Abstract
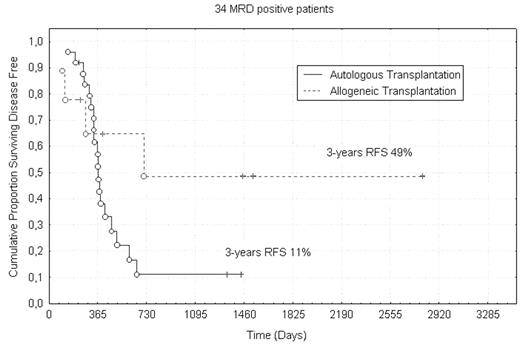
Autologous (AuSCT) and allogeneic stem cell transplantation (SCT) are well established post-remissional strategies for patients with Acute Myeloid Leukemia (AML). However, there is still a debate ongoing about the relative merit of each of these options in first CR. Minimal residual disease (MRD) may be a useful tool to stratify AML patients into categories of risk which can benefit from differentiated post-remissional approaches. To address this issue, we analysed retrospectively, a series of 123 patients affected with AML in whom flow-cytometry serial determinations of MRD were available, at established time-points (post-induction, post-consolidation, post-stem cell transplantation). All were entered into the EORTC/GIMEMA protocols AML10/AML12 (age <61 yrs) or AML13 (age>61 yrs), all consisting in intensive induction and consolidation cycles, and, for patients aged <61 years, AuSCT or SCT. Median age was 52 years (range 18–78), no APL cases were included in the study. The “Maximally Selected Rank Statistic” analysis was used to select the MRD level and the time-point of analysis achieving the best prognostic significance in terms of overall survival (OS) and relapse free survival (RFS). This test was specifically developed to find out the optimal cut-off for a given biological variable correlating with clinical parameters of interest. This approach confirmed the threshold of 3.5x10−4 residual leukemic cells after consolidation therapy, as a discriminator between MRD− and MRD+ cases with different 5-years OS (64% vs. 14%, P<.001) and RFS (68% vs. 13%, P<.001). Therefore, among these 123 patients, we enucleated 2 groups of patients which underwent stem cell transplant procedure, 53 AuSCT and 11 SCT. The two subgroups were balanced in terms of FAB categories, WBC count, karyotype and expression of MDR-1 phenotype; 34/64 (53%) were MRD+ (9 SCT, 25 AuSCT) and 30/64 (47%) were MRD− (1 SCT, 28 AuSCT). Among the 53 patients submitted to AuSCT, MRD− had a significant better outcome than those MRD+, both in terms of 5-years OS (68% vs. 24%, P=0.003) and RFS (68% vs. 11%, P<.001). In the SCT group the low numbers hampered any firm conclusion; however, when the category of post-consolidation MRD+ patients was separately analysed, the use of SCT was associated with a better RFS (49% vs. 11%, P=NS); we assume that the lack of statistical significance was merely due to the few cases in the SCT group. In conclusion,
the threshold of 3.5x10−4 at post-consolidation check-point is critical to predict disease outcome;
MRD− patients have an excellent outcome regardless of the post-consolidation therapy;
in the MRD+ group, AuSCT seems not to improve the prognosis whereas the use of SCT is associated with a superior outcome, although a larger number of patients is required to confirm this assumption.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal