In a recent article, Elliott et al1 question the specificity of commercially available antibodies against the erythropoietin receptor (EpoR) and thus the validity of an increasing number of studies showing expression of functional EpoR in many nonhematopoietic tissues including most solid cancers.2-6
It is well known that antibody qualities are quite variable. The effort of Elliott et al1 to thoroughly test the available EpoR antibodies should therefore be appreciated, because the authors could eventually have contributed to this field of research. However, a closer look at their study reveals severe methodological issues. First, Elliott et al1 used an expression construct for EpoR that has not been verified in this study. Unfortunately, the detected band was not subjected to liquid chromatography coupled to mass spectrometry (LC-MS), functional integrity of the expressed protein was not demonstrated, and it is therefore unclear if the expression plasmid codes for a functional human EpoR. Second, EpoR undergoes posttranslational modification and functional EpoR has a size between 66 and 78 kDa. A soluble form of EpoR and a truncated form of this receptor can be detected at lower molecular weight. The 59-kDa band detected by Elliott et al1 is most likely physiologically irrelevant and raises the question why proteins derived from their expression plasmid are not processed into active receptors. Third, after ligand binding, EpoR is internalized and degraded. The cancer lines used by Elliott et al1 show varying levels of EpoR surface levels under standard culture conditions. EpoR is usually detectable only after serum starvation, and lack of EpoR expression in these cells under the conditions chosen is no surprise to anyone in this research field. In addition, the C20 antibody was used at 1.32 μg/mL, whereas the manufacturer recommends 0.1 to 1.0 μg/mL. Culture conditions, which lead to receptor internalization and degradation combined with antibody concentrations favoring unspecific binding, are inappropriate to investigate the specificity of any antibody. Fourth, mass spectrometry of trypsin-digested bands cut out of Western blots usually gives rise to many possible protein identities (IDs). HSPs bind to cytokine receptors and identification of a chaperon like HSP70 may indicate incomplete denaturizing conditions. A state-of-the-art approach would have employed 2D electrophoresis instead. In the study of Elliott et al1 it would have been mandatory to report probability scores for the proteins identified and we would have appreciated if the authors would have provided this data as supplementary material. Without this information, the validity of the LC-MS analysis is questionable and the results do not allow any conclusion to be drawn. Finally, the M-20 antibody is not recommended for use in immune histochemistry (IHC) by the manufacturer. Thus, immunohistochemical data provided by Elliott et al1 confirm the product data sheet of the M20 antibody but do not add to the knowledge on EpoR.
With the exception of solid cancer cells, the cytoprotective effect of recombinant human Epo (rhEpo) in many tissues is a widely accepted concept in the scientific community and in the pharmaceutical industry.7,8 Furthermore, an increasing number of studies show not only expression of EpoR mRNA and protein in solid cancers but also rhEpo-dependent signaling in cancer cells.9-11 Two recent clinical trials support tumor protection by rhEpo.12,13 By questioning the validity of past studies of EpoR expression in solid tumors, Elliott et al1 attempt to support the general safety of rhEpo in the treatment of cancer anemia. Unfortunately, their conclusions are not supported by the data presented and indicate methodological issues rather than novel findings.
Anti-EpoR antibodies detect a 59-kDa EpoR protein
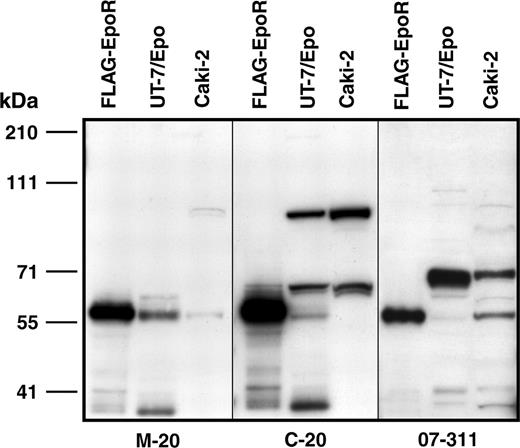
Henke and colleagues claim there are methodological problems with our study demonstrating that the 66-kDa protein detected by the C-20 antibody (Santa Cruz Biotechnology, Santa Cruz, CA) is not EpoR.1 We disagree with their critique of our study for 4 reasons. (1) They suggest we did not demonstrate functional expression of human EpoR encoded by our expression construct (FLAG-EpoR). However, BaF3 cells expressing FLAG-EpoR showed Epo-dependent growth, demonstrating functional expression (Janet Cheng [Amgen, Thousand Oaks, CA]; unpublished data, 2005). (2) The authors state that functional EpoR has a molecular weight of 66 to 78 kDa because of posttranslational modification. However, that statement is incorrect on theoretical grounds and is likely based on studies that used the anti-EpoR antibodies in question. The correct size is likely approximately 59 kDa. The calculated size of EpoR protein is 52.6 kDa, and the single N-linked glycosylation site would add only 3 to 4 kDa, resulting in sizes of glycosylated EpoR and FLAG-EpoR of 56 to 57 and 57 to 58 kDa, respectively (FLAG adds 1 kDa). In the Epo-responsive cell line UT-7/Epo, C-20 detected and immunoprecipitated a 59-kDa protein (Figure S2 in Elliott et al),1 EpoR sequences were found at 59 kDa in preparative gels, 59kDa levels decreased following EpoR shRNA treatment (Figure S1 in Elliott et al),1 and, although 3 different anti-EpoR antibodies detected a 59-kDa protein, they each detected larger proteins of various sizes (Figure 1). (3) Since no commercially available antibodies are suitable for detection of surface EpoR, we did not investigate surface EpoR in cancer cell lines; we reported total cellular levels. We are unaware of validated reports directly showing up-regulation of EpoR in response to serum starvation. The concentration of C-20 used in our study was 0.132 μg/mL and not 1.32 μg/mL (stated in error in our initial report). (4) We performed mass spectrometry on proteolyzed proteins isolated from preparative gels of cell extracts immunoprecipitated with C-20. The sequence analysis was rigorous. Sequence search (SEQUEST; Thermo Finnigan, San Jose, CA) was rigorous, with probability scores of cross-correlation value (XCorr) = 2.0 and delta correlation value (DelCn) = 0.12,2 which were used to filter false positives, and manual validation was performed on questionable spectra. More than 35% of all unique peptides (55 of 153) identified in the 66-kDa band were derived from various regions of heat-shock proteins (HSPs), and none were derived from EpoR. Specific inhibition of C-20 binding to the 66-kDa protein by an HSP70 peptide was demonstrated (Figure 1 in Elliott et al).1 An EpoR peptide identified in the 59-kDa band had a high probability score of 2.6 (XCorr) and 0.23 (DelCn) and its corresponding spectra was manually validated. These analyses show that the 66-kDa band detected by C-20 is an HSP and that the 59-kDa band is EpoR.
Detection of proteins with anti-EpoR antibodies. M-20, C-20, and 07-311 all detected 59-kDa proteins. C-20 detected a 66-kDa protein, whereas 07-311 detected an approximately 70-kDa protein. Protein extracts were prepared from COS-7 cells expressing FLAG-EpoR, UT-7/Epo cells (50 000 cells/lane), and Caki-2 cells (60 000 cells/lane). Proteins were resolved on a 7% gel and subjected to Western immunoblotting using the antibodies C-20 (0.132 ug/mL), 07-311 (0.1 μg/mL), or M-20 (0.2 μg/mL), as described previously.1 Positions of the molecular weight markers are illustrated on the left (kDa).
Detection of proteins with anti-EpoR antibodies. M-20, C-20, and 07-311 all detected 59-kDa proteins. C-20 detected a 66-kDa protein, whereas 07-311 detected an approximately 70-kDa protein. Protein extracts were prepared from COS-7 cells expressing FLAG-EpoR, UT-7/Epo cells (50 000 cells/lane), and Caki-2 cells (60 000 cells/lane). Proteins were resolved on a 7% gel and subjected to Western immunoblotting using the antibodies C-20 (0.132 ug/mL), 07-311 (0.1 μg/mL), or M-20 (0.2 μg/mL), as described previously.1 Positions of the molecular weight markers are illustrated on the left (kDa).
The role of EpoR in tumor growth is highly contentious and, in contrast to the suggestion by Henke and colleagues, has not been conclusively demonstrated. The authors support their contention that erythropoietic-stimulating agents (ESAs) promote tumor growth by citing 2 clinical trials that used ESAs, outside of the prescribing guidelines, to prevent anemia in cancer patients.3,4 However, these studies have been criticized for poor study design and execution.5-8 A number of ongoing trials will determine the impact on survival of patients undergoing therapy with ESAs.
The authors are employed by Amgen Inc, a manufacturer and distributor of erythropoietic-stimulating proteins.
Correspondence: Steve Elliott, Amgen Inc, One Amgen Center Drive, Thousand Oaks, CA 91320; e-mail: selliott@amgen.com.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal