the first hour of culture (Figure 3Ai) without expression of CD107a on the cell surface over the 5 hours of culture. With anti-CD3 stimulation (Figure 3Aii), CD107a was rapidly expressed on the cell membrane of CD8 T cells, becoming noticeable at 2 hours and greater at 5 hours, with 10% to 15% of CD8 T cells showing degranulation, concomitantly with decrease in perforin expressing cells. Addition of IL-21 alone to the cell cultures for 5 hours had no effect on the CD107a expression, but perforin increased after the initial dip at 1 hour (Figure 3Aiii). Cells cultured with IL-21 plus anti-CD3 manifested higher perforin expression in CD8 T cells at 5 hours (21.7% ± 6%) compared with cultures stimulated with anti-CD3 alone (8.2% ± 3%), while CD107a surface expression was not significantly increased by IL-21 addition (Figure 3Aiv).
Expression kinetics of intracellular perforin and degranulation following anti-CD3 and IL-21/IL-15 stimulation. IL-15, but not IL-21, induces significant degranulation and cytotoxicity in anti-CD3–stimulated CD8 T cells. (A) PBMCs were stimulated with anti-CD3 (30 ng/mL), IL-21 (50 ng/mL), and a combination for 1, 2, or 5 hours. Intracellular perforin (dashed line) and surface CD107a (solid line) expression were analyzed in CD3+CD8+ T cells by flow cytometry at baseline and after 1, 2, and 5 hours of culture in healthy individuals (top row) and patients with HIV (bottom row). Values depicted represent mean ± SEM. (B) PBMCs from patients with HIV were stimulated with anti-CD3 (30 ng/mL), IL-21 (50 ng/mL), and IL-15 (50 ng/mL) for 5 to 6 hours and analyzed for surface CD107a expression. Bars represent mean values and one standard error above mean for percent CD107+ CD8+ T cells. *P < .05. (C) A representative dotplot showing perforin and CD107a expression after 5 hours of stimulation in PBMCs from a patient with HIV. Numbers in quadrants indicate percentages of CD8+ T cells that are positive or negative for perforin, CD107a, or both. Boxed quadrants show differential effects of IL-21 and IL-15 on anti-CD3–induced degranulation and show that IL-21 induces de novo synthesis of perforin and does not promote degranulation. (D) Cytotoxicity of purified CD3 T lymphocytes from a healthy volunteer and a patient with HIV in a redirected cytotoxicity assay as described in “Patients, materials, and methods.” Purified CD3 T lymphocytes were cultured in medium or stimulated with IL-21 or IL-15 for 24 hours, and cytotoxicity was measured against P815 cell line. Data are shown as the percentage lysis that was determined as [(% 7-AAD staining sample − % 7-AAD staining of negative control) / (100% 7-AAD staining of negative control)] × 100.
Expression kinetics of intracellular perforin and degranulation following anti-CD3 and IL-21/IL-15 stimulation. IL-15, but not IL-21, induces significant degranulation and cytotoxicity in anti-CD3–stimulated CD8 T cells. (A) PBMCs were stimulated with anti-CD3 (30 ng/mL), IL-21 (50 ng/mL), and a combination for 1, 2, or 5 hours. Intracellular perforin (dashed line) and surface CD107a (solid line) expression were analyzed in CD3+CD8+ T cells by flow cytometry at baseline and after 1, 2, and 5 hours of culture in healthy individuals (top row) and patients with HIV (bottom row). Values depicted represent mean ± SEM. (B) PBMCs from patients with HIV were stimulated with anti-CD3 (30 ng/mL), IL-21 (50 ng/mL), and IL-15 (50 ng/mL) for 5 to 6 hours and analyzed for surface CD107a expression. Bars represent mean values and one standard error above mean for percent CD107+ CD8+ T cells. *P < .05. (C) A representative dotplot showing perforin and CD107a expression after 5 hours of stimulation in PBMCs from a patient with HIV. Numbers in quadrants indicate percentages of CD8+ T cells that are positive or negative for perforin, CD107a, or both. Boxed quadrants show differential effects of IL-21 and IL-15 on anti-CD3–induced degranulation and show that IL-21 induces de novo synthesis of perforin and does not promote degranulation. (D) Cytotoxicity of purified CD3 T lymphocytes from a healthy volunteer and a patient with HIV in a redirected cytotoxicity assay as described in “Patients, materials, and methods.” Purified CD3 T lymphocytes were cultured in medium or stimulated with IL-21 or IL-15 for 24 hours, and cytotoxicity was measured against P815 cell line. Data are shown as the percentage lysis that was determined as [(% 7-AAD staining sample − % 7-AAD staining of negative control) / (100% 7-AAD staining of negative control)] × 100.
In patients with HIV (Figure 3A; bottom row) fewer CD8 T cells degranulated following anti-CD3 stimulation, and the kinetics were slower, becoming evident at 5 hours (Figure 3Aii). The effect of IL-21 was to build up perforin in both unstimulated (Figure 3Aiii) and anti-CD3–stimulated cultures (Figure 3Aiv), without influencing degranulation.
In contrast to IL-21, IL-15 could significantly augment anti-CD3–induced degranulation, as shown in Figure 3B; this effect was especially prominent in CD8 TEM cells (data not shown). Because the perforin up-regulation with IL-21 was more potent than degranulation, there were increased proportions of CD8 T cells positive for both perforin and CD107a in IL-21–treated cell cultures compared with IL-15–treated cell cultures. A representative example illustrating frequency of dual perforin+ and CD107a+ CD8 T cells under different stimulation conditions from a patient is shown in Figure 3C: anti-CD3 alone, 7.4%; anti-CD3 plus IL-21, 14%; and anti-CD3 plus IL-15, 8.3%. The effector function of cytokine-treated CD3 T cells was examined in a redirected cytotoxicity assay against P815 cells labeled with anti-CD3 mAbs. Representative examples with T cells from a healthy donor and a patient with HIV are shown in Figure 3D. IL-15–treated T cells from the healthy donor showed cytotoxicity that was greater than that of medium- or IL-21–treated cells, particularly at higher effector–target-cell ratios. IL-21–treated T cells from the patient showed cytotoxicity that was equivalent to IL-15–treated cells, and greater than medium-treated T cells.
IL-2 and IL-15 predominantly activate STAT5 in CD3 T cells from both healthy individuals and patients with HIV, while IL-21 activates STAT5 and STAT3
The common cytokine receptor γ-chain (γc), shared by the receptors for IL-2, IL-4, IL-7, IL-9, and IL-15, is also a functional component of the IL-21R complex.30,24 In contrast to IL-15, which uses STAT5 for signaling, IL-21 preferentially activates STAT3.24,45,46 To investigate whether there is a difference in STAT signaling between healthy subjects and patients with HIV, phosphospecific flow cytometry for STATs was performed as shown in Figure 4. IL-2 and IL-15 strongly induced STAT5 phosphorylation in both healthy individuals and patients with HIV. Interestingly, basal and STAT5 phosphorylation induced by IL-2 and IL-15 was more pronounced in the patients with HIV. Furthermore, IL-21–stimulated CD3 T lymphocytes of patients with HIV demonstrated 7-fold higher phosphorylation of STAT3 compared with healthy subjects, as well as induced significant STAT5 phosphorylation. As expected, STAT4 was not activated by IL-21 in either healthy individuals or patients with HIV.
IL-2 and IL-15 predominantly activate STAT5 in CD3 T cells from both healthy individuals and patients with HIV, while IL-21 activates STAT5 and STAT3. PBMCs isolated from healthy individuals (A) and patients with HIV (B) were cultured in medium or stimulated with IL-2 (1000 IU/mL), IL-15 (50 ng/mL), and IL-21 (50 ng/mL) for 15 minutes, and expression of surface CD3 and phosphorylated epitopes for STAT3, STAT4, and STAT5 were determined on fixed and permeabilized cells by flow cytometry in healthy controls (n = 5) and patients with HIV (n = 3). Bars represent mean values of percentages of CD8+ T cells positive for phosphorylated STATs. Error bars depict one standard error above mean. (C) Representative histogram plots from 1 healthy control and 1 patient with HIV comparing STAT phosphorylation by medium or the cytokines IL-2, IL-15, and IL-21.
IL-2 and IL-15 predominantly activate STAT5 in CD3 T cells from both healthy individuals and patients with HIV, while IL-21 activates STAT5 and STAT3. PBMCs isolated from healthy individuals (A) and patients with HIV (B) were cultured in medium or stimulated with IL-2 (1000 IU/mL), IL-15 (50 ng/mL), and IL-21 (50 ng/mL) for 15 minutes, and expression of surface CD3 and phosphorylated epitopes for STAT3, STAT4, and STAT5 were determined on fixed and permeabilized cells by flow cytometry in healthy controls (n = 5) and patients with HIV (n = 3). Bars represent mean values of percentages of CD8+ T cells positive for phosphorylated STATs. Error bars depict one standard error above mean. (C) Representative histogram plots from 1 healthy control and 1 patient with HIV comparing STAT phosphorylation by medium or the cytokines IL-2, IL-15, and IL-21.
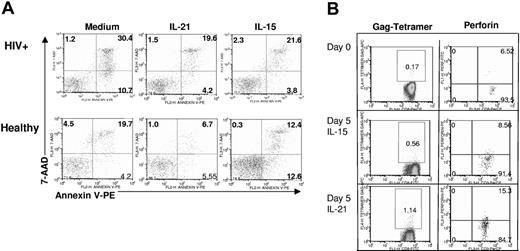
IL-21 protects cells from undergoing apoptosis and up-regulates perforin in HIV gag-specific CD8 T cells
We next determined the effect of the cytokines on cell death after 5 days in culture. PBMCs were analyzed for the expression of annexin V and 7-AAD expression in CD8 T cells. As shown in Figure 5A, addition of IL-21 or IL-15 to cell cultures protected the CD8 T cells from apoptosis, and the protective effect was more pronounced in cells from patients with HIV compared with healthy controls. HIV-tetramer+ CD8 T cells are also known to undergo spontaneous apoptosis in culture.47,48 HIV gag tetramer+CD8+ T cells from HLA-A2+ patients with HIV were examined for perforin expression after 5 days of culture with IL-21 or IL-15. Both cytokines were found to increase perforin expression in HIV gag-specific CD8 T cells (Figure 5B).
IL-21 protects cells from apoptosis and induces perforin in antigen-specific CD8 T cells. (A) PBMCs obtained from patients with HIV and healthy individuals were cultured in the presence or absence of IL-21 (50 ng/mL) or IL-15 (50 ng/mL) for 5 days and then stained with annexin V and 7-AAD to detect the percentage of apoptotic cells. Data were analyzed by using FLOWJO software. The results are representative of 2 independent experiments. (B) PBMCs isolated from a patient with HIV were cultured for 5 days with medium, IL-21 (50 ng/mL), and IL-15 (50 ng/mL). CD3+CD8+ T cells were gated to determine perforin expression in Gag-tetramer+ cells.
IL-21 protects cells from apoptosis and induces perforin in antigen-specific CD8 T cells. (A) PBMCs obtained from patients with HIV and healthy individuals were cultured in the presence or absence of IL-21 (50 ng/mL) or IL-15 (50 ng/mL) for 5 days and then stained with annexin V and 7-AAD to detect the percentage of apoptotic cells. Data were analyzed by using FLOWJO software. The results are representative of 2 independent experiments. (B) PBMCs isolated from a patient with HIV were cultured for 5 days with medium, IL-21 (50 ng/mL), and IL-15 (50 ng/mL). CD3+CD8+ T cells were gated to determine perforin expression in Gag-tetramer+ cells.
Discussion
CD8 T cells have been shown to play an important role in restricting HIV and SIV replication.49,50 Various mechanisms have been described to explain impaired CTL function in progressive HIV disease that include, among others, perforin deficiency in CD8 T cells of patients with HIV.51,52 Patients in the present study were on HAART and were aviremic with evidence for immune reconstitution of CD4 T cells, yet had decreased perforin-expressing CD8 T cells and exhibited delayed and incomplete degranulation of activated CD8 T cells, based on CD107a expression. A novel finding described herein is that the cytokine IL-21 induces perforin transcription in CD8 T cells of patients without concomitant cellular activation or degranulation.
Perforin degranulation in response to anti-CD3 stimulation was slower in CD8 T cells of patients with HIV, particularly in TEM, compared with those of healthy donors. The delayed CD8 T-cell degranulation in patients with HIV could be the result of defective phosphorylation of the ξ chain46,53 or a more distal signaling event in TCR-mediated signal transduction involving tyrosine kinases Lck, Fyn, and ZAP 70. Given the fact that the study patients were on HAART, it is also possible that 1 or more treatment drugs, which have been implicated in perforin and granzyme defects in such patients,9 contributed to the defective perforin degranulation in patient CD8 T cells. Regulation of perforin appears to be distinct from granzyme B, which had a higher basal level of expression. Only perforin was up-regulated by IL-21 at 5 hours, and also exhibited greater enhancement than granzyme B after longer periods of culture.
The rapid induction of perforin by IL-21 was evident within 5 hours and was noted also at 5 days, with maximal perforin expression in effector and memory subsets of CD8 T cells, including HIV gag tetramer+ cells. Failure of antigen-induced perforin up-regulation in HIV tetramer+ CD8 T cells of patients with progressive HIV disease has been associated with poor ability to undergo lymphoproliferation.44 In contrast, antigen-specific CD8 T cells from long-term nonprogressors have been shown to proliferate and concomitantly build up perforin in proliferating cells. The study presented here demonstrates that IL-21 was able to up-regulate perforin expression in CD8 T cells of patients with HIV that had minimal to no induction of proliferation, whereas the IL-15–induced perforin expression was associated with lymphoproliferation. Short-term cultures for 24 hours with IL-15, but not with IL-21, up-regulated activation markers CD69 and CD25. Unlike IL-21, IL-15 was also found to augment the surface CD107a expression in anti-CD3–stimulated cells, in agreement with the induction of cytotoxic activity in memory CD8 T cells that occurs with IL-15.54 Thus, it appears that IL-15 is more effective in the release of perforin from individual cells, but does so at the expense of inducing cellular proliferation and generalized cellular activation.
Regulation of the perforin gene in effector CD8 T cells and natural killer (NK) cells is biologically important and is not well understood. Interestingly, the magnitude of increase in both perforin protein and mRNA levels after culture for 5 hours was significantly higher with IL-21 than that observed with IL-15, and was greater in patients with HIV compared with healthy volunteers. A potential explanation for this phenomenon could be related to differences in perforin regulation by these 2 γc cytokines, as well as the state of activation of responding cells. The rapid increase of perforin mRNA by IL-21 did not require de novo protein synthesis. This is consistent with the rapid translational activation of pre-existing STAT proteins that are critical for cytokine receptor signaling.23 Recent studies have indicated that STAT proteins can regulate perforin gene expression via 2 enhancers and STAT5 in CTLs.43,55,56 It is well known that IL-2, and possibly also IL-15, regulate perforin expression at the level of transcription, directly inducing perforin transcription in CD8 T cells through STAT5 activation.42,43,55,56 IL-21 mainly activates STAT1 and STAT3, and only weakly activates the STAT5 protein in healthy persons,20,46,57 but the direct role of STAT1 or STAT3 in perforin regulation has not been established and needs to be investigated. Interestingly, in patient cells, STAT5 as well as STAT3 were both activated by IL-21. IL-21 may be regulating perforin transcription in the CD8 T cells of patients with HIV by activating these STATs, possibly as a result of the higher basal state of STAT3 in patient cells occurring in association with a heightened state of immune activation, as has been shown for NK-like cells.54 This idea would favor the likelihood of increased expression of the IL-21 receptor in patient cells, which is known to be up-regulated in activated T cells.58 The heightened sensitivity of patient cells to IL-21 was apparent also in the redirected cytotoxicity assay, wherein IL-21–treated effector T cells of patients were as efficient as IL-15–treated cells, whereas T cells of healthy controls were more responsive to IL-15 than to IL-21.
In summary, our data show that IL-21 increases perforin rapidly and significantly more than does IL-15, particularly in memory CD8 T cells, and does so more effectively in HAART-treated patients with HIV than in healthy controls. The novel action of IL-21 to rapidly stimulate perforin synthesis in memory CD8 T cells is a property that can potentially be exploited for therapeutic purposes for enhancing antiviral immunity in patients with diminished perforin stores in CD8 T cells. The lack of cellular activation by IL-21 could be considered a favorable attribute in the scenario of HIV infection, as it is desirable to avoid activation of resting/latent reservoirs of HIV.10
Authorship
Author contributions: L.W. and S.K. contributed equally to this work; they performed all culture experiments and flow cytometry analysis and contributed to writing the paper. N.S. contributed to data analysis and writing of the manuscript. H.L. performed RT-PCR experiments. M.A.K. contributed to patient selection and research design. M.L. contributed to study design. R.N.P. contributed to study design. S.P. developed and supervised the project and finalized the manuscript.
Conflict-of-interest statement: The cytokine IL-21 was provided free of charge by Zymogenetics, Inc. An unrestricted award of $30 000 was given in 2005 by Zymogenetics, Inc to S.P.
Correspondence: Savita Pahwa, Department of Microbiology and Immunology, 1580 NW 10th Ave, BCRI 712, Miami, FL 33136; e-mail: spahwa@med.miami.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgment
The authors thank the patients for their participation in this study and Mr James Phillips from the University of Miami Sylvester Comprehensive Cancer Center Flow Cytometry Core Facility for his assistance. IL-21 was a gift from ZymoGenetics, Inc. (Seattle, WA).
Supported by National Institutes of Health grant AI065293 to S.P.

![Figure 3. Expression kinetics of intracellular perforin and degranulation following anti-CD3 and IL-21/IL-15 stimulation. IL-15, but not IL-21, induces significant degranulation and cytotoxicity in anti-CD3–stimulated CD8 T cells. (A) PBMCs were stimulated with anti-CD3 (30 ng/mL), IL-21 (50 ng/mL), and a combination for 1, 2, or 5 hours. Intracellular perforin (dashed line) and surface CD107a (solid line) expression were analyzed in CD3+CD8+ T cells by flow cytometry at baseline and after 1, 2, and 5 hours of culture in healthy individuals (top row) and patients with HIV (bottom row). Values depicted represent mean ± SEM. (B) PBMCs from patients with HIV were stimulated with anti-CD3 (30 ng/mL), IL-21 (50 ng/mL), and IL-15 (50 ng/mL) for 5 to 6 hours and analyzed for surface CD107a expression. Bars represent mean values and one standard error above mean for percent CD107+ CD8+ T cells. *P < .05. (C) A representative dotplot showing perforin and CD107a expression after 5 hours of stimulation in PBMCs from a patient with HIV. Numbers in quadrants indicate percentages of CD8+ T cells that are positive or negative for perforin, CD107a, or both. Boxed quadrants show differential effects of IL-21 and IL-15 on anti-CD3–induced degranulation and show that IL-21 induces de novo synthesis of perforin and does not promote degranulation. (D) Cytotoxicity of purified CD3 T lymphocytes from a healthy volunteer and a patient with HIV in a redirected cytotoxicity assay as described in “Patients, materials, and methods.” Purified CD3 T lymphocytes were cultured in medium or stimulated with IL-21 or IL-15 for 24 hours, and cytotoxicity was measured against P815 cell line. Data are shown as the percentage lysis that was determined as [(% 7-AAD staining sample − % 7-AAD staining of negative control) / (100% 7-AAD staining of negative control)] × 100.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/109/9/10.1182_blood-2006-09-045278/4/m_zh80090700140003.jpeg?Expires=1765023409&Signature=4D3uNICKo24c9Zi6hUYoWriCXmtP-m~pFGeBZ01f7OWkGKRpJmDmSODc8-EEhn8jEzhLMLgFDuUssE8EtAvLicJLQYVEUaFyz3UCuqCQyjcYchnZpgpHvPXyESsXyUCVxxY58-ERvs0q6hW62ixrC1zext5yWtxWogbW~g9CWnkB4yTgE0WIiBD76i6n2pAai8rOLp3wic0w3mODnwzfau2968yJxByWxaZnx05BWEucum77fHUgxTG~q8DofgOWmuFHbkNc7sOxCWNelE335utkn62RcYZuQ~ufXiOfPiqh~683EZAt4oV7Iuc-cyNVC3PPYRwnZhBLkhRkrzVpDw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal