Abstract
Background
Approximately 60,000 people are born with thalassaemia major every year. The average life expectancy of thalassaemia major patients is 35 years due to iron overload Cardiomyopathy. The cardiomyopathy is reversible when treated early, but once heart failure is established it is often rapidly progressive, and unresponsive to treatment. The single breath hold (SBH) T2* technique has been validated as the most robust and reproducible non-invasive measurement of myocardial and iron load. Our aim in this study was to validate the transferability and reproducibility of this technique in different scanners worldwide.
Methods
We aim to compare the reproducibility in six different sites worldwide as part of an NIH funded grant (R01-DK66084-01). So far, two of these sites have been validated: Singapore (Siemens Sonata, 1.5T scanner) and Cagliari, Italy (GE Signa, 1.5 T scanner). At both validation sites, 10 patients were scanned for heart and liver T2*, and scans were repeated for interstudy reproducibility. All patients then flew to London to be rescanned on our reference Siemens Sonata scanner.
Results
Of the 20 patients scanned, 70% had myocardial iron loading (T2* <20ms) and in 10% the myocardial iron loading was severe.
Liver iron loading was present in 65% of patients and in 30% this was severe.
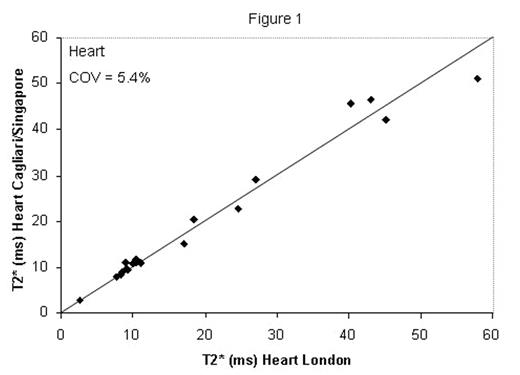
The coefficient of variation (COV) for the heart T2* measurements between the local sites and London was 5.9% and 4.9% yielding an average coefficient of variation across both sites of 5.4% (figure 1).
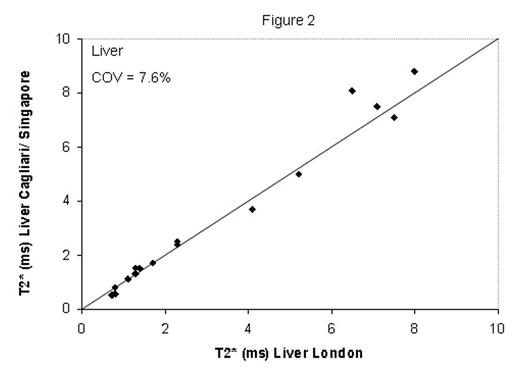
The coefficient of variation (COV) for the liver T2* measurements between the local sites and London was 11.3% and 3.9% yielding an average coefficient of variation across both sites of 7.6% (figure 2).
There was no significant correlation between liver and myocardial loading.
Conclusion
These are the first data demonstrating the transferability of the SBH T2* technique and the clinical validation from the 2 collaborating centers were excellent for both heart and liver measurements. Further MR sites confirmed for validation include Children’s Hospital of Philadelphia (USA); Ramathibodi Hospital, Bangkok (Thailand); and Chinese University Hong Kong.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal