Abstract
Background: Allogeneic hematopoietic stem cell transplantation is potentially curative in agnogenic myeloid metaplasia (AMM) but is associated with substantial mortality and morbidity that necessitates accurate identification of patients in whom benefit outweighs risk. The current single institutional study investigates prognostic variables in transplant-eligible patients with AMM with the main objective of improved discrimination between intermediate- and high-risk patient categories.
Methods: Patients diagnosed with AMM before the age of 60 years and seen at Mayo Clinic were identified and the diagnosis confirmed. Relevant demographic, clinical and laboratory characteristics were abstracted and the impact of various parameters on overall survival was evaluated with univariate and multivariate analysis.
Results: A cohort of 159 patients (median age 52 years, range 18–60; 89 males) with AMM is described. Median follow-up from initial diagnosis was 63 months (range 0–300). During this period, 102 patients have died; overall median survival 79 months. Multivariate analysis of parameters measured in all study patients at diagnosis identified thrombocytopenia (platelet count < 100 x 109/L) as the strongest predictor of inferior survival (p=0.002). In addition, a hemoglobin level of <10 g/dL (p=0.003), white blood cell count of either <4 or >30 x 109/L (p=0.03), and older age (p=0.02) were also found to be independent indicators of poor prognosis. However, when the analysis included parameters that were measured in variable proportion of the study population, the independent prognostic factors for poor survival were thrombocytopenia (p=0.0001), anemia (p=0.01), and the presence of unfavorable cytogenetic abnormalities (0.001).
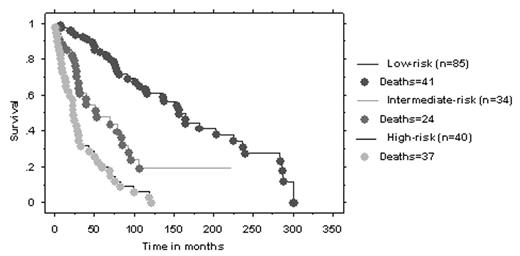
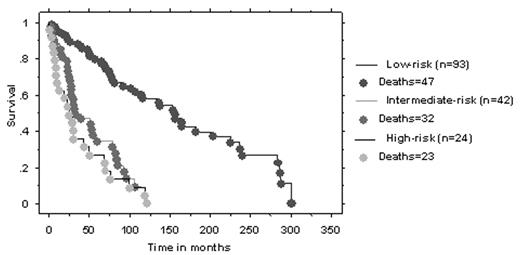
Based on the above findings, we constructed a new complete blood count (CBC)-based prognostic scoring system (Figure 1) that performed better than the Dupriez scoring system in discriminating intermediate- from high-risk patient categories(Figure 2).
Conclusions: Thrombocytopenia is a strong predictor of poor survival in transplant-eligible patients with AMM. The incorporation of platelet count into the Dupriez prognostic scoring system might allow the construction of an improved, CBC-based scoring system that can accurately identify high-risk as well as intermediate-risk patients with AMM.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal