Abstract
Being underweight or markedly overweight is associated with poorer outcome after myeloablative allogeneic HSCT. The role of body weight after reduced-intensity HSCT is unknown. The outcome of 91 patients (19–71 y, median 53) with hematologic malignancies undergoing submyeloablative allogeneic HSCT was studied to determine the effect of weight. 8 patients were >10% underweight (A), 33 were from ≤10% underweight to ≤10% overweight (B), 41 were >10% but ≤50% overweight (C), and 9 were >50% overweight (D). Donors were HLA-matched siblings (n=51), 10/10 allele-matched unrelated (n=29), or 1-locus/allele mismatched (n=11). The conditioning comprised 100 mg/m2 melphalan with (n=50; no prior auto) or without (n=41; prior auto) 50 mg/kg cyclophosphamide. Cyclophosphamide dose was based on actual weight in underweight patients and adjusted ideal weight [ideal + 0.25(actual-ideal)] in overweight patients, while melphalan dose was usually based on the actual weight if it did not exceed ideal weight by >20%. Above that, adjusted ideal weight was used. GVHD prophylaxis comprised cyclosporine-mycophenolate (HLA-matched sibs) or tacrolimus-mycophenolate (others). G/GM-CSF were not given routinely. Supportive care was uniform.
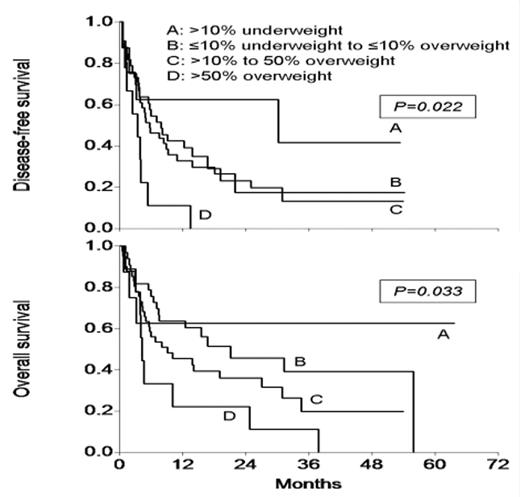
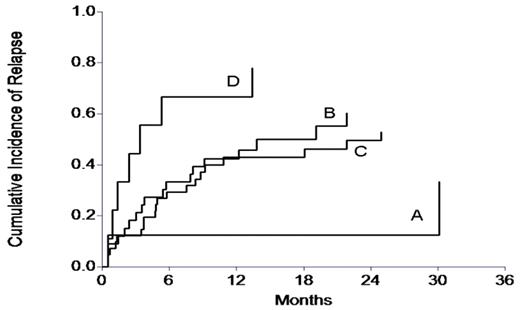
As the figure above shows, weight affected overall (OS) and disease-free (DFS) survival significantly. When analyzed as a continuous variable, increasing difference between actual and ideal weight (i.e. increasing overweight) had a detrimental effect on OS (RR 1.0017; 95% CI 1.0036–1.0198; P=0.005) and DFS (RR 1.0092; 95% CI 1.0012–1.0173; P=0.023). Weight difference was also analyzed in a Cox model with chemosensitivity (refractory or not), performance status (PS; 0/1 or 2/3), donor age (<45 or ≥45), and LDH (elevated or not) - variables shown to affect outcome significantly in this group of patients (Mehta et al. ASH 2006, BMT 2006). The 4 known prognostic factors retained their significance, and weight difference was also found to affect DFS and OS significantly. Transplant-related mortality was not affected by weight but relapse was - as shown in the figure below.
Further Cox analysis showed that relapse was significantly affected by chemosensitivity, donor age, and weight difference. Transplant-related mortality was affected by donor age and LDH. The effect of PS on TRM disappeared when weight difference was introduced in the model although there was no correlation between weight difference and PS. This observation of lower weights affecting outcome favorably through lower relapse is somewhat unexpected, and requires confirmation in other series of patients undergoing submyeloablative allografts. Possible reasons for this may be a greater amount of chemotherapy delivered based on actual weight in group A compared to groups B, C and D, and leptin-mediated immunomodulation with attenuation of graft-vs-tumor effects with increasing weight.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal