Abstract
Analysis of pre-transplant variables affecting the outcome of submyeloablative HSCT in 63 adult patients with hematologic malignancies identified refractory disease, poor performance status (ECOG 2/3), elevated LDH, and donor age >45 years as significant adverse prognostic factors (Mehta et al. ASH 2005, BMT 2006). The outcome of the next 28 patients treated identically was studied to see if the prognostic model developed from the first group was predictive of outcome of the second. The conditioning was 100 mg/m2 melphalan with (no prior auto) or without (prior auto) 50 mg/kg cyclophosphamide. GVHD prophylaxis comprised cyclosporine-mycophenolate (HLA-matched sibs) or tacrolimus-mycophenolate (others). G/GM-CSF were not administered routinely. All supportive care was uniform. As the table shows, the two groups of patients were comparable with reference to the major prognostic factors.
| . | Reference group (n=63) . | Test group (n=28) . | P . |
|---|---|---|---|
| Refractory disease | 60% | 64% | 0.72 |
| Performance status 2 or 3 | 25% | 14% | 0.28 |
| Donor age >45 y | 52% | 61% | 0.46 |
| High LDH | 44% | 18% | 0.21 |
| . | Reference group (n=63) . | Test group (n=28) . | P . |
|---|---|---|---|
| Refractory disease | 60% | 64% | 0.72 |
| Performance status 2 or 3 | 25% | 14% | 0.28 |
| Donor age >45 y | 52% | 61% | 0.46 |
| High LDH | 44% | 18% | 0.21 |
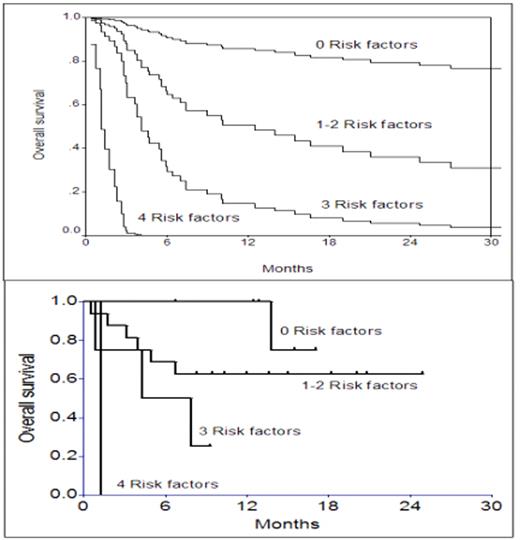
The upper part of the first figure shows adjusted overall survival curves based on the number of adverse prognostic factors derived from the Cox model in the first 63 patients (reference group). The lower part shows actuarial overall survival of the next 28 patients by the number of adverse prognostic factors.
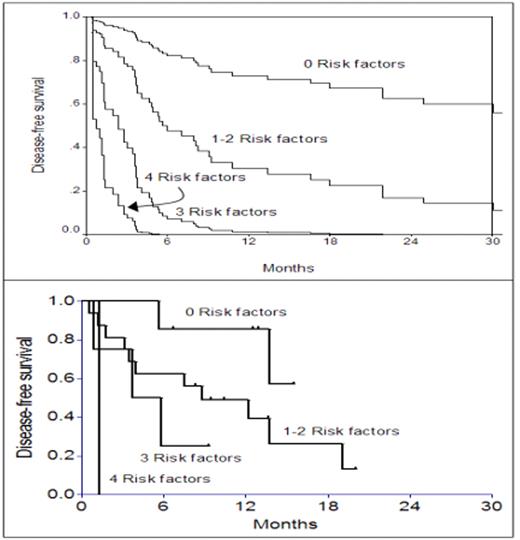
Similarly, the upper part of the second figure shows adjusted disease-free survival curves based on the number of adverse prognostic factors derived from the Cox model in the first 63 patients, and the lower part shows actuarial disease-free survival of the next 28 patients by the number of adverse prognostic factors.
As the figures show, the actual outcome of the second cohort of patients is similar to the outcome predicted by the prognostic model derived from the first cohort - validating the applicability of the model. It should be noted that the prognostic model may be different for other conditioning regimens. Also, while advanced patient age and HLA mismatch did not emerge as significant variables in this series, these variables need to explored further because the number of patients with these characteritics, expected to be adverse, was small (22% over 60 y and 12% HLA-mismatched). These data suggest that the combination of performance status, donor age, LDH, and disease chemosensitivity can be used to predict post-transplant prognosis in patients with hematologic malignancies. Identifying patients who are likely to experience a poor outcome post-transplant would then enable appropriate modification of the treatment regimen - such as reduction in the intensity of the regimen if toxicity is likely to be a concern, and intensification of the regimen and/or measures to augment graft-vs-tumor reactions if relapse is likely to be a concern.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal