Abstract
Randomized studies testing the clinical efficacy of platelet additive solutions (PASs) for storage of platelets are scarce and often biased by patient selection. We conducted a multicenter, randomized study to investigate clinical efficacy of platelets stored in PAS II versus plasma, also including patients with clinical complications associated with increased platelet consumption. A total of 168 evaluable patients received pooled buffy coat–derived platelet concentrates (PCs) suspended in either plasma (n = 354) or PAS II (n = 411) stored up to 5 days. Both univariate as well as multivariate analysis showed a significant effect of used storage medium in regard to 1- and 24-hour count increments and corrected count increments, in favor of plasma PCs. However, there were no significant differences between the groups regarding bleeding complications and transfusion interval. Adverse transfusion reactions occurred significantly less after transfusions with PAS II PCs (P = .04). Multivariate analysis showed no significant effect of the used storage medium on the incidence of 1- and 24-hour transfusion failure. We showed safety and efficacy of PAS II PCs in intensively treated patients; however, plasma PCs show superior increments.
Introduction
The use of platelet concentrates (PCs) for the prevention and treatment of bleeding complications in patients with thrombocytopenia, due to cytotoxic therapy or malignancies of the bone marrow, is generally accepted. Despite the use of prophylactic platelet transfusions, bleeding is a frequent complication. Recommendations regarding the preferred transfusion regimen, the quantity and quality of transfused platelets, and strategies to monitor efficacy differ, and only a minority is evidence based.1,2
In recent decades storage of platelets suspended in nonplasma media (additive solutions) evolved as a growing field of interest. Possible advantages of using additive solutions instead of plasma are an increase of plasma available for plasma products, a reduction of plasma-related adverse reactions, improvement of storage conditions to increase the shelf life of PCs, and allowing photochemical pathogen reduction techniques. In the Netherlands, the National Blood Supply aims for harmonization of blood products used throughout the country. Currently, except when selected donors are required, all platelet products are prepared using the buffy coat (BC) method. On historical grounds, 2 platelet products are used: plasma-stored platelet concentrates (plasma PCs) and platelet concentrates stored in platelet additive solution II (PAS II PCs) (Trombosol; Baxter, Lessines, Belgium). However, there are no informative studies for a strong selection for one of these products. Although in vitro studies showed significant differences suggesting inferior quality in metabolic, functional, and flow cytometric parameters in platelets stored in PAS II as compared with plasma, platelets stored up to 5 days in PAS II stay within the range of minimal quality requirements.3-6 The correlation of these in vitro parameters with clinical efficacy is inconsistent.7-9 One paired radiolabeled platelet survival study showed a significant decrease in both recovery as well as survival of PAS II PCs compared with plasma PCs and PCs stored in PlasmaLyte A (Baxter, Deerfield, IL).10 Data regarding the clinical transfusion response of platelets stored in PAS II are also limited. A small, nonrandomized clinical trial did not show a significant difference between PAS II PCs and plasma PCs, and one small prospective, randomized study reported that corrected count increments (CCIs) after transfusion with PAS II PCs were significantly lower.11,12 Despite lower CCIs bleeding complications did not differ, and the latter study reported a significant reduction in transfusion reactions.11 Observational analysis of the transfusion response of PAS II PCs and plasma PCs, used in the control arm of a randomized trial evaluating pathogen-inactivated platelets (euroSPRITE), did not show significant differences.13,14 A major drawback of these studies was the exclusion of patients with clinical factors known to increase platelet consumption.12-14 Because several studies show the importance of patient-related factors in relation to platelet transfusion response, we performed a randomized, controlled, double-blinded study to evaluate the therapeutic efficacy and safety of PAS II PCs in a nonselected patient population.15-19
Patients, materials, and methods
Patients and study design
The study protocol was approved by the Leiden University Medical Center (Leiden, The Netherlands) and HagaZiekenhuis (The Hague, The Netherlands), ethics committees and conducted according to the Guidelines of Good Clinical Practice. All patients older than 18 years who needed or were expected to need more than 2 platelet transfusions were eligible. After informed consent patients were randomized to receive PAS II PCs or plasma PCs. Patients with HLA and/or HPA alloantibodies, active immune thrombocytopenia, or an indication for CMV-negative blood products (CMV-negative patients receiving stem cells of CMV-negative, unrelated or HLA-mismatched donors) were excluded. Patients were enrolled at the hematology departments of Leiden University Medical Center and Haga-Ziekenhuis. Inclusion was restricted to a maximum of 30 days after the first PC transfusion or a maximum of 8 PC transfusions, whichever occurred first. The inclusion period ended in case of informed consent withdrawal, the occurrence of immunologic refractoriness, after request of the patient or the treating physician, or in case of reaching 30 days after the first PC or 8 PC transfusions. In case of the latter 2, a second randomization was allowed. After randomization, age, sex, height, weight, diagnosis, intended treatment, existence of an enlarged spleen (by physical examination and/or imaging techniques), medical history, transfusion history, and medication were recorded. Blood samples were tested for ABO-RhD blood group, irregular red blood cell antibodies, hemoglobin, hematocrit, white blood count, platelets, HLA and HPA alloantibodies, and antiplatelet autoantibodies. During the inclusion period, platelet and red-cell transfusions, transfusion-related adverse reactions (skin reactions, fever elevated 2°C, dyspnea, hypotension), bleeding complications, mucosal damage, fever, infections, and used medication were recorded. Bleeding complications were graded according to the World Health Organization criteria, and mucosal damage was graded according to the Common Toxicity Criteria (version 2.0).20,21 Both parameters were reviewed on a daily basis. Infections were scored positive in case of positive cultures or if a focus was likely as shown by radiologic examination.
Platelet concentrates
PCs were prepared from 5 pooled whole-blood BCs with the same ABO blood group.22,23 After collection of a unit of whole blood, BCs were prepared through high-speed centrifugation. Five BCs together with 1 unit of PAS II or 1 unit plasma from one of the BC donors were coupled to a BC pool set (containing a transfer bag, leukocyte filter, and a PL-2410 storage container; Baxter) through a sterile connection device. After connecting, the 5 BCs were pooled in the transfer bag together with the unit of PAS II or plasma. A low-speed differential centrifugation was used to separate the platelet-rich supernatant from erythrocytes and leukocytes, which subsequently was pressed through the leukocyte filter into the storage container. A sample was obtained prior to storage to measure platelet content, pH, and bacterial culture. The platelet content was measured using a Beckman Coulter Act-10 (Beckman Coulter, Miami, FL). The PCs were stored at 20°C to 24°C on a flatbed shaker up to 5 days. The PCs were γ irradiated with 25 Gy at the time of issue in case of specific patient requirements for the prevention of transfusion-associated graft-versus-host disease.
Platelet transfusions and monitoring
The treating physician ordered platelet transfusions according to local hospital guidelines. In general, indications were prophylactic trigger-based transfusions, prophylaxis prior to an intervention, or treatment of bleeding complications. The transfusion trigger for uncomplicated prophylaxis was up to 10 × 109/L. In case of serious infections, anticoagulant medication, or administration of anti–thymocyte globulin (ATG), a trigger of up to 30 × 109/L was used. In case of surgical interventions or bleeding complications, a platelet trigger of 50 × 109/L or above was used. Pretransfusion platelet count was measured 1 hour prior to transfusion. Platelet counts were measured from 10 minutes to 2 hours after transfusion and from 16 to 24 hours after transfusion to determine the 1- and 24-hour increment, respectively. Platelet counts in the participating hospitals were measured using a Sysmex XE-2100 (Sysmex, Kobe, Japan). In case of a second PC transfusion within 4 hours, both transfusions were considered to be part of one transfusion. If the 24-hour increment exceeded the 1-hour increment, combined with other signs of hematopoietic recovery, the 24-hour increment value was excluded from analysis. PC transfusion failure was defined as a 1-hour CCI below 7.5 and/or a 24-hour CCI below 4.5. Patients experiencing repeated episodes (2 or more subsequent PC transfusions) of PC transfusion failure without an apparent nonimmunologic cause were tested for the existence of HLA and/or HPA antibodies. If available, PCs of ABO-identical donors were used, although both minor ABO-incompatible (ie, potential donor anti-A and/or anti-B antibodies directed to the platelets/red cells of the patient) and major ABO-incompatible (ie, potential patient anti-A and/or anti-B antibodies directed to the donor platelets) PCs were not excluded.
Study end points
The primary end points of the study protocol were the 1- and 24-hour CCIs, calculated as follows: CCI1/24 h = [(posttransfusion count (× 109/L)1/24 h – pretransfusion count (× 109/L)) × body surface area (m2)]/platelet dose (× 1011). Secondary end points were transfusion interval, transfusion-related adverse reactions, and bleeding complications. The transfusion interval was defined as the calculated administrative time of 2 consecutive PC transfusions.
Statistical methods
The study was designed as a 2-arm noninferiority study. The sample size calculation was based on data of patients enrolled in the 2 randomized trials concerning nonplasma storage media.12,13 The standard deviation of the mean 1- and 24-hour CCIs was estimated as 6.0. To detect a difference of 30% between the 1- and 24-hour CCIs of PAS II PCs and plasma PCs using a .05 level 2-sided test, a sample size of 360 transfusions in each study arm provided a power of 90%. The statistical comparison of the CCIs of the 2 products was performed both as independent transfusion events as well as in a mixed linear model, assuming biologic interdependence of consecutive PC transfusions in a patient (SPSS/PC+; SPSS, Chicago, IL). Fisher exact tests were used to compare patient characteristics. A multivariate analysis testing the effects on both count increments and CCIs as well as the occurrence of transfusion failure was performed, including storage time, storage medium, sex, age, body weight, body surface area, diagnosis, therapy, history of prior platelet transfusions, fever (body temperature more than 38°C) at the time of transfusion, infection, splenomegaly, and ATG, using a random effects logistic regression model (EGRET).
Results
Patient population
Between October 2003 and April 2005, 195 patients were randomized (plasma PC, n = 95; PAS II PC, n = 100). A total of 11 patients were excluded (plasma PC, n = 7; PAS II PC, n = 4) of which 6 patients had HLA alloantibodies and 1 patient had HPA alloantibodies prior to the first transfusion, 1 patient developed refractoriness with proven HLA alloantibodies after the second transfusion, 2 patients acquired an indication for CMV-negative blood products, and 1 patient was transferred to another department. Although patients were randomized based on expected platelet transfusions, 16 patients did not receive any platelet transfusion during the inclusion period (plasma PC, n = 4; PAS II PC, n = 12), resulting in 168 patients in which platelet transfusions could be evaluated (plasma PC, n = 84; PAS II PC, n = 84). There were no significant differences between the 2 study arms (ie, patients with evaluable transfusions) regarding demographic characteristics, diagnosis, treatment, and transfusion history (Table 1). The same applied for the excluded, nontransfused patients in both groups. Splenomegaly was present in 17 patients (10.1%). The mean time on study for patients receiving PAS II PCs and plasma PCs was 20.7 ± 7.1 and 21.5 ± 8.6 days (P = 0.54), respectively. Twenty-one patients were randomized more than once (plasma PC, n = 11; PAS II PC, n = 10). There were no significant differences in the occurrence of febrile episodes, proven infections, and mucosal damage, most often localized to the digestive system (painful oral lesions and diarrhea).
Patient characteristics
. | Plasma PC . | PAS II PC . | P . |
|---|---|---|---|
| No. of patients | 84 | 84 | — |
| Male/female | 53/31 | 56/28 | .85 |
| Age, y ± SD | 51.4 ± 13.1 | 50.1 ± 14.6 | .54 |
| Body surface area, m2 ± SD | 1.94 ± 0.22 | 1.92 ± 0.24 | .57 |
| Enlarged spleen (%) | 6 (7.1) | 11 (13.1) | .31 |
| Diagnosis | |||
| AML/MDS (%) | 43 (51) | 44 (52) | .999 |
| ALL (%) | 7 (8.3) | 5 (5.9) | .77 |
| CML (%) | 5 (5.9) | 3 (3.6) | .72 |
| CLL (%) | 1 (1.2) | 3 (3.6) | .62 |
| Myeloma (%) | 14 (17) | 6 (7.1) | .09 |
| NHL (%) | 13 (15) | 21 (25) | .18 |
| Other (%) | 1 (1.2) | 2 (2.4) | .999 |
| Therapy | |||
| Remission induction (%) | 31 (37) | 31 (37) | 1.13 |
| Consolidation (%) | 9 (11) | 12 (14) | .64 |
| Allogenic transplantation (%) | 18 (21) | 20 (24) | .58 |
| Autologous transplantation (%) | 23 (27) | 19 (23) | .59 |
| TBI (%) | 17 (20) | 14 (17) | .69 |
| ATG (%) | 5 (5.9) | 7 (8.3) | .77 |
| Other (%) | 3 (3.6) | 2 (2.4) | .999 |
| Transfusion history | |||
| RBC concentrates (%) | 66 (79) | 62 (74) | .59 |
| PCs (%) | 58 (69) | 52 (62) | .42 |
| Transplantations (%) | 10 (12) | 5 (5.9) | .28 |
. | Plasma PC . | PAS II PC . | P . |
|---|---|---|---|
| No. of patients | 84 | 84 | — |
| Male/female | 53/31 | 56/28 | .85 |
| Age, y ± SD | 51.4 ± 13.1 | 50.1 ± 14.6 | .54 |
| Body surface area, m2 ± SD | 1.94 ± 0.22 | 1.92 ± 0.24 | .57 |
| Enlarged spleen (%) | 6 (7.1) | 11 (13.1) | .31 |
| Diagnosis | |||
| AML/MDS (%) | 43 (51) | 44 (52) | .999 |
| ALL (%) | 7 (8.3) | 5 (5.9) | .77 |
| CML (%) | 5 (5.9) | 3 (3.6) | .72 |
| CLL (%) | 1 (1.2) | 3 (3.6) | .62 |
| Myeloma (%) | 14 (17) | 6 (7.1) | .09 |
| NHL (%) | 13 (15) | 21 (25) | .18 |
| Other (%) | 1 (1.2) | 2 (2.4) | .999 |
| Therapy | |||
| Remission induction (%) | 31 (37) | 31 (37) | 1.13 |
| Consolidation (%) | 9 (11) | 12 (14) | .64 |
| Allogenic transplantation (%) | 18 (21) | 20 (24) | .58 |
| Autologous transplantation (%) | 23 (27) | 19 (23) | .59 |
| TBI (%) | 17 (20) | 14 (17) | .69 |
| ATG (%) | 5 (5.9) | 7 (8.3) | .77 |
| Other (%) | 3 (3.6) | 2 (2.4) | .999 |
| Transfusion history | |||
| RBC concentrates (%) | 66 (79) | 62 (74) | .59 |
| PCs (%) | 58 (69) | 52 (62) | .42 |
| Transplantations (%) | 10 (12) | 5 (5.9) | .28 |
Percentages represent percentages of patients in the study arm.
AML/MDS indicates acute myeloid leukemia/myelodysplastic syndrome; ALL, acute lymphoid leukemia; CML, chronic myeloid leukemia; CLL, chronic lymphoid leukemia; NHL, non-Hodgkin lymphoma; TBI, total body irradiation; —, not applicable; and RBC, red blood cell.
Platelet transfusions: product parameters and increments
A total of 765 PCs were transfused (plasma PC, n = 354; PAS II PC, n = 411). A total of 684 PC transfusions could be evaluated (89%; plasma PC, n = 311; PAS II PC, n = 373). In the PAS II PC group, the 1-hour and 24-hour CCIs could be calculated in 337 (90%) and 334 (90%) transfusions, respectively. In the plasma PC group this was the case in 274 (88%) and 282 (91%) transfusions. The missing CCIs were a result of missing precount and 1- and/or 24-hour postcount data.
In Table 2, product parameters, dosage, count increments, and CCIs are shown. Although the mean platelet content of PAS II PCs was significantly lower than that of plasma PCs, there was no significant difference in the mean dose per kilogram of body weight per transfusion between the 2 groups. There was a significant difference regarding the pH. However, all products had a pH well above 6.8. Univariate analysis, assuming each platelet transfusion as an independent event, showed a mean difference in 1-hour and 24-hour CCIs between plasma PCs and PAS II PCs of 19.7% (95% confidence interval [CI], 11.7% to 27.2%; P < .001) and 17.8% (95% CI, 5.9% to 31%; P = .004), respectively. We also analyzed the CCIs in a mixed linear model for biologic interdependence of consecutive PC transfusions (Table 2). This analysis resulted in the same mean difference in 1-hour and 24-hour CCIs between plasma PCs and PAS II PCs, but confidence intervals and P values differed. With respect to the difference in 1-hour CCI the analysis showed a 95% CI between 6.5% and 32.9% (P = .004), and the difference in 24-hour CCI resulted in a 95% CI between – 2.4% and 38.1% (P = .09). A multivariate analysis as described in “Patients, materials, and methods” showed an independent effect of the used storage medium with regard to both count increments and CCIs. Plasma PCs and PAS II PCs resulted in a sufficient 1-hour CCI in 81.3% and 69.1%, respectively (P < .001). The 24-hour CCI was sufficient in 70.7% and 65.7% (P = 0.16). Considering the difference in platelet content of plasma PCs and PAS II PCs, we also performed a linear regression analysis of count increments and platelet dose confirming significant lower 1- and 24-hour count increments after transfusion of PAS II PCs (data not shown). Gamma irradiation had no significant effect on the transfusion responses of both PCs.
Platelet product parameters, dosage, and transfusion response
. | Plasma PC . | PAS II PC . | P . |
|---|---|---|---|
| No. of transfusions | 311 | 373 | — |
| No. of platelets/product, × 109 ± SD | 412 ± 93 | 391 ± 119 | .01 |
| Storage time, d ± SD | 3.5 ± 1.3 | 3.5 ± 1.1 | n.s. |
| pH ± SD | 7.12 ± 0.04 | 7.08 ± 0.04 | < .001 |
| Product volume, mL ± SD | 356 ± 19 | 316 ± 11 | < .001 |
| Precount, × 109/L ± SD | 13.3 ± 8.7 | 13.7 ± 10.5 | n.s |
| Platelet dose per kg body weight,* × 109/L ± SD | 5.5 ± 1.7 | 5.3 ± 2.0 | n.s. |
| Transfusion response† | |||
| No. of 1-h transfusions | 274 | 337 | — |
| CI ± SD | 32.2 ± 17.1 | 24.6 ± 14.8 | .001 |
| CCI ± SD | 13.9 ± 7.0 | 11.2 ± 6.4 | .004 |
| No. of 24-h transfusions | 282 | 334 | — |
| CI ± SD | 20.6 ± 16.0 | 16.3 ± 14.1 | .028 |
| CCI ± SD | 8.4 ± 6.9 | 6.8 ± 6.4 | .09 |
. | Plasma PC . | PAS II PC . | P . |
|---|---|---|---|
| No. of transfusions | 311 | 373 | — |
| No. of platelets/product, × 109 ± SD | 412 ± 93 | 391 ± 119 | .01 |
| Storage time, d ± SD | 3.5 ± 1.3 | 3.5 ± 1.1 | n.s. |
| pH ± SD | 7.12 ± 0.04 | 7.08 ± 0.04 | < .001 |
| Product volume, mL ± SD | 356 ± 19 | 316 ± 11 | < .001 |
| Precount, × 109/L ± SD | 13.3 ± 8.7 | 13.7 ± 10.5 | n.s |
| Platelet dose per kg body weight,* × 109/L ± SD | 5.5 ± 1.7 | 5.3 ± 2.0 | n.s. |
| Transfusion response† | |||
| No. of 1-h transfusions | 274 | 337 | — |
| CI ± SD | 32.2 ± 17.1 | 24.6 ± 14.8 | .001 |
| CCI ± SD | 13.9 ± 7.0 | 11.2 ± 6.4 | .004 |
| No. of 24-h transfusions | 282 | 334 | — |
| CI ± SD | 20.6 ± 16.0 | 16.3 ± 14.1 | .028 |
| CCI ± SD | 8.4 ± 6.9 | 6.8 ± 6.4 | .09 |
n.s. indicates nonsignificant; —, not applicable.
Per transfusion.
General linear mixed model accounting for within-patient correlation of observations (repeated measurements).
Bleeding complications, transfusion reactions, and transfusion interval
The overall incidence of bleeding complications was 32.1%, consisting of 16.1% grade I, 14.3% grade II, and 1.8% grade III. Grade IV bleeding was not observed. There were no differences between the 2 study groups. As a surrogate marker for bleeding, we also calculated the mean transfused red-cell concentrates per patient; no difference was observed.
A total of 26 mild transfusion reactions were observed in 21 patients. Of these, 17 (5.5%) transfusion reactions were related to plasma PCs and 9 (2.4%) to PAS II PCs (P = .04). Eight patients receiving PAS II PCs experienced transfusion reactions versus 13 receiving plasma PCs (P = .35). One patient, receiving plasma PCs and having complications of repeated dyspnea and wheezing, decided to end the study protocol and was further treated with plasma-reduced hyperconcentrated platelet products.
Table 3 shows an overview of platelet and red-cell transfusions and the calculated transfusion interval. There were no significant differences with regard to transfused PCs, interval, and required red-cell transfusions per patient. However, the platelet transfusion interval is substantially determined by timing of blood sampling and varying (logistic) delays in PC administration after reaching a transfusion trigger.
Platelet transfusions, red-cell transfusions, and transfusion interval
. | Plasma PC . | PAS II PC . | P . |
|---|---|---|---|
| No. of patients | 84 | 84 | — |
| No. of RBC transfusions | 452 | 475 | — |
| Mean RBC transfusions per patient ± SD | 4.8 ± 4.1 | 5.1 ± 3.8 | .62 |
| No. of PC transfusions | 354 | 411 | — |
| PC transfusion interval, d ± SD | 2.0 ± 1.0 | 2.1 ± 1.0 | .52 |
| Mean PC transfusions per patient ± SD | 4.2 ± 2.7 | 4.9 ± 2.8 | .10 |
| Cumulative platelet dose per kg, × 1011/kg ± SD | 0.22 ± 0.15 | 0.23 ± 0.16 | .68 |
. | Plasma PC . | PAS II PC . | P . |
|---|---|---|---|
| No. of patients | 84 | 84 | — |
| No. of RBC transfusions | 452 | 475 | — |
| Mean RBC transfusions per patient ± SD | 4.8 ± 4.1 | 5.1 ± 3.8 | .62 |
| No. of PC transfusions | 354 | 411 | — |
| PC transfusion interval, d ± SD | 2.0 ± 1.0 | 2.1 ± 1.0 | .52 |
| Mean PC transfusions per patient ± SD | 4.2 ± 2.7 | 4.9 ± 2.8 | .10 |
| Cumulative platelet dose per kg, × 1011/kg ± SD | 0.22 ± 0.15 | 0.23 ± 0.16 | .68 |
— indicates not applicable.
Effects of storage
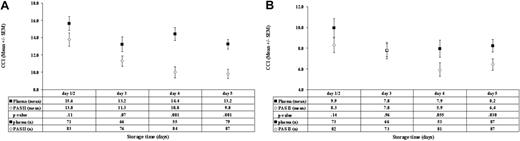
Storage time had a significant effect on the transfusion response of both PCs (Figure 1). Stored PAS II PCs as well as stored plasma PCs showed a decrease in 1-hour CCI compared with fresh PCs. For both PCs this difference became significant after 2 days of storage. Stored plasma PCs show a gradual decrease in 24-hour CCI; however, no significance is reached compared with fresh PCs. The same is true for PAS II PCs, although after 4 days of storage the deterioration was significant (P = .02), showing that the effects of storage time were more pronounced in PAS II PCs.
Comparison of 1- and 24-hour CCIs. Both panels show the comparison of 1- and 24-hour CCIs, respectively, related to storage time of plasma PCs and PAS II PCs. Both PCs show a significant decrease in 1- and 24-hour CCIs during storage. (A) A significant difference between plasma PCs and PAS II PCs after 3 days of storage is shown. (B) A significant difference between the 2 products after 5 days of storage is shown. SEM indicates standard error of the mean; n, number of transfusions.
Comparison of 1- and 24-hour CCIs. Both panels show the comparison of 1- and 24-hour CCIs, respectively, related to storage time of plasma PCs and PAS II PCs. Both PCs show a significant decrease in 1- and 24-hour CCIs during storage. (A) A significant difference between plasma PCs and PAS II PCs after 3 days of storage is shown. (B) A significant difference between the 2 products after 5 days of storage is shown. SEM indicates standard error of the mean; n, number of transfusions.
Effect factors of increased platelet consumption
Refractoriness, both immunologic as well as nonimmunologic, remains an important clinical problem. In our study, 34.5% of patients experienced 1 or more transfusions with a 1-hour CCI below 7.5, while 25% of all transfusions resulted in a 1-hour CCI below 7.5. Of all transfusions 25 were major ABO incompatible (plasma PC, n = 12; PAS II PC, n = 13), mostly patients with blood group O receiving a blood group A product. A 1-hour transfusion failure after 2 or more subsequent transfusions occurred in 34 patients (plasma PC, n = 14; PAS II PC, n = 20), in 7 patients (plasma PC, n = 4; PAS II PC, n = 3) not explained by obvious nonimmunologic factors. Testing these patients revealed only 1 patient with HLA antibodies and none with HPA antibodies. Two patients, without detectable HLA antibodies, received an HLA-matched test transfusion, both without success.
A number of nonimmunologic factors have been associated with an increase in platelet consumption. Most patients with hematologic malignancies experience complex clinical conditions, and in our study only 25% of the transfusions were administered in the absence of factors known to increase platelet consumption. A multivariate analysis to evaluate transfusion efficacy in terms of 1- and 24-hour transfusion failure is shown in Table 4. Factors independently influencing 1-hour transfusion failure were splenomegaly, ATG, fever, and infection. Storage time showed a trend toward an effect, but the used storage medium did not significantly influence the occurrence of 1-hour transfusion failure. The 24-hour transfusion failure was determined by splenomegaly, ATG, and fever, and the age of the patient significantly contributed to the occurrence of 24-hour transfusion failure, whereas both storage time and used medium disappeared as independent factors.
Multivariate analysis*of 1- and 24-hour transfusion failure
. | Odds ratio, 1-h CCI less than 7.5 (95% CI) . | P . | Odds ratio, 24-h CCI less than 4.5 (95% CI) . | P . |
|---|---|---|---|---|
| Storage time | 1.93 (0.95-3.93) | .069 | 1.51 (0.82-2.79) | .18 |
| Storage medium | 0.60 (0.25-1.42) | .25 | 0.72 (0.30-1.69) | .46 |
| Fever | 1.41 (0.97-2.04) | .071 | 1.88 (1.33-2.66) | < .001‡ |
| Infection | 0.38 (0.17-0.84) | .02‡ | 1.08 (0.57-2.05) | .999 |
| Enlarged spleen | 26.7 (8.13-87.7) | < .001‡ | 7.55 (2.35-24.2) | < .001‡ |
| ATG | 39.6 (7.81-201) | < .001‡ | 4.83 (1.14-20.5) | .03‡ |
| Age | 1.01 (0.98-1.04) | .47 | 1.04 (1.01-1.07) | .023†‡ |
| Sex | 0.59 (0.18-1.93) | .39 | 0.71 (0.21-2.42) | .58 |
| Diagnosis | 0.71 (0.71-1.31) | .96 | 1.09 (0.82-1.43) | .56 |
| Therapy | 1.16 (0.85-1.58) | .36 | 1.06 (0.79-1.44) | .68 |
| Transfusion history | 1.10 (0.41-2.90) | .85 | 0.68 (0.46-3.35) | .68 |
| Body weight | 0.97 (0.86-1.11) | .69 | 0.90 (0.79-1.04) | .999 |
. | Odds ratio, 1-h CCI less than 7.5 (95% CI) . | P . | Odds ratio, 24-h CCI less than 4.5 (95% CI) . | P . |
|---|---|---|---|---|
| Storage time | 1.93 (0.95-3.93) | .069 | 1.51 (0.82-2.79) | .18 |
| Storage medium | 0.60 (0.25-1.42) | .25 | 0.72 (0.30-1.69) | .46 |
| Fever | 1.41 (0.97-2.04) | .071 | 1.88 (1.33-2.66) | < .001‡ |
| Infection | 0.38 (0.17-0.84) | .02‡ | 1.08 (0.57-2.05) | .999 |
| Enlarged spleen | 26.7 (8.13-87.7) | < .001‡ | 7.55 (2.35-24.2) | < .001‡ |
| ATG | 39.6 (7.81-201) | < .001‡ | 4.83 (1.14-20.5) | .03‡ |
| Age | 1.01 (0.98-1.04) | .47 | 1.04 (1.01-1.07) | .023†‡ |
| Sex | 0.59 (0.18-1.93) | .39 | 0.71 (0.21-2.42) | .58 |
| Diagnosis | 0.71 (0.71-1.31) | .96 | 1.09 (0.82-1.43) | .56 |
| Therapy | 1.16 (0.85-1.58) | .36 | 1.06 (0.79-1.44) | .68 |
| Transfusion history | 1.10 (0.41-2.90) | .85 | 0.68 (0.46-3.35) | .68 |
| Body weight | 0.97 (0.86-1.11) | .69 | 0.90 (0.79-1.04) | .999 |
Random effects binary logistic model for distinguishable data (odds ratios and P values are corrected for within-patient correlation of observations).
Increasing age had a minor unfavorable effect on transfusion failure.
Values are significant.
Discussion
With the intention to harmonize platelet products in the Netherlands and in anticipation of future product changes, we performed a randomized controlled trial comparing plasma PCs with PAS II PCs. With the exception of immunologic refractoriness due to HLA and HPA antibodies, no exclusion criteria regarding factors of increased platelet consumption were used. There is general agreement that changes in platelet products should be validated for their clinical quality. Because major bleeding complications are rare, platelet count increments and CCIs have been accepted as surrogate end points.24 A draft guidance for testing and evaluating platelet components advises an array of in vitro tests, the use of in vivo autologous radiolabeled platelet survival studies, and clinical trials, including hemostatic efficacy.25 Currently, in Europe the requirements defined for quality control of platelet transfusion are minimal. In our study swirl, pH and platelet content were determined as in vitro parameters. Swirl was present in all transfused products. The platelet content of the products was measured directly after production, because a previous study has shown a limited decline in platelet number during 5 days of storage.4,23 We found significant differences with regard to pH and platelet content of the 2 PCs. The lower pH of PAS II PCs is due to a lower intrinsic pH of PAS II, lower buffering capacity, and higher lactate production.23 The lower platelet content of PAS II PCs can be explained by a viscosity-related difference in the platelet distribution during centrifugation, resulting in a less efficient separation.23
We showed that the 1- and 24-hour CCIs of PAS II PCs were lower compared with plasma PCs, with a mean difference of 19.7% and 17.8%, respectively. This effect remained after correcting for possible confounders in a multivariate analysis. Although the platelet content in PAS II PCs was significantly (approximately 5%) lower compared with plasma PCs, this small difference is not clinically relevant and the transfused dose per kilogram (or per square meter) in both groups was similar. Univariate analysis of the effect of storage time showed a significant decrease in 1-hour and 24-hour CCIs in both products (more pronounced in stored PAS II PCs) in contrast with the results of the study of de Wildt-Eggen et al.12 The mechanism of this storage effect is unknown. Increased P-selectin expression and structural changes have been suggested as possible mechanisms.5,6 Whether such in vitro changes explain the inferior increments of PAS II PCs remains unclear.8,9
To investigate the clinical relevance of the inferior CCI of PAS II PCs, we compared the incidence of bleeding, transfusion interval, red-cell concentrate usage, and the occurrence of transfusion failure, the latter also in relation to patient factors. We did not observe significant differences with regard to bleeding complications or the consumption of PCs and red-cell concentrates. Univariate analysis of transfusion failures showed a significant effect of PAS II PCs on the occurrence of 1-hour transfusion failure but not on the 24-hour transfusion failure. A multivariate analysis showed that patient-related factors overruled product-defined factors as determinants of transfusion failure at 1 and 24 hours, with the exception of storage time, which showed a trend toward 1-hour transfusion failure. The only other randomized study, conducted by de Wildt-Eggen et al,12 used a different transfusion threshold (more than 20 × 109/L) and excluded sick patients. It is likely that the differences in CCIs and transfusion failure between the 2 studies are caused by factors of increased platelet consumption in our study population, because several studies demonstrated the impact of patient factors on the occurrence of transfusion failure.15-19 In our study, more than 75% of all PCs were transfused during episodes with clinical complications associated with increased platelet consumption, and multivariate analysis showed that patient-related factors annihilated the effects of the used storage medium in relation to transfusion failure.
Compared with other studies we found a relatively low percentage of transfusion reactions, although significantly less after transfusions with PAS II PCs (P = .04), confirming the results of de Wildt-Eggen et al.12 Probably this percentage underestimates the real frequency due to the fact that most reactions are mild, whereas fever and chills are common symptoms in this category of patients.
In conclusion, we showed that transfusion responses with PAS II PCs are significantly lower, but not inferior, as compared with plasma PCs. The biologic significance of this observation does not significantly exceed a 30% deterioration. A multivariate analysis showed that patient-related factors annihilated the observed differences, and there were no significant differences with regard to bleeding complications or PC consumption. Transfusion reactions were mild, infrequent, and significantly lower with PAS II PCs. Because most patients in need of supportive care temporarily experience factors leading to increased platelet consumption, we propose that future clinical trials studying experimental platelet products should include these patients. We showed safety and efficacy of PAS II PCs in intensively treated patients; however, plasma PCs show superior increments. To prevent a downward creep in platelet products developed in the future, we advise that storage of platelets in plasma should be included as a reference in future trials.
Prepublished online as Blood First Edition Paper, July 6, 2006; DOI 10.1182/blood-2006-04-020131.
J.-L.H.K. was the primary investigator and wrote the article; J.C.E. provided scientific support and was a local investigator at Leiden University Medical Centre; M.S.S. was a local investigator at HagaZiekenhuis; R.J.v.W.-V. was the data manager; R.B. was the statistician; M.S.H. provided scientific support and study design; R.R.d.V. provided scientific support and supervised the local blood bank; R.B. provided scientific support and supervised the department of hematology; D.J.v.R. was a scientific supervisor and supervised the regional blood bank; and A.B. was a scientific supervisor and designed the study.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors acknowledge all laboratory personnel, physicians, and nursing staff of the hematology departments of the Leiden University Centre, the HagaZiekenhuis in The Hague, and Sanquin Blood Bank South West Region, without whose efforts this study could not have been completed.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal