Abstract
The characteristics and clinical outcomes of CML blast phase (CML-BP) patients whose blasts express antigens from more than one lineage are currently unknown. We systemically assessed lineage fidelity among patients with CML-BP using the definition of biphenotypic leukemia as proposed by the European Group for the Immunological Characterization of Leukemias (
EGIL; Leukemia 1995; 9:1783
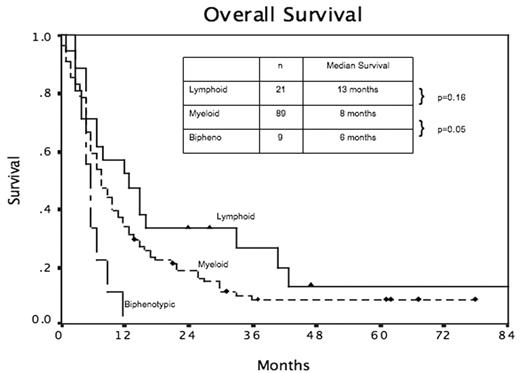
). Briefly, individual antigens are assigned scores based on known specificity for one of three lineages (myeloid, B-lymphoid or T-lymphoid); biphenotypic leukemia is defined by a score of >2 points for two lineages. Between 02/97 and 01/06, 163 patients were treated for CML-BP at the MD Anderson Cancer Center, of which 120 had adequate flow cytometric assessment for calculation of EGIL score. The number of patients by lineages was: 89 myeloid (74%), 21 lymphoid (17.5%; B 14%, T 3.5%), 9 biphenotypic (7.5%), 1 unclassifiable (<1%). Four of nine biphenotypic BP patients had a history of antecedent myeloid BP (n=3) or lymphoid BP (n=1). Lymphoid BP patients had lower mean white cell count (p=0.04), lower mean platelets (p=0.007) and higher mean bone marow blast percentage (p<0.001) than myeloid BP patients; those with biphenotypic BP had values between the lymphoid and myeloid groups. Seven imatinib-naïve biphenotypic patients received imatinib as initial therapy for CML-BP, with six regaining a second chronic phase; however, median time to failure was only 2 months and, with the exception of one patient censored for allogeneic transplantation, all patients progressed within 4 months. The patient who underwent allogeneic transplantation died of transplant-related complications. An additional patient who had previously failed imatinib and nilotinib in chronic phase had no response to dasatinib in biphenotypic BP. The final patient developed biphenotypia during resistant relapse of previous B-lymphoid BP, and received supportive therapy only. Overall survival for lymphoid, myeloid and biphenotypic BP were 13, 8 and 6 months respectively (p=0.04). In order to determine the significance of minor degrees of lineage aberrancy, we examined the survival of myeloid and lymphoid BP patients with EGIL score 1.0 – 2.0 in a second lineage. For lymphoid BP patients, minor expression of myeloid antigens did not affect survival; in contradistinction, myeloid BP patients with minor expression of lymphoid antigens had a trend to inferior survival. Biphenotypic BP may either be de-novo or may emerge from previous unilineage CML-BP, highlighting the trend for lineal infidelity in CML-BP. Responses to tyrosine kinase inhibitors are short-lived, and survival using current therapeutic strategies is very poor.Overall Survival
Disclosures: At the time of data collection, both nilotinib and dasatinib are of investigational status.; Dr Cortes receives research funding from Novartis and Bristol Myers Squibb.
Author notes
*
Corresponding author
2006, The American Society of Hematology
2006

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal