Abstract
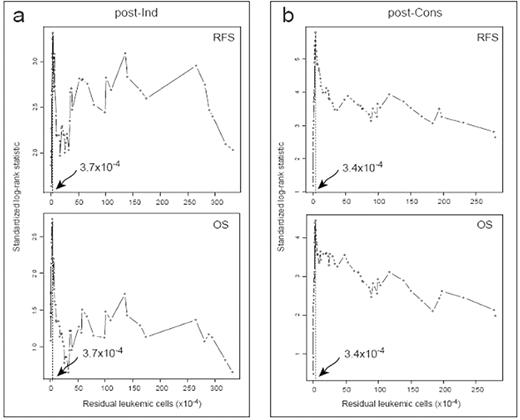
The current experience in the use of multiparametric flow-cytometry for immunological detection of MRD in AML, indicates that the method is feasible, rapid and relatively sensitive. In our previous studies of AML patients with aberrant phenotype (Blood 2000, Leukemia 2003 & 2006), we found that the level of MRD after consolidation therapy was the best predictor of outcome. In fact, a MRD level higher than 3.5x10−4 residual leukemic cells after consolidation was significantly correlated with a poor outcome. The major problem with using an empirically established cut-off to define thresholds is that it may not be reproducible over different populations of patients. In order to confirm the prognostic value of the threshold of 3.5x10−4 residual leukemic cells, previously selected, we used the Maximally Selected Rank Statistic analysis to determine optimal cutpoint, yielding the best separation of AML patients into two groups with different OS and/or RFS probabilities. To do this, we evaluated the trend of standardized log-rank statistics using RFS (Fig. 1, upper panels) and OS (Fig. 1, lower panels) as dependent variables, and the values of residual leukemic cells, determined both at the post-Induction (post-Ind) and post-consolidation (post-Cons) checkpoints, as independent variable (Fig. 1A and 1B, respectively). The experimental cut-off points, identified as the absolute peak in standardized log-rank statistics plots (vertical dotted lines in Fig. 1), were 3.7x10−4 and 3.4x10−4 residual leukemic cells for post-Ind and post-Cons values, respectively. According to this data we decided to utilize the 3.5x10−4 residual leukemic cells cut-off value to discriminate MRD− from MRD+ cases both after induction and consolidation. Therefore, patients with a residual leukemic cells values below the cutoff of 3.5×10−4 will be referred to as MRD−, while those with residual leukemic cells equal or exceeding the 3.5×10−4 level will be classified as MRD+. Post-Cons MRD− patients had a superior outcome in terms of relapse rate (27% vs. 78%, P<0.001), 7-years OS (64% vs. 14%, P<0.001) and RFS (68% vs. 13%, P<0.001). Moreover, post-Cons MRD− patients had a better outcome regardless of the MRD status after induction: in particular, patients entering MRD negativity only after consolidation showed the same outcome as those achieving early negativity after induction. Multivariate analysis, including karyotype, age, MDR1 phenotype, post-Ind and post-Cons MRD levels, indicated that the post-Cons MRD status independently affected relapse rate, OS and RFS (P<0.001, for all comparisons). In conclusion:
the threshold of 3.5x10−4 is valid in discriminating risk categories in adult AML;
post-consolidation MRD assessment is critical to predict disease outcome regardless of the MRD status after induction.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal