Comment on Feldmann et al, page 2658
In this issue of Blood, Feldmann and colleagues highlight a congenital immune defect that may underlie an isolated severe encephalitis-like neurological disorder.
Perhaps no other field of medicine has seen such a rapid increase in knowledge as that of congenital disorders of the immune system. Immunodeficiencies initially thought to differ only by genetic alteration and pathogenic mechanism are now known to make up 130 distinct entities. The various molecules identified to date often share the property of being involved in signaling pathways responsible for specific functions. However, the more cases identified with that specific alteration, the clearer it is that the individual clinical phenotype differs profoundly among the distinct forms. In real patients, disease presents with clinical features that differ profoundly from the classical presenting signs of an immune defect. An example of how profoundly the clinical history of a real case may differ from what is generally expected for a particular functional impairment is familial hemophagocytic lymphohistiocytosis (FHL) associated with defective cytolytic activity.
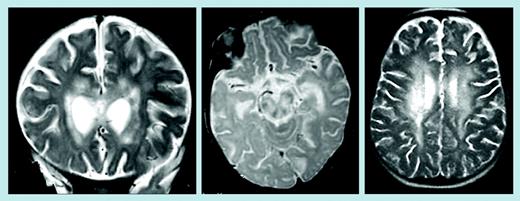
In this issue of Blood, Feldmann and colleagues report on 2 patients affected with FHL presenting initially as an isolated severe and progressive neurologic disorder resembling acute encephalitis and characterized by large lesions of white matter in periventricular areas and brain stem, as seen on magnetic resonance imaging. The clinical phenotype was associated with a missense mutation in the perforin (PRF1) gene, which affected the in vitro cytolytic activity. Based on these data, the authors suggest that PRF1 gene and function should be evaluated in such patients. The results of this study have several implications. First, a rapidly progressive disease involving only one organ, such as the brain or liver, may be per se a sign of an immunodeficiency. It is notable that physicians very rarely suspect an immunologic defect in such cases. Moreover, a few generally accepted diagnostic criteria for FHL are lacking in these 2 patients, thus implying that the current criteria may not be appropriate to identify all patients and thus that an effort should be made to better define clinical and laboratory features.FIG1
Brain magnetic resonance images of patients 1 and 2. See the complete figure in the article beginning on page 2658.
Brain magnetic resonance images of patients 1 and 2. See the complete figure in the article beginning on page 2658.
As pure speculation, it should also be considered that some nonhematologic clinical problems of immunodeficient patients may not necessarily be infectious in nature but directly related to the extrahematopoietic role of the molecule whose alteration causes the immunodeficiency.
As a result of their overly conservative education, some physicians are prone to emphasize the “traditional” immunodeficiencies, which are the most easily recognized syndromes. This has led to a tendency to underestimate the number of novel immunodeficiencies and their presenting phenotypes, and has resulted in poor quality of health care for some patients. To better understand the prevalence of novel immunodeficiencies, a future effort must be made to analyze presenting signs of diagnosed cases and to increase the number of diagnostic centers so that a greater number of patients with suspicious clinical presentations can be diagnosed. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal