Abstract
Introduction: We previously reported that serum cardiac biomarkers are among the most powerful predictors of overall survival. This observation was based on outcomes of more than 300 patients with primary systemic amyloidosis (AL) receiving either low dose chemotherapy or high dose chemotherapy with peripheral blood stem cell transplant (PBSCT). Not all institutions use the N-terminal pro-brain natriuretic peptide (NTproBNP) assay, but rather the B-type natriuretic peptide (BNP) assay. We therefore determined the relative utility of BNP in patients with AL undergoing PBSCT and up-dated our results using our NTproBNP-troponin T staging system. Methods: Between 4/10/96 and 2/24/05, 164 patients with AL undergoing PBSCT had measurements of serum cardiac biomarkers. All BNP measurements were done on fresh serum (Biosite Inc., San Diego). The NTproBNP (Roche Diagnostics, Indianapolis, IN) and troponin T (TnT) (Roche Diagnostics, Indianapolis, IN) measurements were done on either stored serum or on fresh samples as previously reported. Follow-up for patients was through March 2005.
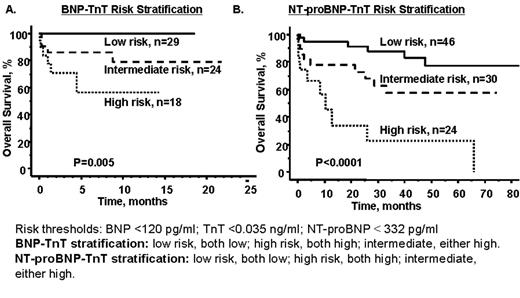
Results: Between 5/1/03 and 2/15/05, 72 patients had BNP measurements pre-transplant. The median value was 167 pg/ml (range 5 to 7739). Forty-two of these patients also had an NTproBNP measured. There was good agreement between the two tests in the 42 patients that had both measurements (rho 0.823, p<0.0001). To further test the relationship between the two tests, we evaluated the correlation between BNP and NTproBNP using 204 simultaneous measurements from 106 patients (rho=0.89, p<0.0001). Next, we tested the prognostic utility of BNP. Using a cut-off point of 120 pg/L (the upper limit of normal for women over the age of 70 and the 50th percentile of all measurements in our data set), we found that BNP was prognostic for survival post-transplant. It was independent of TnT values, and patients could be divided into 3 risk categories using these two measurements (low risk if both values were low, high-risk if both were high, and intermediate if either was high). This system was highly predictive of overall survival (Figure A). We next compared the BNP-TnT staging system to our previously reported NTproBNP-TnT staging system in the 42 patients that had all 3 values pre-transplant. The correlation between the two staging systems was excellent (rho=0.91, p<0.0001). Follow-up for the 100 patients who had been reported previously is now 26.9 months. As shown in Figure B, the NTproBNP-TnT system predicts for overall survival post transplant.
Conclusions: Serum levels of cardiac biomarkers are invaluable prognostic markers in patients with AL. Preliminary data would suggest that a BNP-TnT system is as useful as the NTproBNP-TnT system.
Risk thresholds: BNP <120 pg/ml; TnT <0.035 ng/ml; NT-proBNP < 332 pg/ml BNP-TnT statisfaction: low risk, both low; high risk, both high; intermediate, either high. NT-proBNP-TnT satisfaction: low risk, both low; high risk, both high; intermediate, either high.
Risk thresholds: BNP <120 pg/ml; TnT <0.035 ng/ml; NT-proBNP < 332 pg/ml BNP-TnT statisfaction: low risk, both low; high risk, both high; intermediate, either high. NT-proBNP-TnT satisfaction: low risk, both low; high risk, both high; intermediate, either high.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal