To the editor:
Several years ago, we described in Blood a group of patients who presented with acute, severe thrombocytopenia after taking acetaminophen (Tylenol; McNeil Consumer Healthcare, Guelph, ON, Canada) or naproxen (Aleve; Bayer Health Care, Morristown, NJ) and showed that in each case a platelet-reactive antibody dependent on a drug metabolite (acetaminophen sulfate or naproxen glucuronide) was the apparent cause of platelet destruction.1 We wish to describe here a patient who experienced repeated episodes of acute thrombocytopenia after taking acetaminophen who was sensitized to a different metabolite of acetaminophen: acetaminophen glucuronide.
A 4-year-old girl presented with florid petechial hemorrhages and a platelet count of 12 × 109/L (12 000/μL). Other hematologic indices were normal. Platelets returned to normal in 1 week. Four months later, she presented with fever, extensive petechiae and ecchymoses, and bleeding from the buccal mucosa. Her platelet count was 15 × 109/L (15 000/μL). In the belief she might have recurrent idiopathic thrombocytopenia (ITP), she was given prednisone. Platelets returned to normal in 4 days. Two months later, she had a third, virtually identical presentation. At this time, a possible connection between the thrombocytopenic episodes and ingestion of acetaminophen was suspected. Because it was felt to be medically important that the cause of the thrombocytopenic episodes be established and with the consent of parents, she was challenged 2 weeks later with a single 200-mg dose of acetaminophen. A few hours later, she developed a fever of 39°C. On the next morning, petechiae and ecchymoses were present, and the platelet count had dropped from 209 × 109/L (209 000/μL) to 17 × 109/L (17 000/μL). Platelets returned to normal in 4 days on prednisone. With avoidance of acetaminophen, she had no further episodes of thrombocytopenia over 18 months.
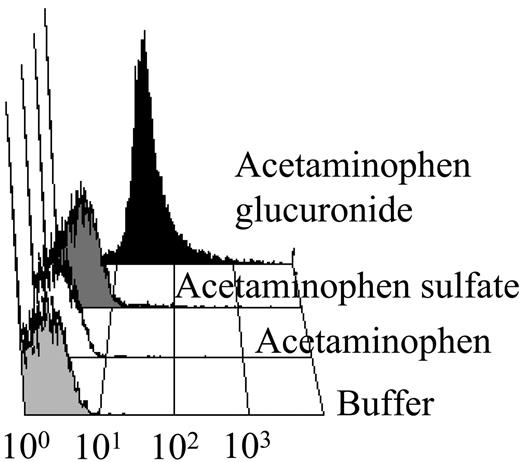
Using a flow cytometric assay,1 platelet-reactive antibodies specific for acetaminophen or acetaminophen sulfate could not be found in a blood sample taken 2 months after the fourth thrombocytopenic episode However, an IgG antibody was identified that reacted strongly with platelets in the presence of acetaminophen glucuronide (Sigma-Aldrich, St Louis, MO; Figure 1) at dilutions up to 1:100. Immunoprecipation studies1 showed that the antibody reacted with the platelet glycoprotein (GP) IIb/IIIa complex, but not with GPIb/V/IX.
The patient's antibody (1:5 dilution) reacted with normal platelets in the present of acetaminophen glucuronide, but not acetaminophen or acetaminophen sulfate. Washed platelets (5 × 106) were combined with patient serum in the presence or absence of 0.4 mM acetaminophen or the metabolite indicated in a final volume of 50 μL. After incubation for 1 hour, the platelets were washed in the presence or absence of the indicated drug or metabolite (0.2 mM). Bound human IgG was detected by the addition of FITC goat (Fab′)2 anti-human IgG (H+L) (1:200; Jackson Immunoresearch, West Grove, PA). No reaction occurred with normal serum under same conditions. Abscissa indicates mean platelet fluorescence intensity in arbitrary units.
The patient's antibody (1:5 dilution) reacted with normal platelets in the present of acetaminophen glucuronide, but not acetaminophen or acetaminophen sulfate. Washed platelets (5 × 106) were combined with patient serum in the presence or absence of 0.4 mM acetaminophen or the metabolite indicated in a final volume of 50 μL. After incubation for 1 hour, the platelets were washed in the presence or absence of the indicated drug or metabolite (0.2 mM). Bound human IgG was detected by the addition of FITC goat (Fab′)2 anti-human IgG (H+L) (1:200; Jackson Immunoresearch, West Grove, PA). No reaction occurred with normal serum under same conditions. Abscissa indicates mean platelet fluorescence intensity in arbitrary units.
These findings indicate that acetaminophen glucuronide, the major metabolite of acetaminophen, should be added to the list of drug metabolites capable of inducing antibodies and causing symptomatic thrombocytopenia upon re-exposure to the primary drug. At least 8 structurally characterized metabolites have now been identified as triggers for immune thrombocytopenia or hemolytic anemia.1-7 Of these, 4 are glucuronide conjugates, which are known to be capable of linking covalently and spontaneously to amine groups on proteins8 and inducing drug-specific antibodies, at least in mice.9 Many drugs (eg, nonsteroidal anti-inflammatory agents) implicated as triggers for immune cytopenia are conjugated to glucuronide prior to being excreted.10 Further studies to determine whether glucuronide conjugates are particularly prone to trigger immune responses leading to blood cell destruction or other immunologic conditions appear indicated.
Authorship
Correspondence: Daniel W. Bougie, BloodCenter of Wisconsin, PO Box 2178, Milwaukee, WI 53201-2178; dan.bougie@bcw.edu.
Supported by American Heart Association (AHA) grant 0235419Z and by grant HL-13629 from the National Heart Lung and Blood Institute.
Conflict-of-interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal