Comment on Braiteh et al, page 2992
Erdheim-Chester disease is a rare form of non-Langerhans histiocytosis that is rapidly fatal. No specific therapy has been proven effective. A report in this issue establishes a rationale for and effectiveness of interferon in this disorder.
Interest in interferon-α as an anticancer agent has waxed and waned since its clinical development more than 30 years ago. For several tumor types, notably, chronic myeloid leukemia (CML) and hairy cell leukemia, interferon was, at one time, considered an important component of clinical management. Interferons mediate a farrago of biologic effects. Besides antiviral activity, interferons demonstrate growth inhibitory, differentiation induction, immunomodulatory, and anti-angiogenic effects, as well as enhancement of tumor-associated antigen expression.1 These diverse effects, while leading to an interest in interferon to treat a wide variety of disorders, have made it difficult to pinpoint an exact mechanism(s) of action and have resulted in side effects in patients. With the development of specific, more effective, and better tolerated therapies—imatinib mesylate for CML, 2-chlorodeoxyadenosine (2CDA) for hairy cell leukemia—interferon has been relegated to a minor role in these disorders. Nevertheless, clinical interest in interferon continues. In this issue, Braiteh and colleagues report on a new use of interferon-α in a rare histiocytic disorder, Erdheim-Chester (E-C) disease.FIG1
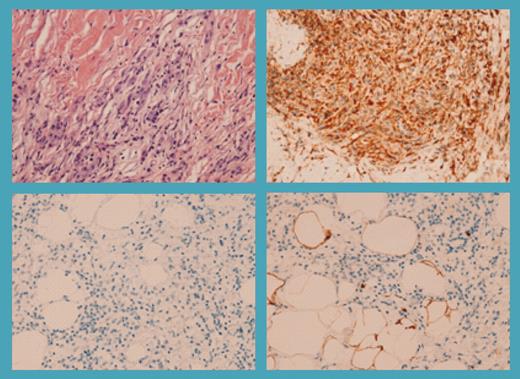
Retro-orbital and retroperitoneal disease in patient 1. See the complete figure in the article beginning on page 2992.
Retro-orbital and retroperitoneal disease in patient 1. See the complete figure in the article beginning on page 2992.
The histiocytic syndromes, broadly categorized as Langerhans cell and non–Langerhans cell histiocytosis, comprise an uncommon group of diseases characterized by accumulation and infiltration of macrophage- or histiocyte-like cells into multiple organs.2 The Langerhans cell is a bone marrow–derived, CD34+ cell of myeloid lineage, which differentiates to macrophages and dendritic cells under cytokine and chemokine influences. Immunocytochemical studies from patients with Langerhans cell histiocytosis have established that these cells, in contrast to normal Langerhans cells, are immature dendritic cells that have not undergone differentiation. The pathologic Langerhans histiocytes overexpress receptors for inflammatory chemokines (CCR1, CCR2, CXCR1), which allow for recruitment of other immature dendritic cells and fail to express chemokines, such as CXCR4 and CCR7, which help mediate migration to secondary sites.
Type I interferons alone, and in unison with other cytokines, have been shown to enhance terminal differentiation and activate migration of histiocytes, progenitor cell–derived dendritic cells, and Langerhans cells.3 These observations suggested a rationale for use in the histiocytic–dendritic cell disorders. Braiteh et al report 3 patients with E-C disease who were treated with interferon-α. Responses in the 3 patients were significant and durable. E-C shares clinical features with that of the Langerhans cell histiocytosis but carries a worse prognosis, with a reported 3-year survival of 50%.4 Cells from E-C patients do not have a Langerhans cell phenotype, lack Birbeck granules, and stain negative for CD1a and CD207, all distinctly positive features of Langerhans cell histiocytosis. This report, along with case studies of the activity of interferon in Langerhans histiocytosis, should encourage further evaluation of this agent in the dendritic-histiocytic cell diseases.
These observations still leave us with the question of the mechanism by which interferon works. Although differentiation of the histiocyte–dendritic cell to terminal maturation and apoptosis is an attractive hypothesis, it has not been proven. Other effects of interferon-α, such as up-regulation of natural killer (NK) cells, activation of protein kinase C signaling pathways within histiocytes, or direct antiproliferative effects, could also explain the activity of interferon seen in these patients.5 In any event, interferon—despite, or rather, because of its unnumbered effects—has once again emerged as an effective tool in a rare group of disorders for which there are limited options for many patients. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal