Abstract
The anticoagulant and anti-inflammatory enzyme, activated protein C (APC), naturally controls thrombosis without affecting hemostasis. We therefore evaluated whether the integrity of primary hemostasis was preserved during limited pharmacological antithrombotic protein C activator (PCA) treatment in baboons. The double-mutant thrombin (Trp215Ala/Glu217Ala) with less than 1% procoagulant activity was used as a relatively selective PCA and compared with systemic anticoagulation by APC and low-molecular-weight heparin (LMWH) at doses that inhibited fibrin deposition on thrombogenic segments of arteriovenous shunts. As expected, both systemic anticoagulants, APC (0.028 or 0.222 mg/kg for 70 minutes) and LMWH (0.325 to 2.6 mg/kg for 70 minutes), were antithrombotic and prolonged the template bleeding time. In contrast, PCA at doses (0.0021 to 0.0083 mg/kg for 70 minutes) that had antithrombotic effects comparable with LMWH did not demonstrably impair primary hemostasis. PCA bound to platelets and leukocytes, and accumulated in thrombi. APC infusion at higher circulating APC levels was less antithrombotic than PCA infusion at lower circulating APC levels. The observed dissociation of antithrombotic and antihemostatic effects during PCA infusion thus appeared to emulate the physiological regulation of intravascular blood coagulation (thrombosis) by the endogenous protein C system. Our data suggest that limited pharmacological protein C activation might exhibit considerable thrombosis specificity.
Introduction
Systemic anticoagulants can completely interrupt thrombus formation, but their usefulness is limited because their antithrombotic and antihemostatic activities are mechanistically tied. Highly effective plasma concentrations of systemic anticoagulants, such as those used for temporary thrombo-prophylaxis in interventional cardiology, prevent thrombin generation in both the blood vessel and the wound and can paralyze hemostasis with potentially fatal consequences. Due to safety considerations, the vast majority of patients who receive antithrombotic treatment are not anticoagulated to full efficacy. Thrombotic blood vessel occlusions causing myocardial infarction and ischemic stroke thus continue to contribute to mortality statistics.1 Until more thrombosis-specific intravascular anticoagulants become available, balancing the potential benefits and risks of systemic anticoagulation remains a critical hurdle for the clinician.
Occlusive thrombus formation is naturally down-regulated without bleeding complications most of the time following thrombogenic stimuli, such as blood vessel injuries or infections. It thus seems possible that selective pharmacological enhancement of the natural antithrombotic systems could achieve thrombosis specificity. Enhancement of the endogenous protein C pathway in the vicinity of thrombus formation might offer this wider therapeutic window. Thrombin is the natural protein C activator enzyme that activates protein C on such anatomic surfaces as the endothelial lining of blood vessels.2 Although low-dose thrombin infusion is antithrombotic, its safety is limited by systemic prothrombotic effects.3 The recent development of selective protein C activator (PCA) thrombin analogs offers viable, potentially useful alternatives.4–9 Unlike systemic anticoagulants, PCAs do not anticoagulate blood in the fluid phase, and their indirect anticoagulant activity is naturally targeted to the blood/lumen interface. Similar to native thrombin, injected PCAs bind to the transmembrane thrombomodulin and activate protein C in situ. Most thrombomodulin-dependent protein C activation occurs on the endothelial protein C receptor (EPCR), which is abundant in larger blood vessels.10–15 Accordingly, PCAs could be more specific for thrombus propagation that occurs in the intravascular boundary layer of blood flow than for hemostasis that occurs in the transvascular and extravascular space.
Since efficacy can be achieved by high enough doses of virtually all available anticoagulants, the critical question for each new approach to anticoagulation, including protein C activation, is whether it can offer hemostatic safety advantages over established methods. We thus tested the hypothesis that limited thrombomodulin-dependent endogenous protein C activation is safer than enhancement of the fluid-phase antithrombin system by systematically comparing the hemostatic safety of a PCA, the double mutant thrombin (Trp215Ala/Glu217Ala; WE), with equiefficacious doses of an indirect anticoagulant, low-molecular-weight heparin (LMWH, enoxaparin), in a primate model of hemostasis and acute large-vessel thrombosis.
Materials and methods
Antithrombotic agents
Low-molecular-weight heparin (LMWH), enoxaparin sodium, was from Sanofi Aventis (Paris, France). The injectable PCA formulation of recombinant WE thrombin was prepared and characterized as described and stored frozen until use.5,9 Lyophilized human activated protein C (APC) was from the American Red Cross (Bethesda, MD) and had anticoagulant activity comparable with recombinant APC (Lilly, Indianapolis, IN) in baboon plasma. Physiological saline with 2.5% dextrose vehicle was used for negative (“no treatment”) controls.
Experimental animals
The study was approved by the Institutional Animal Care and Use Committee. The pharmacodynamic effects of the antithrombotic agents were studied in a previously described primate model of hemostasis and thrombosis in which the antithrombotic effects of endogenous protein C activation were first demonstrated.3 Twenty one baboons weighing 9.1 kg to 13.1 kg were used in the studies, some for over a period of one year. The experiments consisted of temporary deployment of thrombogenic devices into chronic high-flow exteriorized arteriovenous shunts, administration of anticoagulants, bleeding time measurements, and blood sampling in restrained, conscious seated animals. Anxiety, if noted, was managed with low-dose ketamine (maximum: 2 mg/kg per hour) with or without diazepam (0.5 mg/kg per hour). All pharmacological agents were injected into, and blood samples were collected from, the shunts. Blood sampling was restricted to less than 2% of the blood volume on any experimental day. The thrombogenic device was removed after 60 minutes of perfusion, and the permanent shunt was reconnected. All shunts remained patent after each experiment.
Treatments
Treatments were administered by intravenous infusion, starting 10 minutes before placement of the thrombogenic device (see “Antithrombotic efficacy assessment,” below). The effects of intravenous LMWH were systematically evaluated in and around the reported clinically relevant dose range of interventional indications.16–20 Pilot studies with higher doses suggested significantly increased bleeding risk in the baboons. Lower doses were not tested. We administered an average dose of 1 mg/kg, divided into the following 4 groups: 325 (n = 5), 650 (n = 8), 1300 (n = 5), and 2600 (n = 3) μg/kg (72, 144, 289, and 578 nmol/kg, respectively; estimated averages). Half of the enoxaparin dose was given as a loading bolus (0 to 1 minute), followed by continuous infusion of the rest of the dose over the next 70 minutes. The dose range of PCA was determined based on pilot experiments and previous studies that explored the effects of up to 500 μg/kg WE.5,21 High PCA doses (≥ 110 μg/kg) caused profound temporary systemic anticoagulation with potential hemostasis impairment in baboons. For the present study, we elected to use a low average PCA dose of 4.2 μg/kg, divided into 3 subgroups: 2.1 (n = 5), 4.2 (n = 5), and 8.3 (n = 5) μg/kg (0.06, 0.12, and 0.23 nmol/kg, respectively), each administered as 1/3 bolus + 2/3 continuous infusion for 70 minutes. The effects of exogenous APC infusion were also tested. In early studies, a 20-fold dose range (100 μg/kg per hour to 2 mg/kg per hour) was evaluated for antithrombotic and anticoagulant activity in the baboon model. In the present study, APC was administered at 2 dose levels: 28 μg/kg (0.38 nmol/kg) continuous infusion for 70 minutes (n = 5), and an 8-fold higher dose (222 μg/kg [2.99 nmol/kg]) administered as 1/3 bolus + 2/3 continuous infusion for 70 minutes (n = 4). The former dose corresponds to the approved dosage form of recombinant APC for use in septic patients.
Hemostatic safety assessment
The hemostatic safety of LMWH, PCA, or APC administration was assessed as prolongation of the standard template skin bleeding time in comparison with the pretreatment baseline. The measurements were performed using an FDA-approved incision device (Surgicutt; International Technidyne, Edison, NJ). Sequential cuts were performed as instructed immediately before and approximately 40 minutes after the start of treatments. Any prolongation was considered to be an antihemostatic effect. Unlike several other bleeding time tests, this test has been shown to be sensitive for the detection of changes in hemostasis during the treatment of patients with antithrombotic or hemostatic products.22–24 The test has also been shown to be sensitive to the hemorrhagic effects of virtually all tested antithrombotic agents at antithrombotic doses, including direct thrombin inhibitors, activated protein C preparations, or glycoprotein αIIbβ3 inhibitors under experimental conditions in the baboon. Other safety observations included hemoglobin and hematocrit measurements, as well as thorough clinical monitoring of the study subjects.
Antithrombotic efficacy assessment
The equiefficacious doses of the anticoagulants were determined in a primate model as described in detail elsewhere.3 In brief, every animal received 125I-labeled purified baboon fibrinogen and 111In-tropolone–labeled autologous platelets for quantitative assessment of thrombus formation. Thrombus-forming conduit segments were deployed into the arteriovenous shunts during the last 60 minutes of anticoagulation. The device consisted of a 0.25-mL volume prosthetic vascular graft (4-mm ID), followed distally by a 20-mm long connector tubing and a 1.27-mL volume 9-mm ID silicone rubber extension segment (“thrombus chamber”). The flow rate was restricted to 100 mL/min during the experiment. Thrombosis was quantified as the total amount of deposited fibrin in the thrombus chamber. Inhibition of fibrin deposition in the thrombus chamber was quantified to establish the equiefficacious doses of LMWH and PCA. Real-time assessment of platelet deposition in the thrombus chamber provided additional information about thrombogenesis. Fibrin and platelet deposition were also determined in the graft segments.
Blood sample analyses
Blood samples (0.9 mL) were collected into 0.1 mL 3.2% citrate and 0.1 mL citrate/benzamidine in order to monitor select coagulation parameters immediately before and several times during thrombogenic device placements. Since the activated partial thromboplastin time (APTT) test is sensitive to both heparins and APC, it was used for monitoring the systemic effect of each injected anticoagulant. The APTT was determined in citrated plasma using a commercial point-of-care test (Rapid Point Coag; Bayer Diagnostics, Tarrytown, NY) between 5 and 7 minutes after blood drawing. To investigate the association between circulating APC levels and hemostatic safety or antithrombotic efficacy of the PCA, APC levels were also determined in both the PCA- and APC-treated animals using frozen citrate/benzamidine plasma samples, as described.25 The protein C zymogen levels were measured as described26 to assess potential substrate depletion during PCA treatment. Additional EDTA-anticoagulated samples were used for thrombus size calculations as described,3 and for monitoring potential adverse events, such as platelet and fibrinogen consumption, or bleeding. Additional 2-mL blood samples were collected into Phe-Pro-Arg-chloromethylketone (PPACK, 19 mM, 0.02 mL) for radiolabeled PCA distribution and binding studies in separate animals (see “Distribution of radiolabeled PCA, in vivo,” below).
Microscopy
Thrombi from thrombosis experiments and whole blood clots that were prepared in vitro were subjected to microscopic evaluation to quantify the differences between their leukocyte content. Grafts containing thrombi from untreated animals were fixed (4% formaldehyde), dehydrated, and paraffin embedded (n = 3). Whole blood samples (n = 3) were collected into glass tubes and allowed to clot and retract for 60 minutes before processing for microscopy. Phosphotungstic acid hematoxylin (PTAH)–stained sections were then prepared, and the number of nucleated cells was counted in 27 fields of view per sample. Images of PTAH-stained thrombus and blood clot sections were captured with a Nikon Optiphot-2 upright microscope (Nikon, Tokyo, Japan) with a Nikon Plan 20×/0.50 objective lens using an RT Slider camera (Diagnostic Instruments, Sterling Heights, MI) and SPOT 3.5 software (Diagnostic Instruments). The potential for interaction between leukocytes and PCA was studied by quantitation of leukocyte adhesion to immobilized PCA essentially as described.27 In brief, platelets and leukocytes were imaged using Köhler illuminated Normanski DIC optics with a Zeiss 63×/1.40 oil-immersion plan-apochromat objective lens on a Zeiss Axiovert 200m microscope (Carl Zeiss, Thornwood, CA). Images were captured with a Hamamatsu Orca 285 cooled digital camera (Hamamatsu City, Japan) and recorded using stallion 4.0 software (Intelligent Imaging Innovations, Denver, CO). Polystyrene 24-well plates were coated with PCA or thrombin for 3 hours at 37°C followed by washing and incubation with heat-inactivated fetal bovine serum (FBS) for 20 minutes at 37°C. Purified leukocytes (2 × 106/mL in HBSS buffer containing 0.2% BSA) were added to wells for 1 hour at 37°C in the absence or presence of EDTA (5 mM). Wells were then washed with HBSS and fixed with paraformaldehyde for 10 minutes, and the degree of leukocyte adhesion was recorded and quantified via phase-contrast video microscopy. To quantify platelet binding to PCA, washed red blood cells (RBCs) were reconstituted with fluorescently labeled platelets (2 μM DiOC6; Molecular Probes, Eugene, OR) before perfusion over PCA-coated coverslips at a shear rate of 300 s−1. In selected experiments, platelets were pretreated with the antiglycoprotein 1b alpha (GPIb, CD42b) monoclonal antibody 6D1 (generously provided by Dr Barry Coller). The degree of platelet rolling (transient platelet interactions lasting > 500 ms) on immobilized PCA was monitored in real time using fluorescence microscopy as previously described.28 In brief, platelets and leukocytes were imaged using KÖHLER illuminated Normanski DIC optics with a Zeiss 63×/1.40 NA oil-immersion plan-apochromat lens on a Zeiss Axiovert 200m microscope (Carl Zeiss, Thornwood, NY); images were captured with a Hamamatsu Orca 285 cooled digital camera (Hamamatsu City, Japan) and recorded using STALLION 4.0 (Intelligent Imaging Innovations, Denver, CO).
Distribution of radiolabeled PCA, in vivo
To investigate whether PCA directly and preferentially distributes into thrombi, radiolabeled PCA (125I-WE, 0.27 μCi [10 kBq]/μg, > 99% protein bound after dialysis) was infused (5 μCi [0.185 MBq] total; 1.8 μg/kg per hour intravenously) during thrombus formation for 60 minutes (n = 3). Radiolabeled PCA retention in the thrombus was determined following the method for measuring fibrinogen deposition.3 Blood samples (4 mL) were collected into PPACK at the end of the PCA infusion. After determining the radioactivity of the whole sample, the buffy coat was isolated and washed (2 × wash in HBSS buffer), and the retention of radioactivity by the cells was determined. Distribution of PCA in blood and binding of PCA to cells of the buffy coat were also determined in vitro by spiking PPACK-anticoagulated fresh whole blood with 125I-WE (270 pM) and following similar procedures.
Data analysis
The results are shown as means of the measured values, or as the mean ratio to or percentage of the baseline (pretreatment) values, as indicated. The 95% confidence interval and the number of experiments (n) are shown in parentheses after the means, unless otherwise stated. Error bars are displayed in the figures. The corresponding results of the treated groups were compared to preinfusion values within the group, or to the comparator group, as indicated. Means were compared using the t test. Corresponding groups of means, such as platelet deposition values over time, were compared between treatments using analysis of variance. Regression analysis was used to identify associations between study parameters and to evaluate dose response, and the correlation coefficients are shown. Results with P values of less than .05 were considered statistically significant. Nonsignificant results are labeled NS.
Results
Antihemostatic effects
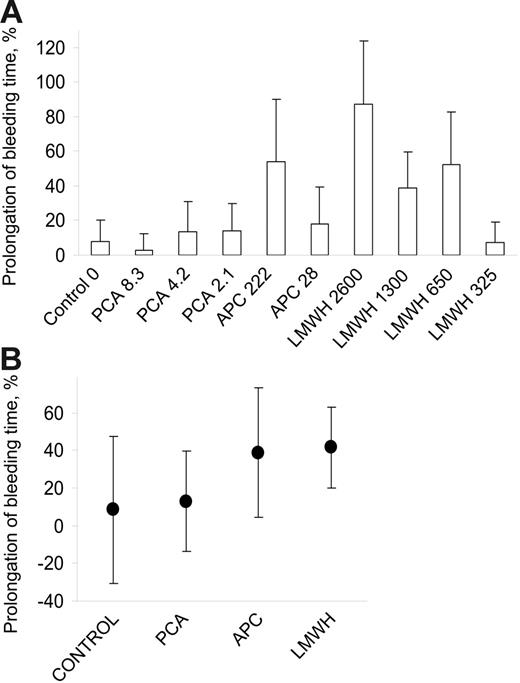
There were no hemorrhagic adverse events during treatments with LMWH, APC, and PCA. Pretreatment bleeding times averaged 3.55 (95% confidence interval: 3.35-3.76; n = 70) minutes. The changes in the bleeding time within individual treatment and dose groups are illustrated in Figure 1A. The number of experiments in each group was low for individual comparisons, and the t test for the mean differences between doses within treatments did not reach statistical significance. Regression analysis of dose versus response showed poor correlation in the LMWH treatment group, and no statistically significant slope for PCA and APC in the tested dose ranges. Figure 1B shows the average prolongations of bleeding times in the 3 active treatment (PCA, APC, and LMWH) and the vehicle treatment (negative control) groups. The bleeding time increased 1.46-fold, averaging 5.72 (4.42-7.02) minutes during treatments with LMWH (average dose: 1006 μg/kg, n = 23). The bleeding times during LMWH treatment were significantly longer than corresponding pretreatment controls in the same animals (P < .002, paired t test). APC also prolonged the bleeding time 1.42-fold, to 4.30 (3.60-5.00) minutes (average dose: 114 μg/kg), but this was only marginally significant (P = .03, n = 14). In contrast, 1.13-fold prolongation of the bleeding time averaging 3.4 (2.89-3.91) minutes during treatment with PCA (average dose: 4.9 μg/kg) was not statistically significant (P > .2, n = 15). Likewise, the 1.07-fold increase in bleeding time in vehicle-treated controls (n = 7) was not significant. One-way ANOVA comparing the no-effect levels with prolongations within treatment groups revealed similar results, indicating that LMWH treatment resulted in highly significant increase in bleeding time; APC treatment, in marginal increase; and PCA treatment or no treatment, in no significant bleeding time prolongation. While the mean bleeding time prolongations were not significantly different from the untreated controls in this analysis, the estimates for bleeding time prolongation for all treatments resulted in 6%, 9%, 31%, and 33% bleeding time increase projections for the average doses of vehicle, PCA, APC, and LMWH, respectively, assuming larger studies. The average increase in bleeding time was more prolonged during LMWH than PCA treatment (t test, one tail, P < .03), while, the average efficacies were not demonstrably different in statistical analyses.
Prolongation of the template skin bleeding time. Saline (control), protein C activator (PCA; Trp215Ala/Glu217Ala thrombin; WE thrombin), activated protein C (APC), or low-molecular-weight heparin (LMWH; enoxaparin) was administered intravenously to baboons. The bleeding time was determined on the volar surfaces of the lower arms using an FDA-approved method and device (Surgicutt). Several measurements were performed before treatment and between 40 to 60 minutes after the start of treatment. (A) The means of bleeding time prolongations in each treatment dose group and the vehicle-treated controls are shown with the error bars. The dose of the antithrombotic agent is given in micrograms per kilogram of body weight, administered over 70 minutes, and shown next to the treatment label. The 87% average bleeding time prolongation was statistically significant in the highest LMWH dose group. (B) The averages of bleeding time changes in the 4 treatment arms are shown with the 95% confidence intervals (bars). Short-term anticoagulation with PCA (n = 15, average dose 4.9 μg/kg) did not demonstrably impair the hemostasis. APC (n = 9, average dose: 125 μg/kg) had marginal effect and LMWH (n = 23, average dose: 1006 μg/kg) significantly increased the bleeding time.
Prolongation of the template skin bleeding time. Saline (control), protein C activator (PCA; Trp215Ala/Glu217Ala thrombin; WE thrombin), activated protein C (APC), or low-molecular-weight heparin (LMWH; enoxaparin) was administered intravenously to baboons. The bleeding time was determined on the volar surfaces of the lower arms using an FDA-approved method and device (Surgicutt). Several measurements were performed before treatment and between 40 to 60 minutes after the start of treatment. (A) The means of bleeding time prolongations in each treatment dose group and the vehicle-treated controls are shown with the error bars. The dose of the antithrombotic agent is given in micrograms per kilogram of body weight, administered over 70 minutes, and shown next to the treatment label. The 87% average bleeding time prolongation was statistically significant in the highest LMWH dose group. (B) The averages of bleeding time changes in the 4 treatment arms are shown with the 95% confidence intervals (bars). Short-term anticoagulation with PCA (n = 15, average dose 4.9 μg/kg) did not demonstrably impair the hemostasis. APC (n = 9, average dose: 125 μg/kg) had marginal effect and LMWH (n = 23, average dose: 1006 μg/kg) significantly increased the bleeding time.
Antithrombotic effects
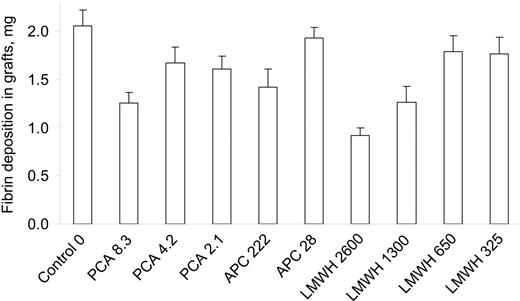
End-point fibrin deposition in the thrombus chamber during treatments with various doses of PCA, APC, and LMWH is shown in Figure 2A. Fibrin deposition averaged 2.12 (1.8-2.44) mg in untreated controls, and was lowered by all anticoagulants (P < .05 for each vs controls). PCA and LMWH were comparably efficacious in the tested dose ranges, since deposition of fibrin was inhibited by 82.9% (77%-88.8%) during PCA and 85.4% (80.2%-90.6%) during LMWH treatments (P = .50). Inhibition of fibrin deposition was less pronounced at 55.6% (36.7%-74.5%) during APC treatments (P < .02 vs both). The relative treatment efficacies were also determined as inhibition of fibrin deposition in the thrombus chambers at individual dose levels (Figure 2B). Fibrin deposition averaged 0.48 (0.35-0.61) mg during treatment with 2.1 μg/kg PCA (79% inhibition), which was not statistically different from the efficacy of enoxaparin at 325 μg/kg (72% inhibition; 0.63 [0.48-0.78] mg fibrin) or 650 μg/kg (86% inhibition; 0.33 [0.27-0.39] mg fibrin). PCA (8.3 μg/kg) and high-dose LMWH (1300 or 2600 μg/kg) virtually abolished fibrin deposition (> 90% inhibition, P < .05 versus other groups), indicating that these doses approached the upper limit of quantitative efficacy measurement in the thrombus chamber. There were modest correlations between the dose and antithrombotic effects of PCA (R2 = 0.80) or LMWH (R2 = 0.59).
Inhibition of fibrin deposition as a marker of antithrombotic effect in the thrombus chamber. Thrombogenic devices comprising a 4-mm diameter proximal Dacron graft segment and a 9-mm diameter distal thrombus chamber were deployed into the permanent arteriovenous shunts at 10 minutes after the start of PCA, APC, LMWH, or vehicle (control) infusion. Deposition of fibrin in the 1.27-mL thrombus chamber at 100 mL/minute blood flow rate was determined after 60 minutes of perfusion. (A) The means of fibrin deposition in each treatment dose group are displayed with error bars. All treatments significantly reduced fibrin accumulation by more than 50% but less than 95% in comparison with vehicle-treated controls. All doses of the PCA and enoxaparin doses of 650 μg/kg and above inhibited thrombus formation by more than 75%. (B) The average antithrombotic efficacies of treatments with PCA, APC, or LMWH were calculated as percent inhibition of fibrin deposition, compared with untreated controls, and are shown with the 95% confidence intervals. The antithrombotic efficacies of PCA (83%, n = 15, average dose 4.9 μg/kg) and LMWH (85%, n = 23, average dose: 1006 μg/kg) were comparable.
Inhibition of fibrin deposition as a marker of antithrombotic effect in the thrombus chamber. Thrombogenic devices comprising a 4-mm diameter proximal Dacron graft segment and a 9-mm diameter distal thrombus chamber were deployed into the permanent arteriovenous shunts at 10 minutes after the start of PCA, APC, LMWH, or vehicle (control) infusion. Deposition of fibrin in the 1.27-mL thrombus chamber at 100 mL/minute blood flow rate was determined after 60 minutes of perfusion. (A) The means of fibrin deposition in each treatment dose group are displayed with error bars. All treatments significantly reduced fibrin accumulation by more than 50% but less than 95% in comparison with vehicle-treated controls. All doses of the PCA and enoxaparin doses of 650 μg/kg and above inhibited thrombus formation by more than 75%. (B) The average antithrombotic efficacies of treatments with PCA, APC, or LMWH were calculated as percent inhibition of fibrin deposition, compared with untreated controls, and are shown with the 95% confidence intervals. The antithrombotic efficacies of PCA (83%, n = 15, average dose 4.9 μg/kg) and LMWH (85%, n = 23, average dose: 1006 μg/kg) were comparable.
The net platelet accumulation rate (NPAR), defined as the number of platelets deposited in successive 5-minute intervals, continuously increased in untreated controls, reaching 0.52 (0.41-0.62) billion platelets deposited during the last 5 minutes in the thrombus chamber (Figure 3A). Similar NPAR patterns of treatments produced with 4.2 μg/kg PCA and 650 μg/k LMWH suggested comparable antithrombotic efficacies. The NPARs were demonstrably smaller in all anticoagulated animals than in untreated controls from about the fortieth minute of thrombus growth. Total platelet accumulation in the thrombus chamber was significantly reduced in a dose-dependent manner by each anticoagulant (Figure 3B). The graft material provided robust thrombogenic stimulus and was less sensitive to the inhibitory effect of the anticoagulants than the distal thrombus chamber. Consistent with the findings in the thrombus chamber, the efficacy of PCA (26.6% inhibition of fibrin deposition) was not significantly different from the efficacy of LMWH (30.4% inhibition, P = .23) in the graft. The applied doses of APC moderately affected thrombus formation (18.6% inhibition of fibrin deposition) in the graft. In individual dose analyses, all doses of PCA, high-dose APC, and LMWH at 1300 μg/kg and above demonstrably inhibited fibrin deposition in the graft (Figure 4). The antithrombotic effect of the 2 lowest doses of LMWH did not reach statistical significance. The deposition of platelets in the graft was less affected by the anticoagulants (data not shown).
Inhibition of platelet deposition in the thrombus chamber. The number of deposited platelets was determined using gamma camera imaging in 5-minute intervals during thrombus formation in order to obtain kinetic information. The total doses of antithrombotic agents (μg/kg for 70 minutes) are displayed after the symbols and labels in the inset in panel B. (A) The effect on the net platelet accumulation rates (NPARs) of the intermediate doses of PCA (4.2 μg/kg) and LMWH (650 μg/kg), and the standard dose of APC (28 μg/kg) is shown. NPARs increased throughout the experiment in vehicle-treated controls. Treatment with PCA, APC, or LMWH slowed down the NPAR increase and, about 30 minutes after the start of thrombosis, decelerated the NPAR. The R2 for the polynomial regression of each displayed curve was above 0.85. (B) The absolute number of platelets residing in the thrombus is displayed every 5 minutes from deployment of the thrombogenic device at 10 minutes after start of treatment. The highest doses of PCA (8.3 μg/kg) and LMWH (1300 μg/kg and above) terminated platelet accumulation early, while the antithrombotic effect of the lowest doses of PCA and LMWH as well as of APC manifested the later. The means are shown with error bars.
Inhibition of platelet deposition in the thrombus chamber. The number of deposited platelets was determined using gamma camera imaging in 5-minute intervals during thrombus formation in order to obtain kinetic information. The total doses of antithrombotic agents (μg/kg for 70 minutes) are displayed after the symbols and labels in the inset in panel B. (A) The effect on the net platelet accumulation rates (NPARs) of the intermediate doses of PCA (4.2 μg/kg) and LMWH (650 μg/kg), and the standard dose of APC (28 μg/kg) is shown. NPARs increased throughout the experiment in vehicle-treated controls. Treatment with PCA, APC, or LMWH slowed down the NPAR increase and, about 30 minutes after the start of thrombosis, decelerated the NPAR. The R2 for the polynomial regression of each displayed curve was above 0.85. (B) The absolute number of platelets residing in the thrombus is displayed every 5 minutes from deployment of the thrombogenic device at 10 minutes after start of treatment. The highest doses of PCA (8.3 μg/kg) and LMWH (1300 μg/kg and above) terminated platelet accumulation early, while the antithrombotic effect of the lowest doses of PCA and LMWH as well as of APC manifested the later. The means are shown with error bars.
Deposition of fibrin in the Dacron vascular graft segments. Means are shown with SEM. This highly thrombogenic 0.25-mL section of the device was not sensitive for the detection of antithrombotic effects of the lower yet clinically effective doses of the LMWH. Overall, the inhibitory effects were negligible to moderate. The most pronounced decrease in fibrin deposition was observed during treatment with the highest dose of LMWH (2600 μg/kg), followed by comparable inhibition by 8.3 μg/kg PCA and 1300 μg/kg LMWH. The decrease in fibrin deposition by the lower doses of LMWH (325 and 650 μg/kg) and the lower APC dose (28 μg/kg) did not reach statistical significance.
Deposition of fibrin in the Dacron vascular graft segments. Means are shown with SEM. This highly thrombogenic 0.25-mL section of the device was not sensitive for the detection of antithrombotic effects of the lower yet clinically effective doses of the LMWH. Overall, the inhibitory effects were negligible to moderate. The most pronounced decrease in fibrin deposition was observed during treatment with the highest dose of LMWH (2600 μg/kg), followed by comparable inhibition by 8.3 μg/kg PCA and 1300 μg/kg LMWH. The decrease in fibrin deposition by the lower doses of LMWH (325 and 650 μg/kg) and the lower APC dose (28 μg/kg) did not reach statistical significance.
Circulating APC levels
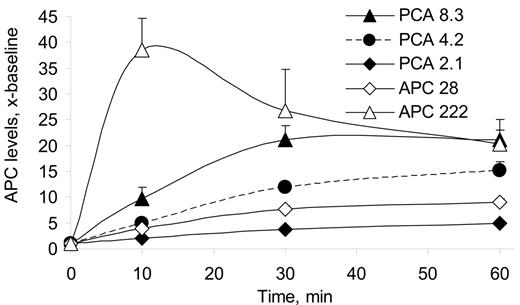
PCA infusion increased circulating APC concentration multiple-fold above the 5.6 (5.2-6.1)–ng/mL baseline in a dose-dependent manner (R2 = 0.94, P < .05) (Figure 5). APC levels averaged 3.6-, 10.7-, and 17.3-fold baseline at the 2.1-, 4.2-, and 8.3-μg/kg PCA dose levels, respectively, and reached 5.0-fold (3.4-fold to 6.6-fold), 15.1-fold (10.3-fold to 19.9-fold), and 21.1-fold (15.8-fold to 26.6-fold) pretreatment levels by 60 minutes. APC levels averaged 6.9-fold baseline during infusion of standard-dose APC (28 μg/kg for 70 minutes), and reached 9-fold (7-fold to 11-fold) baseline by 60 minutes. In the higher-dose APC treatment group, APC levels averaged 28.5-fold baseline, with highest level of 38.5-fold (32.4-fold to 44.7-fold) baseline at 10 minutes, and remained elevated 20.2-fold (15.3-fold to 25.1-fold) at 60 minutes. Consumption of circulating protein C zymogen (−11%) in the highest PCA dose group did not reach statistical significance (P = .35), and was even less notable at lower doses. PC zymogen levels were not expected to change and were not determined in other treatment groups.
Increase in circulating APC levels during infusion of PCA or APC. Circulating APC levels were determined using an enzyme immunocapture assay. Both treatments resulted in increased APC levels, with the highest values observed in the high-dose PCA (8.3 μg/kg) and APC (222 μg/kg) treatment groups. APC levels reached 5-fold over baseline by the end of low-dose PCA (2.1 μg/kg) infusion, and 9-fold in the lower-dose APC (28 μg/kg) treatment groups.
Increase in circulating APC levels during infusion of PCA or APC. Circulating APC levels were determined using an enzyme immunocapture assay. Both treatments resulted in increased APC levels, with the highest values observed in the high-dose PCA (8.3 μg/kg) and APC (222 μg/kg) treatment groups. APC levels reached 5-fold over baseline by the end of low-dose PCA (2.1 μg/kg) infusion, and 9-fold in the lower-dose APC (28 μg/kg) treatment groups.
Systemic anticoagulant effects
Although the global APTT test is not particularly sensitive to LMWHs, the interventional doses of intravenous LMWH were high enough to significantly prolong the APTT. The lowest to highest doses of LMWH increased the APTT 1.3-fold (1.3-fold to 1.4-fold), 1.7-fold (1.6-fold to 1.8-fold), 1.9-fold (1.6-fold to 2.2-fold), and 3.4-fold (2.0-fold to 4.5-fold), respectively. The 1.1-fold (1.0-fold to 1.2-fold) APTT increase during 2.1 μg/kg PCA treatment was not statistically significant. Infusion of 4.2 μg/kg and 8.3 μg/kg PCA caused 1.8-fold (1.5-fold to 2.2-fold) and 2.1-fold (1.3-fold to 2.8-fold) increase in APTT, respectively. APTT values remained near pretreatment levels at 1.3-fold (0.9-fold to 1.7-fold) baseline during 28 μg/kg APC infusion, while the higher dose increased APTT 2.6-fold (1.7-fold to 3.5-fold) after the bolus, and remained at 2.2-fold (2.0-fold to 2.3-fold) over baseline at 60 minutes. The APTT prolongations showed dose response for both PCA (R2 = 0.99) and LMWH (R2 = 0.96).
Associations between in vitro and in vivo study parameters
The correlation between all APTTs and the corresponding bleeding times was poor (R2 = 0.52, P < .03), although there was an association trend between APTT and the prolongation of the bleeding time in the LMWH treatment cohort (R2 = 0.86, P = .05). No association between APTT or APC levels and bleeding time prolongations could be shown during PCA treatment (R2 < 0.04 for both). APTT and circulating APC levels showed strong linear correlation (R2 = 0.99), regardless of whether PCA or APC was administered. The correlations between efficacies (inhibition of fibrin deposition) and systemic APC levels or APTT values within individual treatment groups were not significant.
Mechanistic assessment of PCA interactions with thrombi and blood cells, in vivo and ex vivo
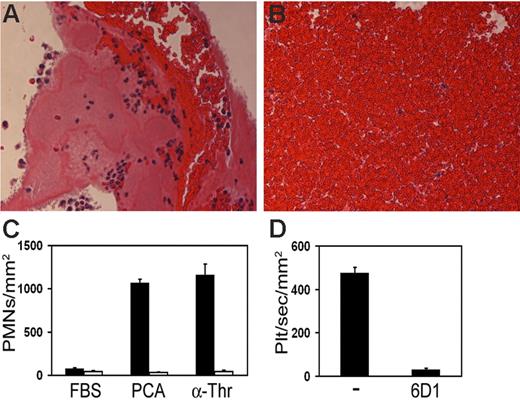
Consistent with previous reports, microscopy documented significant leukocyte accumulation in the experimental thrombi by 60 minutes (Figure 6A). Thrombi contained 25.3-fold (21.2-fold to 29.5-fold) more trapped leukocytes than corresponding fields of whole blood clot slides (P < .001) (Figure 6B). The majority of nucleated cells were polymorphonuclear (PMN) leukocytes. For comparison, the number of platelets in the 1.25-mL thrombus chamber reached 2.9 billion in untreated controls by the end of the experiment (Figure 3B). Since thrombi variably left more than two thirds of the lumen open by 60 minutes (estimate based on visual observations), untreated thrombi contained at least 10-fold more platelets than corresponding volumes of blood. Accordingly, leukocytes and platelets were incorporated into the thrombus at comparable rates. Immediately following the infusion of radiolabeled PCA, 0.025% ± 0.001% of the radioactivity was recovered in 1 mL blood. Cells in the washed buffy coat from the peripheral blood sample contained 38% of the total sample radioactivity. Washed hematocrit contained 28% of the radioactivity. The thrombogenic device (graft plus thrombus chamber), which corresponds to less than 0.001% of the entire estimated endothelial surface in a 10-kg baboon, contained 1.4% ± 0.8% of the injected total radioactivity, indicating robust local accumulation of PCA (0.26 μg PCA in the thrombus). Blood samples spiked with 270 pM radiolabeled PCA had 84% ± 3% bound to cells in the washed buffy-coat layer. This cell binding could be reduced only modestly to 75% ± 7% by addition of 100-fold molar excess of the unlabeled protein (n = 5, P = .01). Purified leukocytes bound to both immobilized PCA and α-thrombin ex vivo, and leukocyte-PCA and leukocyte-thrombin binding was completely blocked by the presence of EDTA (5 mM) (Figure 6C). Platelets tethered and rolled on immobilized PCA under shear flow conditions, and these platelet PCA interactions were abrogated in the presence of a blocking anti-GPIb mAb (Figure 6D).
Retention of leukocytes and platelets by thrombi, in vivo, or immobilized PCA, ex vivo. Standard light microscopy (PTAH stain) demonstrated the increased presence of trapped leukocytes in thrombi that developed for 60 minutes in the chamber region of the thrombogenic device. A representative section (A) shows the distribution of leukocytes in and around the thrombus that formed on the wall of a thrombus chamber. Thrombi were rich in fibrin and platelets, attracted leukocytes to their surface regions, and had relatively fewer red blood cells than the same volume of blood clot. For comparison of histology, blood that was clotted for 60 minutes before fixation is also shown in a typical section (B). Polystyrene 24-well plates were coated with PCA or thrombin for 3 hours followed by incubation with heat-inactivated FBS for 20 minutes. Purified leukocytes (2 × 106/mL) were placed on surface-immobilized PCA or thrombin (α-Thr) for 1 hour at 37°C in the absence (▪) or presence (□) of EDTA (5 mM) (C). To quantify the degree of adherent leukocytes, surfaces were washed with HBSS, fixed with paraformaldehyde, and imaged via phase-contrast microscopy. To quantify platelet-PCA interactions (D), fluorescently labeled platelets (plt; 2 μM DiOC6) were reconstituted with RBCs and perfused over PCA-coated coverslips at 300 s−1 for 3 minutes in the absence or presence of the anti-GPIb mAb 6D1 (20 μg/mL). Platelet rolling (transient platelet interactions lasting > 500 ms) was recorded in real time using fluorescence microscopy.
Retention of leukocytes and platelets by thrombi, in vivo, or immobilized PCA, ex vivo. Standard light microscopy (PTAH stain) demonstrated the increased presence of trapped leukocytes in thrombi that developed for 60 minutes in the chamber region of the thrombogenic device. A representative section (A) shows the distribution of leukocytes in and around the thrombus that formed on the wall of a thrombus chamber. Thrombi were rich in fibrin and platelets, attracted leukocytes to their surface regions, and had relatively fewer red blood cells than the same volume of blood clot. For comparison of histology, blood that was clotted for 60 minutes before fixation is also shown in a typical section (B). Polystyrene 24-well plates were coated with PCA or thrombin for 3 hours followed by incubation with heat-inactivated FBS for 20 minutes. Purified leukocytes (2 × 106/mL) were placed on surface-immobilized PCA or thrombin (α-Thr) for 1 hour at 37°C in the absence (▪) or presence (□) of EDTA (5 mM) (C). To quantify the degree of adherent leukocytes, surfaces were washed with HBSS, fixed with paraformaldehyde, and imaged via phase-contrast microscopy. To quantify platelet-PCA interactions (D), fluorescently labeled platelets (plt; 2 μM DiOC6) were reconstituted with RBCs and perfused over PCA-coated coverslips at 300 s−1 for 3 minutes in the absence or presence of the anti-GPIb mAb 6D1 (20 μg/mL). Platelet rolling (transient platelet interactions lasting > 500 ms) was recorded in real time using fluorescence microscopy.
Discussion
We investigated in primates a new concept for widening the therapeutic window of anticoagulation, that is, by making an attempt to use the naturally localized effect of protein C activation at the periphery of blood flow. First, we confirmed that intravenous enoxaparin was antithrombotic in the clinically relevant dose range. It also increased the template bleeding time consistent with several reports on the antihemostatic effects of LMWH.29–34 The bleeding time test, which remains the most reliable global marker of treatment-induced hemostasis impairment,22–24,35–37 was therefore used for the safety assessment of PCA treatment infusion in the equiefficacious dose range. While the absence of significant increase in the bleeding time during PCA infusion does not exclude the possibility of bleeding side effects,38 the direct comparison between LMWH and PCA strongly suggested that the latter was considerably safer. PCA treatment has been intended to target surface-associated thrombomodulin by inducing APC on the vascular endothelium. APC dissociates from the surface and diffuses across the boundary layer into the blood flow. Once systemic, APC has both antihemostatic and antithrombotic effects.5–9,21,39 The systemic anticoagulant and antihemostatic side effects of exogenous APC at about 10-fold above baseline levels have been documented in the clinic.39–41 Accordingly, when endogenous APC exceeds a critical plasma concentration, it is also reasonably expected to impair hemostasis. The lowest-dose PCA increased endogenous APC only 5-fold, which might explain its apparent safety. However, since even low doses of PCA have a potential to induce an unsafe increase in endogenous APC levels, a safe and still effective PCA dose would have to be established in appropriate clinical trials. While we did not directly assess risk, our data suggested that the risk of bleeding with equally effective PCA and LMWH treatments should be different. As with any anticoagulant, a PCA overdose remains a safety concern. However, we have already shown that a PCA overdose is inherently safer than overdose of other systemic anticoagulants, because it paradoxically down-regulates the protein C system.21 In contrast, the effect of systemic anticoagulants (eg, LMWH, APC) is not limited, and they are ultimately fatal by paralyzing hemostasis when overdosed. The short plasma half-life of APC,42,43 endogenous or exogenous, might provide some safety advantage over longer-acting therapeutic anticoagulants. The observed absence of direct antihemostatic effects during PCA anticoagulation, apparently even in the presence of relatively high APC levels at the higher doses, might be related to the thrombinlike nature of the PCA. PCA's limited yet detectable procoagulant activity might prevail in the extravascular wound environment in absence of the abundant substrate and cofactor supply that characterizes the high flow intravascular environment.
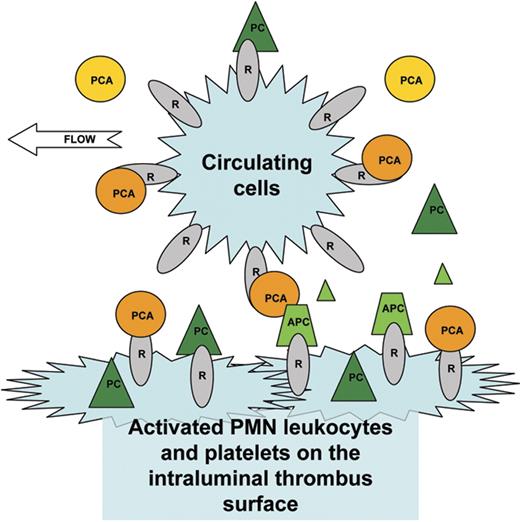
Our understanding of the mechanisms of actions of APC has been increasing since its introduction into the clinic.15 While the present study was not intended to test mechanistic hypotheses, the data provided insight into the potential antithrombotic mechanism of action of PCAs. Since the antithrombotic activity of α-thrombin is dependent on the activation of endogenous protein C,3 we assume the same for PCA. Like α-thrombin, PCAs also induce endogenous APC.3,5,21 The unexpected finding was that the lowest-dose PCA producing only 5-fold baseline APC level increase was more antithrombotic than the lower-dose exogenous APC producing a 9-fold baseline APC level increase. Moreover, the highest-dose PCA produced lower average systemic APC levels but was more efficacious than the higher-dose APC. Meanwhile, the tight correlation between APC and APTT suggested comparable anticoagulant activity of endogenous baboon and exogenous human APC in the animals. Circulating APC thus did not appear to be accountable for all of the observed antithrombotic effects of PCA. One of the possible explanations includes differences in the distribution of exogenous and endogenous APC. Laminar flow in a larger vessel could result in downstream accumulation of endogenous APC and local anticoagulation in the boundary layer where the cellular cofactors of protein C activation are located. In large vessels, EPCR could also retain or concentrate APC on the surface,44,45 thereby contributing to the efficacy of PCA. However, both in the applied model and possibly in vivo as well (eg, in case of a ruptured plaque), the initial thrombus forms on a surface that is unlikely to contain significant density of endothelial thrombomodulin and EPCR. Moreover, following the formation of an initial thrombus, the boundary layer is represented by the blood-thrombus interface anywhere in the circulation. While not readily accessible for quantitative assessment in vivo, we contemplate that a possible mechanism for increased local APC activity on the thrombus surface during PCA infusion could be related to the high cellular density of thrombi and the exposure of this interface to abundant supply of reactants by the passing blood. Since both the washed buffy coat of systemic blood and the thrombus had disproportionally high radioactivity following infusion of 125I-WE, circulating platelets and/or leukocytes appeared to be the vehicles that can effectively capture and/or deliver PCA to the thrombus. Some of it is not surprising, since platelets readily bind thrombin and our present data demonstrate that platelets also interact with the PCA, WE, specifically via GPIb, providing a direct mechanism for GPIb-dependent PCA recruitment to and enrichment on the thrombus surface. In addition, platelet thrombomodulin, about 60 copies per cell, could also capture some PCA and serve as a cofactor for protein C activation, in situ.46 The possibility of thrombomodulin-independent protein C activation by PCA concentrated on the thrombus surface cannot be excluded either. Binding of protein C to thrombus surface–associated (immobilized and activated) platelets could provide the necessary substrate for local protein C activation. The potential role of leukocytes has also been considered, because leukocytes match or even surpass platelets by mass in the thrombus, and because they also express both thrombomodulin (about 5000 copies per cell) and EPCR.47–51 Leukocytes pool and roll on growing thrombi under flow,52–54 and could deliver PCA for local protein C activation, or could capture and deliver APC via EPCR to the surface. However, activated leukocytes can inactivate thrombomodulin by oxidizing methionine 38851,55 ; thus it remains to be determined whether leukocyte thrombomodulin could function as a cofactor for PCA-catalyzed protein C activation in thrombi. Nevertheless, we found that purified leukocytes readily associate with PCA in the absence of EDTA, which was in agreement with the preferential association of radiolabeled PCA to the buffy coat of PPACK-anticoagulated whole blood. Taken together, our data provide evidence that both leukocytes and platelets specifically bind PCA. Of interest, washed RBCs (31% HTC) also retained radiolabeled PCA, although the quantity of RBC-associated radioactivity was negligible relative to the cell mass in this blood fraction. A hypothetical mechanism for cell surface–dependent local protein C activation by PCA is illustrated in a graphic (Figure 7) that depicts how circulating cells that form the cellular structural basis of thrombi could capture PCA in the circulation. In this model, cells carry and expose PCA to surface-associated protein C, resulting in antithrombotic APC accumulation in situ. In addition, concentrated PCA could directly compete with thrombin on the thrombus surface, or exposure of platelets and leukocytes to PCA might alter their thrombogenicity, thus providing a direct antithrombotic mechanism for PCA independent of protein C. These observations also raise the possibility that the intraluminal propagation of thrombi is naturally regulated by local generation of APC at the blood-thrombus interface essentially independent of the endothelial protein C system. While the exact molecular mechanisms of PCAs, in vivo, remain to be further explored, WE thrombin appears to be the most potent short-acting antithrombotic agent reported to date, reaching the efficacy of about 3 orders of magnitude more enoxaparin on a molar basis in primates. Since the equiefficacious doses of LMWH and PCA might be model specific, and could be different in various forms of thrombosis, appropriate dose-ranging clinical trials would be necessary to compare their safety in specific indications.
A hypothetical mechanism of the local antithrombotic effect of protein C activators. In this model, circulating cells (eg, platelets, leukocytes) serve as delivery vehicles that carry the pharmacological PCA to the thrombus. Infused PCA is absorbed from the plasma by high-affinity cellular transmembrane receptors (R), for example, by thrombomodulin and GPIb on circulating leukocytes and platelets, respectively. Some of these PCA-loaded cells encounter the thrombogenic site where they become activated, attach, and become the building blocks, entrapped in a fibrin network, of thrombi. The thrombus is characterized by a cell density comparable with some solid tissues, which disproportionally increases the local concentration of PCA, in situ, relative to circulating blood or the intact endothelium. The abundant activated membrane surface on thrombi attracts vitamin K–dependent coagulation factors, including protein C, and provides a platform for the catalytic conversion of protein C (PC) to APC by PCA. APC concentration increases locally, with some of the APC molecules staying on the surface, either receptor or directly membrane-associated. The APC-enriched surface acts as a local anticoagulant that down-regulates thrombin generation and interrupts thrombus propagation without profound systemic anticoagulant effect.
A hypothetical mechanism of the local antithrombotic effect of protein C activators. In this model, circulating cells (eg, platelets, leukocytes) serve as delivery vehicles that carry the pharmacological PCA to the thrombus. Infused PCA is absorbed from the plasma by high-affinity cellular transmembrane receptors (R), for example, by thrombomodulin and GPIb on circulating leukocytes and platelets, respectively. Some of these PCA-loaded cells encounter the thrombogenic site where they become activated, attach, and become the building blocks, entrapped in a fibrin network, of thrombi. The thrombus is characterized by a cell density comparable with some solid tissues, which disproportionally increases the local concentration of PCA, in situ, relative to circulating blood or the intact endothelium. The abundant activated membrane surface on thrombi attracts vitamin K–dependent coagulation factors, including protein C, and provides a platform for the catalytic conversion of protein C (PC) to APC by PCA. APC concentration increases locally, with some of the APC molecules staying on the surface, either receptor or directly membrane-associated. The APC-enriched surface acts as a local anticoagulant that down-regulates thrombin generation and interrupts thrombus propagation without profound systemic anticoagulant effect.
In summary, the present study supports the hypothesis that the antithrombotic and antihemostatic activities of limited pharmacological thrombomodulin-dependent protein C activation are dissociated. Low-dose PCA does not demonstrably impair the hemostasis, yet, it is as efficient as interventional doses of an established anticoagulant that has significant antihemostatic activity in primates. Very low-dose PCA infusion may therefore present the first example of an antithrombotic regimen with increased relative thrombosis specificity and potentially improved safety compared with an established systemic anticoagulant.
Authorship
Contribution: A.G. and E.D.C. designed research; A.G., U.M.M., M.A.B., O.J.T.M., E.I.T., and J.A.F. performed research; L.B., E.D.C., J.A.F., J.H.G., and S.R.H. contributed vital reagents and analytical tools; A.G., O.J.T.M., U.M.M., and J.A.F. collected data; A.G., E.D.C., O.J.T.M., J.H.G., and S.R.H. analyzed data; A.G. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: András Gruber, Department of Biomedical Engineering, BME-OGI, Oregon Health & Science University, 3303 SW Bond Ave, Portland, OR 97239; e-mail: grubera@ohsu.edu.
Presented in part at the 47th annual meeting of the American Society of Hematology, Atlanta, GA, December 12, 2005.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported primarily by National Institute of Health (NIH) grants HL73813 (E.D.C. and A.G.), and HL49413 and HL58141 (E.D.C.). Additional support was provided by NIH grants HL31950, HL52246, and HL63290 (J.H.G.); NIH grant RR00163 to the Oregon National Primate Research Center; and an American Heart Association grant 0665512Z (O.J.T.M.).
The assistance of Tonya Swanson and Sawan Hurst and the services of the surgical and anesthesia teams led by Dr John Fanton at OHSU/ONPRC are gratefully acknowledged. We thank Dr Barry Coller for the generous gift of the anti-GPIb monoclonal antibody 6D1. M.B. is a Hewitt ARCS scholar.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal