Abstract
[Purpose] To compare the incidence, onset and severity of hepatic toxicities and their ultimate impact on survival after reduced-intensity HCT (RIST) and conventional HCT (CST).
[Patients and methods] We retrospectively reviewed the data of 151 patients with AML (n=86), MDS (32) and overt AML (33) who underwent allogeneic HCT after either RIST (n=78) or CST (73) between Jan, 2000, and Oct, 2004. Conditioning regimens for RIST included busulfan plus fludarabine or cladribine with or without 2–4 Gy TBI, and those for CST included cyclophosphamide with 12 Gy TBI or busulfan. The median age of the patients was 55 years (range, 15–67) for the RIST group and 37 years (1–57) for the CST group. Patients received marrow (n=64), G-CSF-mobilized PBSC (77) or cord blood (10) from either an HLA-matched relative (59), a mismatched relative (19) or an unrelated volunteer (73). The severity of liver toxicities was assessed by maximal measurements of total bilirubin, ALP, AST and ALT according to CTCAE v.3. Causes of hepatic toxicities were assessed basically by the clinical presentation and, in selected cases, by liver biopsy and autopsy results. The median follow-up of surviving patients was 1,401 days (598–2,317).
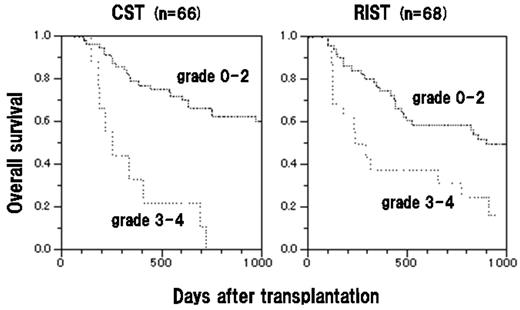
[Results] The incidences of grade 3–4 hepatic toxicities in the RIST and CST groups were, respectively, 38% vs 38% at day 30, and 60% vs 56% at day 100. The timing of maximum hepatic toxicity was also similar between the two groups. However, the incidence of grade 3–4 hyperbilirubinemia was higher in the RIST group after day 60, probably due to the late onset of acute GVHD after the early tapering of immunosuppression in this group. In contrast, there was a trend for more grade 3–4 abnormal transaminase levels in the CST group than in the RIST group, probably due to the toxicities of drugs including myeloablative conditioning. The causes of grade 3–4 hepatic toxicities were GVHD (n=27), drugs (27), conditioning regimen (7), VOD (3), and others (13). Among the 68 RIST and 66 CST patients who survived more than 100 days after HCT, overall survival (OS) was significantly worse in those who developed grade 3–4 hyperbilirubinemia during the first 100 days after HCT than in those who did not (Figure; 1-year OS, 38% vs 76% after RIST and 33% vs 79% after CST). In a multivariate ananysis, grade 3–4 hyperbilirubinemia (HR 1.8 [95% CI, 1.2–2.7], p=0.02) and non-remission status before HCT (HR 2.5 [95% CI, 1.5–4.4], p=0.0001) were associated with an increased risk of mortality. However, grade 3–4 abnormality in ALP and AST/ALT during the first 100 days after HCT was not a significant risk factor for mortality.
[Conclusions] Contrary to our expectations, our data showed a similar incidence of hepatic toxicities between the RIST and CST groups. This may be due to an older age population, the use of busulfan in the conditioning regimen, and the rapid tapering of immunosuppression in the RIST group. The outcome of patients who developed severe grade 3–4 hyperbilirubinemia was poor regardless of the conditioning regimen.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal