Abstract
We investigated the kinetics of hematologic change in patients with sickle cell disease (SCD, HbSS, n=6) or SC disease (HbSC, n=1) who had been newly started on hydroxyurea (HU), with the intention of identifying early correlates to fetal hemoglobin (HbF) responsiveness. We found that HbF increased in all patients on HU, and that the half-maximal degree of HbF response could be estimated by 2 months, in patients’ whose MCVs had risen ≥ 10% above baseline.
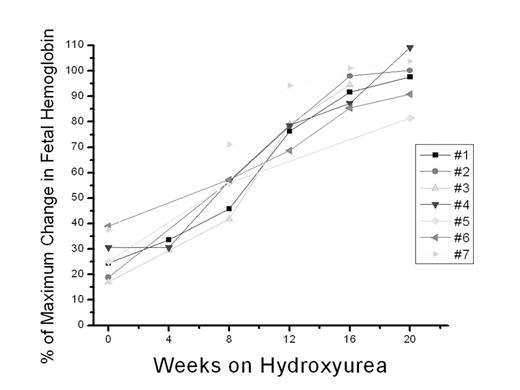
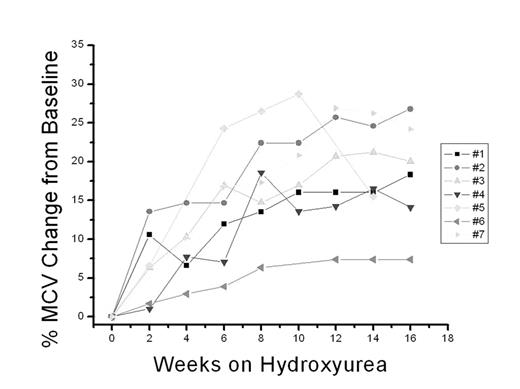
All 7 patients were treated with HU and followed closely for 6 months or more, until hematologic stability. Hematologic stability was apparent by ≥ 5 months. White blood cell count (WBC), absolute neutrophil count (ANC), reticulocyte (retic) count, % HbF, and mean corpuscular volume (MCV) were examined at bi-weekly intervals. Baseline values (1 or 2 values averaged) were compared with mean values obtained during weeks 2 to 8 (3 or 4 values averaged). As expected, by 2 months WBC and ANC had fallen 30 +/− 8% and 26 +/− 8%, respectively. Change in total hemoglobin (5.8 +/−6.7%), total platelet count (less 11 +/− 10.8%), and LDH (5.3 +/− 8.7%) was not consistent during this two month interval. By eight weeks after initiation of HU, retic counts had dropped in all six SS patients, from 15 to 52% less than baseline while MCV rose 9–21% above baseline; in general, rise in MCV preceded the rise in HbF. Overall, by the time of hematologic stability, all patients had increased their percent HbF, at between 3–8.5-fold relative to baseline; baseline percent HbF of total hemoglobin (Hgb) ranged from 0.7 to 8.3% and, after stabilization, from 5.2% to 24.9%. Maximal percentage of Hgb that was accounted for by HbF at stabilization was arbitrarily set at 100; at 8 weeks, all patients had achieved ≥ 42% of their maximal HbF level, mean 55 +/− 9.4% of maximum HbF. Two additional patients in whom extensive lab data were available, but who were suspected to be non-compliant or sub-therapeutically treated, had a >10% rise in MCV that was temporally associated with an inflection upward for HbF. Patient 8 had mean bi-weekly MCVs of 94, 91, 93, and, after a family conference, 102 (p=.003); Concurrent HbF was 7, 6, 6 and then 10 (p=.046). Patient 9 had mean bi-weekly MCVs on low-dose HU of 97, 96, and, after dose adjustment, 109(p=.003); HbF was 2%, 3%, and then 5 (p=.0094).
We speculate that, in many patients, an increase in MCV above baseline of ≥ 10% is a marker of adequate HU dosing, and that HbF levels at that time approximate half-maximal response. A larger series will be necessary to confirm this relationship; a predictive model, correlating MCV and HbF responsiveness, could be used to determine sufficiency of, and compliance to, HU therapy, and to early identify patients who are at high-risk from SCD (e.g. with pulmonary hypertension) whose HbF responsiveness may not be adequate from HU alone.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal