Abstract
The effectiveness of different methods of leukoreduction in preventing alloimmune platelet refractoriness was evaluated in a canine model. Platelets from a random donor dog were administered for up to 8 weeks or until platelet refractoriness. Standard (STD; unmodified) platelets were accepted by 14% of recipients (n = 7) compared with 14% for centrifuge leukoreduced (C-LR) platelets (n = 21) and 31% for filter leukoreduced (F-LR) platelets (n = 13; no significant differences). Surprisingly, using both F-LR and C-LR platelets was highly effective (87% acceptance, n = 15). Transfusing F-LR/C-LR red blood cells (n = 4) or F-LR/C-LR plasma (n = 4), along with F-LR/C-LR platelets, did not affect platelet acceptance (100% acceptance). Overall acceptance of F-LR/C-LR platelets was 91% (n = 23; P ≤ .05 versus STD, C-LR, or F-LR platelets). F-LR/C-LR transfusions also induced tolerance to subsequent STD platelet transfusions from the same donor (82% acceptance, n = 19) as well as to donor skin grafts without recipient immunosuppression (57% acceptance, n = 7). To evaluate mechanisms of tolerance induction, F-LR/C-LR platelets were γ-irradiated. Although the γ-irradiated F-LR/C-LR platelets were uniformly accepted (n = 6), tolerance to STD platelets was lost. These data suggest that some allostimulatory white cells are filter adherent, whereas others escape filtration but can be removed by centrifugation and tolerance requires a residual functioning white cell.
Introduction
Prolonged periods of thrombocytopenia requiring repeated platelet transfusions often result in alloimmunization. In one recent study, platelet alloimmunization to standard (nonleukoreduced) platelet transfusions developed in 45% of acute myeloid leukemia (AML) patients undergoing induction chemotherapy.1 Development of alloantibodies is often associated with clinical platelet refractoriness and an increased bleeding risk. Due to the difficulties of providing platelet support when alloimmunization occurs,2 several different strategies to prevent alloimmunization have been evaluated in patients and animal models. Most of these strategies rely on removing the donor's antigen-presenting cells (APCs) by filtration to prevent immune recognition.1,3-13 However, filtration leukoreduction is not uniformly successful (eg, in a large trial, 18% of patients given filter leukoreduced platelets still became alloimmunized).1
The dog is a valuable preclinical model for predicting human responses to platelet transfusions.14,15 We compared rates of alloimmune platelet refractoriness following standard (STD; unmodified) platelet transfusions versus centrifuge leukoreduced (C-LR) and filter leukoreduced (F-LR) or combined (F-LR/C-LR) platelet transfusions. In addition, we evaluated whether these treated platelet transfusions would induce tolerance to subsequent STD platelet transfusions or even skin grafts.
Materials and methods
Experimental animals
Dogs were housed at the Fred Hutchinson Cancer Research Center (FHCRC) animal facilities, and the protocols used were approved by the FHCRC Institutional Animal Care and Use Committee. A total of 92 dogs were used, 22 as donors and 70 as recipients.
Reagents and filters
Acid citrate dextrose (ACD) and Ringer citrate dextrose (RCD) were obtained from the Fred Hutchinson Cancer Research Center (Seattle, WA). PFL-1, PXL, PL1-B, and ASTPL pediatric platelet leukoreduction filters were used based on their availability from the manufacturer. BPF 4S filters were used for red cell leukoreduction. All filters were generously donated by the Pall Corporation (East Hills, NY).
Platelet component preparations
All platelet preparations started with ACD anticoagulated whole blood. For a STD platelet transfusion, platelet-rich plasma (PRP) was prepared by centrifuging 30 to 60 mL of whole blood diluted 1:1 with RCD for 10 minutes at 250g in a 150-mL transfer pack (Baxter/Fenwal, Deerfield, IL). The PRP was expressed into another transfer pack and centrifuged at 900g for 10 minutes, the supernatant was expressed, and the pellet was resuspended in 6 mL of added RCD.
C-LR platelets were made by centrifuging the 6 mL of STD platelets for 5 minutes at 180g in a tube. The supernatant from this preparation constituted the C-LR platelets. The F-LR platelets were prepared by filtering the PRP using either 1 or 2 of the same type of filter sequentially prior to pelleting. Two filters were used to determine if a further reduction in the number of contaminating leukocytes would improve the acceptance of donor platelets. F-LR/C-LR transfusions were made by conducting the C-LR step on F-LR platelets.
As F-LR/C-LR platelets were accepted by most donors, we evaluated whether F-LR/C-LR plasma or F-LR/C-LR washed red blood cells (RBCs) added back to the same donor's F-LR/C-LR platelets would reduce acceptance rates. Plasma add-backs were done by centrifuging 20 mL of ACD blood at 3800g for 15 minutes. The supernatant plasma was filtered with a platelet filter and injected along with the donor's F-LR/C-LR platelets. The RBC add-backs were prepared from the residual packed RBCs obtained after removing the PRP. The RBCs were diluted with an equal volume of RCD, filtered sequentially through 2 whole-blood filters, and the filtered RBCs were transferred to a vacutainer tube. The tube was inverted and spun at 180g for 5 minutes, and 2 mL of RBCs was removed through the inverted rubber stopper. The RBCs were washed twice with saline, and 0.5 mL was added to the donor's F-LR/C-LR platelets.
We further investigated the potential role of any residual white blood cells (WBCs) in the F-LR/C-LR platelets in the induction of tolerance by γ-irradiating whole blood from the initial donor at a dose of 25 Gy (Gamma Cell 1000 Irradiator; Atomic Energy of Canada, Mississauga, Ontario, Canada) prior to preparing F-LR/C-LR platelets (γ–F-LR/C-LR platelets).
Radiolabeling of donor platelets
To determine the recovery and survival of the donor dog's platelets in the transfused recipient, the donor's platelets were radiolabeled with 51Cr16 and resuspended in 6 mL of RCD, and 5 mL was injected within 4 to 8 hours of collection. Two 0.1-mL aliquots of the radiolabeled platelets were counted for radioactivity to allow a determination of the total amount of radioactivity injected. Two-milliliter samples of EDTA (ethylenediaminetetraacetic acid) blood were drawn from the transfused recipients at 1 and 20 hours after injection, then daily thereafter for up to 4 days. Radioactivity in the samples was determined using a gamma counter (Packard Minaxi Auto Gamma 5000 series; Packard, Downers Grove, IL). Platelet survival was estimated by computerized fitting of the radioactive counts in each blood sample. Initial platelet recovery was obtained by extrapolating the survival curve back to time zero. In 73 normal dogs, autologous platelet recoveries averaged 53% ± 12%, and platelet survivals averaged 4.1 ± 0.8 days (± 1 SD). Rejection of donor platelets was defined as the recovery of 5% or less of the donor's injected platelet radioactivity at 20 hours after transfusion following 2 sequential weekly transfusions. This criterion was selected, as a survival of less than 1 day would not be a useful transfusion.
Platelet and WBC counts of the platelet preparations
Platelet counts were determined by a Coulter T890 Automatic Hematology Analyzer (Coulter, Hialeah, FL) and WBC counts were determined by propidium iodide staining of leukocytes.17 The lower limit of sensitivity for the WBC counts is 0.0006 × 109/L (0.6 WBCs/μL) or 3 × 103 WBCs per transfusion.
Antibody detection
Antibody detection techniques evolved over time. For the initial experiments, no antibody detection tests were performed, and any platelet refractoriness that developed in these normal dogs was assumed to be antibody mediated. A platelet Staph A enzyme-linked immunosorbent assay (ELISA) assay was adapted for the dog,18 and, later, a modified flow cytometry assay19 was used to detect antibodies against both the donor's platelets and lymphocytes.
For the ELISA, PRP from EDTA anticoagulated blood was plated onto a 96-well round-bottom plate (Nunc, Roskilde, Denmark), reacted with test sera, washed, and incubated with Staph Protein-A conjugated to alkaline phosphatase (Roche Molecular Biochemicals, Indianapolis, IN), then washed again and allowed to react with phosphatase substrate (Sigma 104; Sigma Diagnostics, St Louis, MO). A positive reaction, similar to that in our human antibody studies,18 was defined as an optical density read with a Microplate Autoreader (EL-310; Biotek Instruments, Winooski, VT) more than 1.2 times that of a negative sera pool run against the same platelet preparation.
The flow assay used EDTA whole blood that was RBC lysed with ammonium chloride, reacted with test sera, and washed, and platelet- or lymphocyte-bound immunoglobulin G (IgG) was detected with anti–dog IgG–fluorescein isothiocyanate (FITC; Jackson Immuno Research Laboratories, West Grove, PA). A total of 10 000 events were acquired, then platelets and lymphocytes were gated according to characteristic size and complexity and subsequently analyzed for FL-1 intensities (FACScan, Lysis II; Becton Dickinson, San Jose, CA). A serum sample that resulted in a shift in FL-1 intensity by the mean population of gated cells of 100 channels above that of the negative control pooled sera on a 1024-channel scale was considered a positive test result. This represented a 10% change in reactivity and was considered to be specific enough to define a relevant immune response.
Baseline and weekly recipient serum samples for antibody testing were frozen at -80°C, and these samples were batch tested at study conclusion against fresh autologous and donor cells. For both antibody assays, 2 sequential samples had to test positive by the assay criteria before the result was considered positive.
Skin grafting
Some platelet recipients had skin grafts performed from 1 or 2 of their platelet donors and an autologous graft. Recipients were selected for skin grafting only if they had accepted F-LR/C-LR platelets from their initial donor and then a mix of those who had accepted or rejected platelets from third-party donors was used. This allowed us to determine whether platelet acceptance predicted acceptance of skin grafts. Skin grafting was performed under anesthesia, an autologous skin patch was removed, the hair growth direction was reoriented, and the autologous skin graft was reapplied with sutures. An allogeneic skin patch was removed from a platelet donor, an autologous patch of skin was removed from the recipient, and the allogeneic skin graft was sutured in place. Graft sites were inspected daily for up to 21 days after grafting for evidence of rejection as determined by at least two thirds of the graft site having undergone necrosis. There was no pregrafting or postgrafting immunosuppression given.
Trial design
Selection of donor/recipient pairs. Recipient and donor dogs were kennelbred and of either sex. None of the female dogs had been pregnant. Both recipient and donor dogs had 2 radiolabeled autologous platelet recovery and survival measurements prior to study entry to ensure they had no underlying condition that would compromise their response to transfused donor platelets and to demonstrate that their platelets should survive normally after transfusion, respectively. All of the dogs had normal autologous platelet recoveries and survivals. Using an ELISA, baseline recipient serum samples were screened for antibodies against platelet samples from random donor dogs; only cross-match–negative donor-recipient pairs were used. Of the 46 recipient dogs who had antibody tests performed with potential donor dogs prior to transfusion, the antibody tests were negative with 138 donors and they were positive with 85 donors (38% of the donors). As dogs are usually born in litters, there may have been inadvertent cross-contamination of body fluids, there may be naturally occurring antibodies to platelets, or possibly there were immune responses to immunizations given to the dogs.
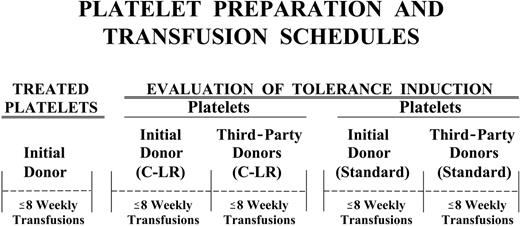
Evaluation of the immunogenicity of platelet preparations and tolerance induction. During the treatment phase, each recipient received up to 8 weekly transfusions of their assigned platelet preparation from their initial donor. If the recipient remained nonrefractory through 8 transfusions, it was deemed to have accepted that platelet product. If the recipient had 2 sequential platelet recoveries of 5% or less before completing 8 transfusions, it was declared platelet refractory. The recipient was considered to have accepted platelets until the time of the first refractory transfusion (eg, if the recovery of donor platelets was ≤ 5% at 24 hours after transfusion with their sixth transfusion, they were considered to have accepted donor platelets for 5 transfusions). At the end of 8 weeks, or with the development of platelet refractoriness, platelet transfusions from the next donor were given (Figure 1).
Sequence of donor platelet transfusions. Each recipient received up to 8 weekly transfusions from a donor, or until the recipient became platelet refractory. Refractoriness was defined as less than 5% of the donor's platelets circulating in a transfused recipient at 20 hours after transfusion after 2 sequential transfusions. As soon as a recipient developed refractoriness to a donor, or at the end of 8 weeks, platelet transfusions from the next donor were given. Different types of donor platelet transfusions were given in order, moving from left to right in the figure. For the tolerance evaluation studies, some recipients received only C-LR platelets from their initial and third-party donors, some recipients received only STD platelets from these donors, and some recipients received both C-LR and STD platelets from these donors. Third-party donors were donors that the recipient had not received before.
Sequence of donor platelet transfusions. Each recipient received up to 8 weekly transfusions from a donor, or until the recipient became platelet refractory. Refractoriness was defined as less than 5% of the donor's platelets circulating in a transfused recipient at 20 hours after transfusion after 2 sequential transfusions. As soon as a recipient developed refractoriness to a donor, or at the end of 8 weeks, platelet transfusions from the next donor were given. Different types of donor platelet transfusions were given in order, moving from left to right in the figure. For the tolerance evaluation studies, some recipients received only C-LR platelets from their initial and third-party donors, some recipients received only STD platelets from these donors, and some recipients received both C-LR and STD platelets from these donors. Third-party donors were donors that the recipient had not received before.
Groups of animals were assigned to specific transfusion programs, and at the conclusion of one treatment program, another program was initiated. The C-LR initial donor transfusions were originally performed and reported in 1987.14 The F-LR transfusion programs were initiated next, followed by the F-LR/C-LR transfusion program, and, finally, standard rather than treated platelet transfusions were given as the initial transfusion to the last group of recipients. The number of recipient animals in each group was selected to provide enough data to demonstrate that the treatment given to the donor's platelets did or did not prevent platelet refractoriness, and, secondarily, whether tolerance was induced.
Most of the recipients that accepted the treated platelet preparation from their initial donor were then transfused with C-LR platelets from their initial donor for up to an additional 8 weeks or until they became refractory. C-LR transfusions were then given from third-party donor(s) (ie, dogs to whom the recipient had not been previously exposed to test for nonspecific tolerance). Even if the recipient did not accept the initial donor's platelets during the treatment phase, C-LR platelet transfusions from up to 2 third-party donors were still given. Dogs that accepted C-LR platelets from at least one third-party donor were considered nonspecifically tolerant to C-LR platelets. Finally, a single C-LR transfusion was given from the initial donor to determine if the recipient had developed refractoriness to this product following the third-party transfusions.
If the recipient was not refractory to the initial donor's C-LR platelets and had completed any planned third-party C-LR transfusions, the recipient was given STD transfusions from the initial donor and any third-party donors to whom they had not developed refractoriness, to further evaluate donor-specific and nonspecific tolerance, respectively. Some recipients were never given C-LR donor transfusions and were tested for tolerance only by giving STD platelet transfusions. If a recipient had not developed refractoriness to their initial donor's treated platelets, they were given standard platelets from this donor, and all recipients, whether or not they had accepted their initial donor's treated platelets, received STD platelets from third-party donors. After these third-party STD transfusions, a final STD transfusion from the initial donor was done to determine whether the recipient remained tolerant to this donor. Finally, autologous transfusions were done to determine whether the recipient dogs still had normal platelet recoveries and survivals.
If both C-LR and STD platelets from the same donor were transfused into the same recipient, it could be determined whether theirs was a differential effect on loss of tolerance depending on the type of WBCs transfused. The WBCs removed by filtration would be present in both types of platelets (C-LR and STD), whereas the WBCs removed by centrifugation would be present only in the STD platelets.
Statistical methods
Estimates of rates of acceptance and tolerance are based on the binomial distribution. The associated confidence intervals were also derived from the binomial distribution. Time to refractoriness to treated platelets from the initial donor was analyzed using the Cox proportional hazards model. Comparisons between treatments were based on Wald chi-square statistics from the Cox model. P values associated with these statistics were adjusted for multiple comparisons using the Bonferroni method. Descriptive statistics are presented for cell counts from each of the platelet preparations.
Results
Cell counts and viability of transfused platelets
The average number of platelets transfused was 1.2 × 109 to 1.9 × 109 (Table 1). The STD, C-LR, and F-LR(× 1) preparations tended to have more platelets per transfusion (1.7 × 109 to 1.9 × 109) than the F-LR(× 2) and F-LR/C-LR preparations (1.2 × 109 and 1.4 × 109, respectively; P = .03). The leukoreduced components contained an average of less than 3 × 103 to 7.9 × 104 WBCs/transfusion. Every leukoreduced component had no more than 2.5 × 106 WBCs/transfusion.
Cell counts of the transfused platelet components
. | . | Treated platelets . | . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
. | Standard platelets . | C-LR . | F-LR × 1† . | F-LR × 2‡ . | F-LR/C-LR . | γ-F-LR/C-LR . | ||||
| No. of observations | 138 | 248 | 54 | 20 | 147 | 48 | ||||
| No. of platelets injected, × 109 | 1.7 ± 0.8 | 1.9 ± 1.2 | 1.9 ± 0.9 | 1.2 ± 0.6 | 1.4 ± 1.0 | 1.4 ± 0.5 | ||||
| Range, × 109 | 0.6-5.8 | 0.4-7.1 | 0.6-4.4 | 0.3-2.5 | 0.2-5.9 | 0.5-2.3 | ||||
| No. of WBCs injected | 6.7 × 106 ± 5.4 × 106 | 4.7 × 104 ± 2.3 × 105 | 7.9 × 104 ± 2.8 × 105 | < 3 × 103* | < 3 × 103* | 3.6 × 103 ± 1.4 × 104 | ||||
| Range | 2.8 × 104-3.1 × 107 | < 3 × 103-2.5 × 106 | < 3 × 103-2.0 × 106 | < 3 × 103 | < 3 × 103-1.9 × 104 | < 3 × 103-6.9 × 104 | ||||
. | . | Treated platelets . | . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
. | Standard platelets . | C-LR . | F-LR × 1† . | F-LR × 2‡ . | F-LR/C-LR . | γ-F-LR/C-LR . | ||||
| No. of observations | 138 | 248 | 54 | 20 | 147 | 48 | ||||
| No. of platelets injected, × 109 | 1.7 ± 0.8 | 1.9 ± 1.2 | 1.9 ± 0.9 | 1.2 ± 0.6 | 1.4 ± 1.0 | 1.4 ± 0.5 | ||||
| Range, × 109 | 0.6-5.8 | 0.4-7.1 | 0.6-4.4 | 0.3-2.5 | 0.2-5.9 | 0.5-2.3 | ||||
| No. of WBCs injected | 6.7 × 106 ± 5.4 × 106 | 4.7 × 104 ± 2.3 × 105 | 7.9 × 104 ± 2.8 × 105 | < 3 × 103* | < 3 × 103* | 3.6 × 103 ± 1.4 × 104 | ||||
| Range | 2.8 × 104-3.1 × 107 | < 3 × 103-2.5 × 106 | < 3 × 103-2.0 × 106 | < 3 × 103 | < 3 × 103-1.9 × 104 | < 3 × 103-6.9 × 104 | ||||
Data are given as the average ± 1 SD.
The lower limit of WBC detection was < 3 × 10317
Platelets were filtered once with a single filter
Platelets were filtered twice with 2 filters
To determine the effects of the treatments on platelet viability, the first transfusion of the donor's treated platelets was compared with the recipient's autologous data (Table 2). The results of only the first transfusion of the donor's treated platelets were used to exclude any effects of immunization on the data. Recoveries of the treated donor platelets were significantly less than the autologous data for both the C-LR and F-LR× 1 platelets (P = .04 and P = .02, respectively), and survivals were significantly less for C-LR platelets, F-LR/C-LR platelets, and γ-irradiated F-LR/C-LR platelets (P < .01, P = .01, and P = .03, respectively). However, none of the treatments caused such abnormal platelet responses that the subsequent development of platelet refractoriness could not be determined.
Viability of standard and treated platelets
. | . | Treated platelets . | . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
. | Standard . | C-LR . | F-LR × 1* . | F-LR × 2† . | F-LR/C-LR . | γ-F-LR/C-LR . | ||||
| No. of observations | 7 | 39 | 8 | 5 | 19 | 6 | ||||
| Platelet recovery | ||||||||||
| Treated, donor, % | 26 ± 16 | 49 ± 19 | 36 ± 15 | 54 ± 4 | 54 ± 19 | 36 ± 13 | ||||
| Control, autologous, % | 27 ± 8 | 56 ± 13 | 53 ± 10 | 51 ± 10 | 55 ± 9 | 42 ± 9 | ||||
| P | .70 | .04 | .02 | .44 | .70 | .68 | ||||
| Platelet survivals | ||||||||||
| Treated, donor, d | 3.0 ± 1.6 | 2.7 ± 1.6 | 4.0 ± 1.6 | 4.1 ± 1.9 | 3.0 ± 1.3 | 2.4 ± 0.9 | ||||
| Control, autologous, d | 3.3 ± 1.1 | 4.0 ± 1.1 | 3.9 ± 0.4 | 3.8 ± 0.4 | 4.0 ± 0.9 | 3.7 ± 1.0 | ||||
| P | .41 | < .01 | .87 | .74 | .01 | .03 | ||||
. | . | Treated platelets . | . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
. | Standard . | C-LR . | F-LR × 1* . | F-LR × 2† . | F-LR/C-LR . | γ-F-LR/C-LR . | ||||
| No. of observations | 7 | 39 | 8 | 5 | 19 | 6 | ||||
| Platelet recovery | ||||||||||
| Treated, donor, % | 26 ± 16 | 49 ± 19 | 36 ± 15 | 54 ± 4 | 54 ± 19 | 36 ± 13 | ||||
| Control, autologous, % | 27 ± 8 | 56 ± 13 | 53 ± 10 | 51 ± 10 | 55 ± 9 | 42 ± 9 | ||||
| P | .70 | .04 | .02 | .44 | .70 | .68 | ||||
| Platelet survivals | ||||||||||
| Treated, donor, d | 3.0 ± 1.6 | 2.7 ± 1.6 | 4.0 ± 1.6 | 4.1 ± 1.9 | 3.0 ± 1.3 | 2.4 ± 0.9 | ||||
| Control, autologous, d | 3.3 ± 1.1 | 4.0 ± 1.1 | 3.9 ± 0.4 | 3.8 ± 0.4 | 4.0 ± 0.9 | 3.7 ± 1.0 | ||||
| P | .41 | < .01 | .87 | .74 | .01 | .03 | ||||
Overall, autologous radiolabeled platelet recoveries and survivals in 73 normal dogs averaged 53% ± 12% and 4.1 ± 0.8 days, respectively (±1 SD). Data are given as average ±1 SD. P values are for paired t statistic comparing baseline autologous data for each dog compared with their first treated donor transfusion.
Treated indicates data from the first standard (if recipient was in the standard initial donor group) or treated donor platelet transfusion given to a recipient; and Control, data from the 2 baseline autologous platelet transfusions of the recipient animals.
Platelets were filtered once with a single filter
Platelets were filtered twice with 2 filters
Acceptance of donor platelets
Data on the number of dogs who accepted the treated platelets of their initial donor are given in Table 3, and time to refractoriness is shown in Figure 2.
Acceptance of donor platelets and induction of tolerance
. | . | Specific tolerance . | . | Nonspecific tolerance . | . | ||
|---|---|---|---|---|---|---|---|
| Initial donor platelet modification . | Acceptance of initial donor's treated platelets . | Initial donor, C-LR platelets . | Initial donor, STD platelets . | Third-party donors,*C-LR platelets . | Third-party donors,*STD platelets . | ||
| None, STD platelets, no. accepting/no. recipients (%) | 1/7 (14) | ND | ND | ND | 0/5 (0) | ||
| Range, % | 0-58 | NA | NA | NA | 0-45 | ||
| Single-treatment programs | |||||||
| C-LR, no. accepting/no. recipients (%) | 3/21 (14) | 1/3 (33) | ND | ND | ND | ||
| Range, % | 3-36 | 1-91 | NA | NA | NA | ||
| F-LR | |||||||
| Filtered × 1, no. accepting/no. recipients (%) | 3/8 (38) | 2/3 (67) | ND | 2/8 (25) | ND | ||
| Filtered × 2, no. accepting/no. recipients (%) | 1/5 (20) | 1/1 (100) | ND | 1/5 (20) | ND | ||
| Total, no. accepting/no. recipients (%) | 4/13 (31) | 3/4 (75) | ND | 3/13 (23) | ND | ||
| Range, % | 9-61 | 19-99 | NA | 5-54 | NA | ||
| Combined-treatment programs | |||||||
| F-LR/C-LR, no. accepting/no. recipients (%) | 13/15 (87) | 10/10 (100) | 7/9 (78) | 10/11 (91) | 3/8 (38) | ||
| Range, % | 60-98 | 74-100 | 40-97 | 59-100 | 8-75 | ||
| F-LR/C-LR + plasma, no. accepting/no. recipients (%) | 4/4 (100) | 4/4 (100) | 4/4 (100) | 4/4 (100) | 2/4 (50) | ||
| Range, % | 47-100 | 47-100 | 47-100 | 47-100 | 7-93 | ||
| F-LR/C-LR + RBC, no. accepting/no. recipients (%) | 4/4 (100) | 3/4 (75) | 3/4 (75) | 3/4 (75) | 2/2 (100) | ||
| Range, % | 47-100 | 19-99 | 19-99 | 19-99 | 72-100 | ||
| Total F-LR/C-LR, non-γ, no. accepting/no. recipients (%) | 21/23 (91) | 17/18 (94) | 14/17 (82) | 17/19 (89) | 7/14 (50) | ||
| Range, % | 72-99 | 73-99 | 57-96 | 67-99 | 23-77 | ||
| γ-F-LR/C-LR, no. accepting/no. recipients (%) | 6/6 (100) | ND | 0/6 (0) | ND | 1/6 (17) | ||
| Range, % | 61-100 | NA | 0-39 | NA | 4-64 | ||
. | . | Specific tolerance . | . | Nonspecific tolerance . | . | ||
|---|---|---|---|---|---|---|---|
| Initial donor platelet modification . | Acceptance of initial donor's treated platelets . | Initial donor, C-LR platelets . | Initial donor, STD platelets . | Third-party donors,*C-LR platelets . | Third-party donors,*STD platelets . | ||
| None, STD platelets, no. accepting/no. recipients (%) | 1/7 (14) | ND | ND | ND | 0/5 (0) | ||
| Range, % | 0-58 | NA | NA | NA | 0-45 | ||
| Single-treatment programs | |||||||
| C-LR, no. accepting/no. recipients (%) | 3/21 (14) | 1/3 (33) | ND | ND | ND | ||
| Range, % | 3-36 | 1-91 | NA | NA | NA | ||
| F-LR | |||||||
| Filtered × 1, no. accepting/no. recipients (%) | 3/8 (38) | 2/3 (67) | ND | 2/8 (25) | ND | ||
| Filtered × 2, no. accepting/no. recipients (%) | 1/5 (20) | 1/1 (100) | ND | 1/5 (20) | ND | ||
| Total, no. accepting/no. recipients (%) | 4/13 (31) | 3/4 (75) | ND | 3/13 (23) | ND | ||
| Range, % | 9-61 | 19-99 | NA | 5-54 | NA | ||
| Combined-treatment programs | |||||||
| F-LR/C-LR, no. accepting/no. recipients (%) | 13/15 (87) | 10/10 (100) | 7/9 (78) | 10/11 (91) | 3/8 (38) | ||
| Range, % | 60-98 | 74-100 | 40-97 | 59-100 | 8-75 | ||
| F-LR/C-LR + plasma, no. accepting/no. recipients (%) | 4/4 (100) | 4/4 (100) | 4/4 (100) | 4/4 (100) | 2/4 (50) | ||
| Range, % | 47-100 | 47-100 | 47-100 | 47-100 | 7-93 | ||
| F-LR/C-LR + RBC, no. accepting/no. recipients (%) | 4/4 (100) | 3/4 (75) | 3/4 (75) | 3/4 (75) | 2/2 (100) | ||
| Range, % | 47-100 | 19-99 | 19-99 | 19-99 | 72-100 | ||
| Total F-LR/C-LR, non-γ, no. accepting/no. recipients (%) | 21/23 (91) | 17/18 (94) | 14/17 (82) | 17/19 (89) | 7/14 (50) | ||
| Range, % | 72-99 | 73-99 | 57-96 | 67-99 | 23-77 | ||
| γ-F-LR/C-LR, no. accepting/no. recipients (%) | 6/6 (100) | ND | 0/6 (0) | ND | 1/6 (17) | ||
| Range, % | 61-100 | NA | 0-39 | NA | 4-64 | ||
Data are presented as the acceptance rate: (no. accepting/no. recipients) × 100 and the 95% confidence intervals for the acceptance ratios are shown in parentheses. If the confidence intervals do not overlap for the comparison of interest, it can be assumed that the percentages differ by at least P ≤ .05.
ND indicates not determined; NA, not applicable.
Results in columns labeled “Third-party donors” give the acceptance rates based on the number of recipients who accepted platelets from at least one of their third-party donors
Time to refractoriness of the initial donor's platelets. Time to refractoriness expressed as a percentage of the recipients who continued to accept STD or treated platelets from their initial donors is shown. The recipient dogs are categorized by the type of platelets they received (ie, both filter and centrifuge leukoreduced [F-LR/C-LR], γ-irradiation with F-LR/C-LR [γ-F-LR/C-LR], filter leukoreduced using 1 or 2 filters [F-LR], centrifuge leukoreduced [C-LR], or standard [STD] platelets). The transfusion week is given on the abscissa and the percentage of accepting recipients remaining in each group on the ordinate. P values for the comparison of each group to the STD group were F-LR/C-LR, P = .001; γ-F-LR/C-LR, P = .004; FL, P = .86; and C-LR, P = .21. Because of multiple comparisons, a P value of .01 or less was considered significant.
Time to refractoriness of the initial donor's platelets. Time to refractoriness expressed as a percentage of the recipients who continued to accept STD or treated platelets from their initial donors is shown. The recipient dogs are categorized by the type of platelets they received (ie, both filter and centrifuge leukoreduced [F-LR/C-LR], γ-irradiation with F-LR/C-LR [γ-F-LR/C-LR], filter leukoreduced using 1 or 2 filters [F-LR], centrifuge leukoreduced [C-LR], or standard [STD] platelets). The transfusion week is given on the abscissa and the percentage of accepting recipients remaining in each group on the ordinate. P values for the comparison of each group to the STD group were F-LR/C-LR, P = .001; γ-F-LR/C-LR, P = .004; FL, P = .86; and C-LR, P = .21. Because of multiple comparisons, a P value of .01 or less was considered significant.
Standard platelet transfusions (control group)
Only 1 of 7 recipients given STD platelet transfusions from their initial donor accepted these transfusions, and none of the 5 recipients tested accepted STD platelets from a third-party donor (Table 3). Median time to platelet refractoriness was 5 weeks (range, 1-8 weeks; Figure 2). Platelet recoveries averaged 40% ± 17% and survivals 2.0 ± 1.2 days for all the donor transfusions given prior to the onset of platelet refractoriness.
Single-treatment programs
Data from a previous study14 showed that only 14% of the dogs (n = 21) who received C-LR platelets accepted them. The acceptance rates for recipients given once-filtered (38%; n = 8) or twice-filtered platelets (20%; n = 5) were not significantly different nor were the results in the direction expected (Table 3). Because there were no differences in the transfusion outcomes for the dogs transfused with filtered platelets, the results were combined, giving a F-LR acceptance rate of 31% (n = 13). Overall, only 7 (21%) of 34 of the recipients accepted C-LR or F-LR platelets. There were no differences in acceptance rates among the single-treatment or STD platelet recipients and also no difference among these recipients in time to onset of platelet refractoriness (ie, median time to refractoriness was 2 weeks [range, 1-8 weeks] for the C-LR recipients and 4 weeks [range, 1-8 weeks] for the F-LR recipients; Figure 2). Prior to the development of platelet refractoriness, average platelet recoveries were 56% ± 11% and 39% ± 16%, and survivals were 2.8 ± 1.1 and 3.1 ± 2.2 days for all C-LR and F-LR donor transfusions, respectively (no significant difference among STD, C-LR, or F-LR transfusions).
Combined-treatment programs
Among the combined-treatment programs, 87% of the F-LR/C-LR recipients (n = 15) and 100% of the γ–F-LR/C-LR (n = 6) recipients accepted their initial donor's treated platelet transfusions (Table 3). To ensure that these results were specifically related to WBC removal and not to the removal of plasma or RBCs that also occurred during the processing steps, F-LR/C-LR plasma and F-LR/C-LR washed RBCs were added back to F-LR/C-LR platelets from the same donor. The addition of neither F-LR/C-LR plasma (n = 4) nor F-LR/C-LR washed RBCs (n = 4) to F-LR/C-LR platelets changed the acceptance rates of the F-LR/C-LR platelets (100% acceptance). Grouping the data from all these F-LR/C-LR recipients, the acceptance rate was 93% (n = 29; P ≤ .05 compared with STD, C-LR, or F-LR platelets). Times to platelet refractoriness for recipients given F-LR/C-LR or γ–F-LR/C-LR platelets versus STD platelets were statistically different (P < .001 and P = .004, respectively; Figure 2).
For all the donor transfusions given prior to the onset of platelet refractoriness, platelet recoveries averaged 47% ± 16% and 55% ± 13%, and platelet survivals averaged 2.6 ± 1.0 days and 2.6 ± 0.9 days for F-LR/C-LR and γ–F-LR/C-LR transfusions, respectively (no significant difference compared with STD, C-LR, or F-LR transfusions).
Tolerance induction to platelets
Specific tolerance. For recipients who had not become refractory to treated platelet transfusions from their initial donor, most received C-LR platelet transfusions from these same donors. And, for the recipients of F-LR or F-LR/C-LR, these C-LR platelets were well tolerated (ie, 75% and 94% of these recipients, respectively, remained platelet responsive). Overall, among the 22 initially nonrefractory recipients tested in the F-LR and F-LR/C-LR groups, 20 (91%) remained responsive to their initial donor's C-LR platelets. This is in contrast to the dogs in the C-LR arm, all of whom were exposed to C-LR platelets from their initial donor without “prior conditioning.” Only 3 (14%) of 21 remained platelet responsive to their initial donor's treated transfusions during the first 8 weeks of C-LR transfusions and when the 3 remaining recipients were given an additional 8 weeks of C-LR platelets from their initial donor, only 1 remained nonrefractory (P = .001). This suggests that, under ordinary circumstances, C-LR transfusions are very immunogenic.
STD platelet transfusions from their initial donors were only given to some of the nonrefractory recipients of the combined-treatment programs. Of the animals that had previously received F-LR/C-LR platelets, 82% of the recipients (n = 17) remained responsive to STD platelets from their initial donor. However, if the initial donor's F-LR/C-LR platelets were also γ-irradiated prior to transfusion, tolerance was not induced to STD platelets from any of the initial donors even though the donor's γ-irradiated F-LR/C-LR platelets were accepted (P < .01 compared with STD transfusions given to recipients of non–γ-irradiated F-LR/C-LR platelets).
Nonspecific tolerance. Excluding the C-LR recipients who received transfusions only from their initial donor, all of the other recipients received either C-LR, STD, or both C-LR and STD platelets from other donors (ie, so-called “third party” donors). Most of the recipients (30/31; 97%) received C-LR platelets from 2 other donors. If they remained responsive to platelets from at least one of these donors, they were considered as accepting that product. Acceptance of C-LR platelets from third-party donors varied widely from only 23% of the recipients (n = 18) of F-LR platelets to 89% of the recipients (n = 19) of F-LR/C-LR platelets (P < .05; Table 3).
Among the 20 animals who were tolerant to both treated and C-LR platelet transfusions from their initial donor, only 4 (20%) became refractory to C-LR platelets from at least one third-party donor (3 were refractory to 1 donor [75%] and 1 to 2 donors [25%]). In contrast, of the 11 dogs who became refractory to their initial donor's either treated or C-LR platelets, all (100%) became refractory to C-LR platelets from at least one third-party donor (P < .01; 1 was refractory to 1 of 2 donors [9%] and 10 were refractory to both donors [91%]).
Of the recipients who received STD platelets from third-party donors, 16 (84%) of 19 received platelets from 2 donors. The STD platelets from third-party donors were not tolerated nearly as well as the C-LR platelets from third-party donors. Only 7 (50%) of 14 recipients of F-LR/C-LR platelets accepted STD platelets from at least one of their third-party donors (Table 3). Three recipients accepted platelets from both donors and 4 accepted platelets from 1 donor. Again, γ-irradiation of the initial donor's F-LR/C-LR platelets essentially eliminated tolerance to STD platelets from third-party donors (ie, only 1/6 recipients [17%] accepted platelets from 1 of the 11 third-party donors tested; P = .32 compared with recipients of F-LR/C-LR non–γ-irradiated platelets).
Refractoriness to transfused platelets from an earlier donor predicted a recipient's response to platelets from a later donor, (ie, 27/31 [87%] recipients continued to “reject” platelets from all later donors). At the end of the study period, previous recipients who had accepted donor platelets were retransfused to determine whether refractoriness to a later donor's platelets had induced refractoriness to an earlier donor's tolerated platelets. Of 18 informative pairs who had accepted some but not all donors, 7 recipients (39%) had become refractory to a previously tolerated donor. In contrast, of 7 recipients who tolerated platelets from all of their donors, only 1 recipient (14%) showed refractoriness to platelets from a previously accepted donor.
All end-of-study autologous platelet recovery and survival measurements gave results comparable to each recipient dog's pretransfusion (baseline) autologous platelet studies (data not shown). This suggests that all refractoriness to donor platelets was immune mediated regardless of whether antibodies were detected. If platelet refractoriness was related to some intercurrent condition, it would have adversely effected the recipient's response to both autologous as well as allogeneic platelets.
Development of platelet alloantibodies
Weekly serum samples were available for antibody testing against donor platelets from a variable number of recipients (Table 4). Antibody results were positive with platelets or lymphocytes from all 14 donors whose platelets were not accepted (100%) and from only 5 (23%) of 22 of donors whose platelets were accepted (P = .04).
Development of alloantibodies to the initial donor's platelets and/or lymphocytes
. | No. antibody-positive/no. tested . | . | |
|---|---|---|---|
| Transfusion group . | Refractory recipients . | Accepting recipients . | |
| Standard | 6/6 | — | |
| Single treatment | |||
| F-LR × 1 | 2/2 | 2/2 | |
| F-LR × 2 | 4/4 | 0/1 | |
| Combined treatment | |||
| F-LR/C-LR | 2/2 | 3/13 | |
| γ-F-LR/C-LR | — | 0/6 | |
. | No. antibody-positive/no. tested . | . | |
|---|---|---|---|
| Transfusion group . | Refractory recipients . | Accepting recipients . | |
| Standard | 6/6 | — | |
| Single treatment | |||
| F-LR × 1 | 2/2 | 2/2 | |
| F-LR × 2 | 4/4 | 0/1 | |
| Combined treatment | |||
| F-LR/C-LR | 2/2 | 3/13 | |
| γ-F-LR/C-LR | — | 0/6 | |
Results are reported for dogs who had all 3 antibody tests run with the initial donor's platelets and lymphocytes. A positive result indicates that the recipient serum reacted with the donor's platelets and/or lymphocytes in at least 1 assay with 2 sequential weekly serum samples.
— indicates not applicable.
Tolerance induction to skin grafts
Skin grafts were performed in a few of the recipients given F-LR/C-LR platelets to determine if acceptance of treated platelet transfusions might permit engraftment. Of the 7 recipients tested, 5 had 2 allografts, and 2 had 1. Four recipients accepted a skin graft (57%; Table 5). Three recipients accepted a skin graft from their initial donor and rejected a third-party graft, whereas the fourth rejected their initial donor's graft but accepted a third-party graft. There were a total of 10 allografts from donors whose STD platelets from either the initial or third-party donors had been accepted by the recipient, and only 4 allografts were accepted (40%). Thus, just accepting STD platelets is not the only factor governing successful engraftment.
Skin graft studies
. | . | . | . | . | . | . | . | . | Skin grafts . | . | . | . | . | . | . | . | . | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Pretransplantation donor platelet transfusions . | . | . | . | . | . | . | . | . | Third-party donors . | . | Posttransplantation donor platelet transfusions . | . | . | . | . | . | |||||||||||||
| Recipient dog no. . | Initial donor's F-LR/C-LR platelets . | . | Initial donor, standard . | . | Second donor, standard . | . | Third donor, standard . | . | Initial donor . | Second donor . | Third donor . | Initial donor, standard . | . | Second donor, standard . | . | Third donor, standard . | . | |||||||||||||
| E652 | A | – | A | – | A | – | A | – | A | ND | R | A | + | A | + | R | + | |||||||||||||
| E281 | A | – | A | – | A | – | A | – | A | ND | R | A | + | A | + | A | + | |||||||||||||
| E238 | A | – | A | – | R | – | R | – | A | R | ND | A | – | ND | + | R | + | |||||||||||||
| E181 | A | – | A | – | A | – | A | – | R | A | ND | A | – | A | + | A | + | |||||||||||||
| E368 | A | – | ND | ND | ND | ND | ND | ND | R | ND | ND | R | + | ND | ND | ND | ND | |||||||||||||
| E308 | A | ND | A | + | A | – | R | – | ND | R | ND | A | + | A | + | A | + | |||||||||||||
| E106 | A | ND | A | – | R | – | A | – | R | ND | R | A | + | ND | ND | R | + | |||||||||||||
. | . | . | . | . | . | . | . | . | Skin grafts . | . | . | . | . | . | . | . | . | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Pretransplantation donor platelet transfusions . | . | . | . | . | . | . | . | . | Third-party donors . | . | Posttransplantation donor platelet transfusions . | . | . | . | . | . | |||||||||||||
| Recipient dog no. . | Initial donor's F-LR/C-LR platelets . | . | Initial donor, standard . | . | Second donor, standard . | . | Third donor, standard . | . | Initial donor . | Second donor . | Third donor . | Initial donor, standard . | . | Second donor, standard . | . | Third donor, standard . | . | |||||||||||||
| E652 | A | – | A | – | A | – | A | – | A | ND | R | A | + | A | + | R | + | |||||||||||||
| E281 | A | – | A | – | A | – | A | – | A | ND | R | A | + | A | + | A | + | |||||||||||||
| E238 | A | – | A | – | R | – | R | – | A | R | ND | A | – | ND | + | R | + | |||||||||||||
| E181 | A | – | A | – | A | – | A | – | R | A | ND | A | – | A | + | A | + | |||||||||||||
| E368 | A | – | ND | ND | ND | ND | ND | ND | R | ND | ND | R | + | ND | ND | ND | ND | |||||||||||||
| E308 | A | ND | A | + | A | – | R | – | ND | R | ND | A | + | A | + | A | + | |||||||||||||
| E106 | A | ND | A | – | R | – | A | – | R | ND | R | A | + | ND | ND | R | + | |||||||||||||
A indicates accepted; ND, not done; and R, rejected.
For platelet transfusions, the recipient accepted 8 weeks of transfusions either from their initial donor (first donor) or third-party donors (second or third donor in order received). For the skin grafts, the recipient accepted a graft from either their initial or one of their third-party donors (second or third donor). For platelet transfusions, the recipient rejected either platelets from their initial donor or third-party donors (second or third donor). For the skin grafts, the recipient rejected a graft from either their initial or one of their third-party donors (second or third donor). The results of lymphocytotoxic antibody cross-match tests using recipient serum and donor lymphocytes is given as positive (+) or negative (–) beside the results of the corresponding platelet transfusion. The serum used for testing was drawn during the week the platelet survival studies were done.
Four to 8 weeks after skin grafting, repeat platelet survivals were performed from 11 donors whose STD platelets had been previously accepted by the recipient. Platelets were accepted after grafting not only from the 4 donors whose skin grafts were accepted but also from 4 (57%) of 7 donors whose skin grafts were rejected.
After grafting, the lymphocyte antibody test became positive with 6 (86%) of 7 donors whose grafts were rejected, but the test was also positive with 3 (75%) of 4 donors whose grafts were accepted. Similarly, antibody positivity did not predict platelet responses after grafting (ie, the lymphocyte cross-match test was positive with all 3 refractory donors [100%], but it was also positive with 6/8 nonrefractory donors [75%]).
Discussion
The most important study findings were the effects of the different methods of leukoreduction and γ-irradiation on acceptance of donor platelets. In a normal immunocompetent recipient, centrifuge leukoreduction (C-LR) or filtration leukoreduction (F-LR), in spite of reducing the average level of contaminating leukocytes to 4.7 × 104 to 7.9 × 104 total WBCs/transfusion, respectively, prevented alloimmune platelet refractoriness in only 14% and 38% of the transfused recipients. These results do not differ from those observed with the transfusion of standard (STD) unmodified donor platelets (ie, 1/7 recipients [14%] accepted donor platelets). The levels of leukocyte reduction achieved were well below the level of less than 5.0 × 106 leukocytes/transfusion considered to prevent alloimmunization in humans.20 The dogs given leukoreduced platelets received 4.7 × 103 to 7.9 × 103 WBCs/kg, whereas a 70-kg man would receive 7.1 × 104 WBCs/kg with a transfusion containing 5 × 106 WBCs (ie, dogs received a log less WBCs/kg). In addition, the leukoreduction was done at the time of blood drawing, which prior rabbit platelet transfusion experiments had suggested was important to prevent immunization.21 Even when the platelets were filtered twice to further reduce the level of the contaminating WBCs to less than 3 × 103 total WBCs/transfusion (at the lower limit of detection of the assay), the level of protection was not improved (ie, only 20% of the recipients [n = 5] receiving platelets filtered twice accepted donor platelets compared with an acceptance rate of 38% in recipients who received platelets filtered only once [n = 8]). These data suggest that just making a quantitative reduction in the level of the contaminating leukocytes does not prevent alloimmune platelet refractoriness. In fact, data in a mouse transfusion model suggests that extremely leukoreduced platelet transfusions are more immunogenic then when some residual WBCs are transfused along with the platelets.22
Surprisingly, combining the 2 methods of leukoreduction (F-LR and C-LR) produced the best results (ie, 87% of the recipients [n = 15] accepted F-LR/C-LR donor platelets; P < .05 compared with C-LR, F-LR, or STD platelet transfusions). Furthermore, add-back experiments demonstrated that neither F-LR/C-LR plasma nor F-LR/C-LR washed red cells were immunogenic, suggesting that the results achieved with F-LR/C-LR platelets were related to leukocyte removal rather than the elimination of contaminating plasma or red cells during platelet preparation. Acceptance of F-LR/C-LR platelets using all these results was 91% (n = 23). These studies are in conflict with prior rabbit platelet transfusion studies that suggested that soluble leukocyte antigens present in plasma are immunogenic.21
These data suggest that there is a qualitative difference in the WBC populations removed by the 2 leukocyte-reduction techniques and imply the presence of at least 2 populations of allostimulatory cells in platelet transfusions. One of these allostimulatory cell populations is a filter-adherent cell, perhaps in the lymphocyte and/or monocyte populations, both of which are removed by filtration,23 whereas the other population may consist of dense, nonadherent cells that can be removed by centrifugation. A candidate for this second cell type would be dendritic precursors,24 known to be allostimulatory and present in very low quantities in peripheral blood. Only when both of these populations of WBCs are removed is a nonimmunogenic platelet preparation achieved. We may have, by chance, arrived at an optimal type and concentration of residual white cells that prevent alloimmunization as has been previously suggested by Semple et al.22 Currently, studies are being performed to characterize the cells that are removed or remain after each of the preparative steps and these results will be reported when completed.
Significantly, not only did the F-LR/C-LR platelets prevent alloimmune platelet refractoriness but they also induced tolerance to donor platelets and skin grafts. Following the F-LR/C-LR platelet transfusions, 2 different types of donor platelets were transfused to test for tolerance induction: C-LR platelets and STD platelets from both the initial and third-party platelet donors. The former platelets contained only the cells that would ordinarily be removed by filtration, whereas the latter contained both types of WBCs. Two observations are of note: (1) F-LR/C-LR recipients accepted C-LR platelets from both the initial donor as well as third-party donors (94% and 89% acceptance, respectively) at higher rates than STD platelets from the same donors (82% and 50% acceptance, respectively); and (2) not unexpectedly, acceptance rates were higher for platelets from the initial donor than from third-party donors (ie, specific tolerance rates were better than nonspecific rates). These studies also suggest that, after the treated transfusions, the cell that is removed by filtration is often accepted, whereas the cell that is removed by centrifugation is more likely to “break” tolerance.
Of the 7 F-LR/C-LR recipients tested, 4 (57%) accepted at least one skin graft from an allogeneic donor (3 from the initial platelet donor and 1 from a third-party donor). We postulated that acceptance of STD platelets from a donor might predict the acceptance of that donor's skin graft. Although STD platelets from 10 donors were accepted, skin grafts from only 4 of these donors were accepted (40%), suggesting that there are other factors involved in accepting skin grafts. This is reinforced by the observation that STD donor platelets were still accepted following skin graft rejection by 4 (57%) of the 7 recipients. Possibly fortuitous histocompatibility matching between donors and recipients may have influenced not only the acceptance of STD platelets but also skin grafts from some but not all donors. As skin grafts are very immunogenic, these data may suggest that prior transfusions of F-LR/C-LR platelets to recipients awaiting organ grafts may facilitate engraftment.
To further evaluate the mechanisms of tolerance induction by F-LR/C-LR platelets, 6 recipients received F-LR/C-LR donor platelets that had also been γ-irradiated. Although all these recipients accepted the F-LR/C-LR γ-irradiated platelets (100%) similar to the 91% acceptance rate for F-LR/C-LR platelets, none of these recipients accepted STD platelets from their initial donor and only one accepted STD platelets from a third-party donor (P < .01 and P = .32, respectively, compared with STD platelet transfusions given to recipients of F-LR/C-LR platelets). These data suggest that, following F-LR/C-LR, there remains a residual white cell that induces tolerance and that the function of this white cell is abrogated by γ-irradiation. Thus, in order for tolerance to occur, a white cell capable of dividing must be transfused (ie, microchimerism has occurred). It may be that Semple et al22 inadvertently removed the tolerance-inducing cell when they produced an extremely leukoreduced product.
Antibody assays were positive with either platelets, lymphocytes, or both from all 14 tested recipients who became refractory to their initial donors (100%) and with only 5 (21%) of 24 of donors they accepted. Thus, there was a direct correlation between antibody positivity and platelet refractoriness (P = .04). However, regardless of the results of the antibody tests, platelet refractoriness in this study was assumed to be alloimmune as these were normal dogs on no medications, they were clinically well, and their autologous platelet recoveries and survivals were all within the normal range both before and after study, suggesting that nonimmune mechanisms of platelet refractoriness were not present in these recipient dogs.
Of interest, lymphocytotoxic antibody tests did not predict the results of skin grafting or donor platelet survival measurements after grafting. All 7 of the skin graft recipients were lymphocytotoxic antibody negative before grafting with their 12 skin graft donors. As expected after grafting, lymphocytotoxic antibody tests became positive with 5 (83%) of 6 donors whose skin grafts were rejected. However, they were also positive with 3 (75%) of 4 of the recipients whose skin grafts were accepted. Similarly, the lymphocytotoxic antibody test was positive with the 3 donors whose STD platelets were rejected after grafting (100%), but the test was also positive with 6 (75%) of 8 donors whose STD platelets were accepted after grafting.
Although it can never be assumed that studies performed in an animal model can be transferred to man, there is data to suggest that, for bone marrow transplantation studies25,26 and potentially also for platelet transfusion studies,14,15 the dog may serve as a good preclinical model. However, it could be argued that the dog studies do not predict outcomes in man because filtration leukoreduction was not nearly as effective in the dog as it has been in patients.1 However, leukoreduction may have been more successful in patients because they were receiving high doses of potentially immunosuppressive chemotherapy while they were being transfused as opposed to the dogs who had a normal immune system. Certainly, in prior studies, patients receiving chemotherapy had much lower rates of antibody formation compared with patients with aplastic anemia.27 It is possible that F-LR/C-LR platelets may prevent alloimmune platelet refractoriness in all patients regardless of the status of their immune system. In addition, the tolerance induction studies may lend insight into the so-called immunomodulatory effects of transfusion28 and may suggest that specific types of transfusions may be needed, depending on the desired clinical outcome. For example, kidney transplant recipients might benefit from F-LR/C-LR platelet transfusions that could lead to tolerance induction without inducing immunization, whereas surgery patients who received a transfusion who may have higher rates of postoperation infection or tumor recurrences might benefit from γ-irradiated transfusions to prevent immunomodulation.
Prepublished online as Blood First Edition Paper, July 1, 2004; DOI 10.1182/blood-2003-08-2942.
Supported by grants from the National Heart, Lung and Blood Institute, National Institutes of Health (RO1 HL47227); the Haemonetics Corporation, Braintree, MA; the Boeing Corporation, Seattle, WA; Pat's Fund, Seattle, WA; and the Leukemia and Lymphoma Society (6147-02). D.F. was supported by a grant from the Fonds de la Recherche en Santé du Québec, Montréal, Québec, Canada.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors are indebted to Ginny Knight and Leta Stever for administrative and secretarial assistance.

![Figure 2. Time to refractoriness of the initial donor's platelets. Time to refractoriness expressed as a percentage of the recipients who continued to accept STD or treated platelets from their initial donors is shown. The recipient dogs are categorized by the type of platelets they received (ie, both filter and centrifuge leukoreduced [F-LR/C-LR], γ-irradiation with F-LR/C-LR [γ-F-LR/C-LR], filter leukoreduced using 1 or 2 filters [F-LR], centrifuge leukoreduced [C-LR], or standard [STD] platelets). The transfusion week is given on the abscissa and the percentage of accepting recipients remaining in each group on the ordinate. P values for the comparison of each group to the STD group were F-LR/C-LR, P = .001; γ-F-LR/C-LR, P = .004; FL, P = .86; and C-LR, P = .21. Because of multiple comparisons, a P value of .01 or less was considered significant.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/105/2/10.1182_blood-2003-08-2942/6/m_zh80020572620002.jpeg?Expires=1767734821&Signature=4-M7mqBHuxuChDkh0od55jqYp~b0cWXaAcEEx08C2XP7DhMlFXcuEZpwsv4wFob7xwHeyzDC9GejCWKPE2l1LdGElylIa3j7juv4TrGymiNChom6KjbV26GGwJxiJKVsqfk~3oO1hqmJeagXvFMG6lNnTgwG6fB~HEvnFYNPL~Wol-u6LQ1EvoxI5BlpTAYNkP6nynjIx66AKAA3clmTdp-FOcLfz3DZFUQGzDbOazdPqY0ui8U6XV5spVvANFCpTl9qJJpWwIA46Lf7ZchtVqtfVfhiORD6hP60it95oy2IZkv~vPghcCWIWptyCoTpYMr~M-AmXYNxfurHUsUzHw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal