A collaborative study has shown that allogeneic stem cell transplantation offers the best chance for long-term survival when offered at diagnosis for patients with the highest-risk disease but should be delayed to a later time for patients, particularly younger ones, in lower-risk groups.
When the best therapy for a condition is also the most dangerous, assistance is required in determining the optimal timing of that treatment. The first paper clearly showing that allogeneic bone marrow transplantation (BMT) was curative therapy for myelodysplastic syndromes (MDSs) was published in 19841 and subsequent studies have confirmed this observation. In this issue of Blood, Cutler and colleagues (page 579) tell us that in order to maximize survival, HLA-matched sibling donor allogeneic BMT is best performed at diagnosis for patients in the highest-risk groups, based on the International Prognosis Scoring System (IPSS), and delayed to a time prior to leukemic transformation for those with lesser IPSS scores. For the younger patients in the study, the effect of delay was even more noticeable. These decisions are important, especially in a condition where improvements in the understanding of clinical and biologic prognostic factors have improved the overall selection of therapies, curative and palliative.2 FIG1
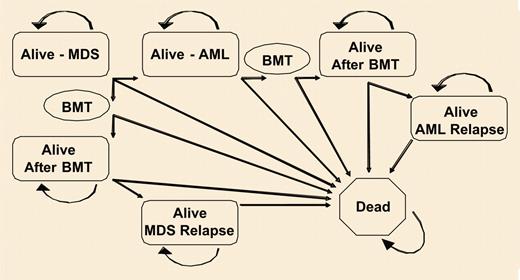
Markov decision model. See the complete figure in the article beginning on page 579.
Markov decision model. See the complete figure in the article beginning on page 579.
The Markov approach to decision analysis has been used to define prognosis for particular patient groups dependent on clinical scenarios for over 20 years.3 “Patients and methods” of Cutler et al's paper describes this sophisticated statistical technique in terms readily understandable by the hematologist. In this study, the process looked at the movement of patients between various states of health (alive, dead, before and after BMT, with MDS, with acute myelogenous leukemia [AML]) and adjusted outcome probabilities as these transitions were made.
The potential for new therapies that, while not curative, may modify the natural history of and improve the quality of life for patients with MDS, along with changes in the clinical practice of BMT, means that the results of these types of studies become essential aids to clinical decision making. That prospectively collected data from disparate centers and research groups can be brought together to perform these studies is encouraging and engenders optimism that the correct answers to difficult clinical questions in the field of BMT and myeloid malignancies can be obtained in the most reliable way.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal