To determine whether combined modality therapy (CMT) is superior to chemotherapy (CT) alone, 152 untreated Hodgkin disease patients with clinical stages (CSs) IA, IB, IIA, IIB, and IIIA without bulk disease were prospectively randomized to 6 cycles of doxorubicin, bleomycin, vinblastine, dacarbazine (ABVD) alone or 6 cycles of ABVD followed by radiation therapy (RT) (3600 cGy: involved field for 11 patients, modified extended field for the rest). Of 76 patients randomized to receive RT, 65 actually received it, and 11 did not (4 progressed, 1 had bleomycin toxicity, 6 refused). For ABVD + RT, the complete remission (CR) percentage was 94% and no major response, 6%. For ABVD alone, 94% achieved a CR; 1.5%, a partial response (PR); and 4.5%, no major response. At 60 months CR duration, freedom from progression (FFP), and overall survival (OS) for ABVD + RT versus ABVD alone are 91% versus 87% (P = .61), 86% versus 81% (P = .61), and 97% versus 90% (P = .08), respectively (log-rank). The 95% confidence intervals for CR duration, FFP, and OS differences at 5 years were –8% to 15%, –8% to 18%, and –4% to 12%, respectively. Although significant differences were not seen, it is possible that a benefit in outcome of less than 20% for CMT might be seen in a larger trial.
Introduction
The optimal treatment of early-stage Hodgkin disease has been controversial because of the success of several approaches. These include extended field (EF) radiation therapy (RT) in surgically staged1,2 and even clinically staged patients,3 combinations of chemotherapy and RT (combined modality therapy, CMT),4-7 and chemotherapy alone.8,9 Disease-free survival with EF RT in surgically staged IA and IIA patients has varied between 60%10,11 and 80%.1,2
Because of dissatisfaction with the results with RT alone, the trials at Memorial Sloan-Kettering Cancer Center (MSKCC) used CMT for the patients with stages I, II, and IIIA disease. Other combined modality trials have also included stage IA patients.12 Our first combined modality trial for early-stage Hodgkin disease conducted between 1975 and 1981 consisted of 6 cycles of MOPP (mustine, vincristine, procarbazine, prednisone) and involved region RT. Complete responses (CRs) were achieved in 96% of patients with a 10% relapse rate at 92 months.11
Between 1981 and 1986, a second trial was conducted for clinical stages (CSs) IA, IIA, and IIIA with 4 cycles of MOPP or thiotepa, vinblastine, and bleomycin (TBV) and involved region RT in a randomized design in an attempt to reduce toxicity. There were no significant differences between MOPP/RT and TBV/RT in CR percentage, or disease-free or overall survival at 5 years, and results were similar to those in the previous trial.13
The trial with chemotherapy alone (doxorubicin, bleomycin, vinblastine, dacarbazine [ABVD]) versus chemotherapy + RT was the next step in the attempt to obtain excellent results in early-stage Hodgkin disease while reducing toxicity. The long-term toxicities of RT and MOPP are well known. The ABVD regimen is superior to the MOPP regimen in advanced-stage Hodgkin disease and is associated with less long-term toxicity than MOPP. The first objective of the trial was to confirm the role of optimal chemotherapy for patients with early-stage Hodgkin disease without tumor bulk, with a drug program reducing risks of toxicity, especially secondary leukemia. The second objective was to determine the necessity for adjuvant RT in combination with optimal chemotherapy that was considered to be 6 cycles of ABVD at the time that the trial was designed. The hypothesis for the second objective was that the chemotherapy combined with RT would result in a superior duration of CR and freedom from progression (FFP).
Patients, materials, and methods
Diagnosis and staging
Histopathologic diagnosis was made according to the Rye modification of the Lukes and Butler classification.14 Clinical staging procedures were performed according to the guidelines of the Ann Arbor and Cotswold conferences.15 Pretreatment evaluations consisted of complete blood count (CBC); platelet count; serum biochemistries including liver function tests, lactic acid dehydrogenase, and uric acid; erythrocyte sedimentation rate; chest x-ray; computerized tomography of chest, abdomen, and pelvis with oral and intravenous contrast; bone marrow biopsy; echocardiogram; pulmonary function tests including diffusion capacity; and double-dose gallium scan with single photon emission computerized tomography. There were 2 patients (1%) who underwent staging laparotomies for pathologic staging. Laparoscopically directed liver biopsies were performed in 5 patients (3%). The rest of the patients were clinically staged.
Randomization and treatment
At time of enrollment, patients were randomized either to receive 6 cycles of ABVD alone or 6 cycles of ABVD followed by RT. The eligibility criteria were as follows: a diagnosis of Hodgkin disease confirmed at MSKCC; no previous treatment; clinical or pathologic staging as IA, IB, IIA, IIB, or IIIA; and lack of bulky nodal tumor (mediastinal mass ≤ 0.33, the thoracic diameter on chest x-ray measured at T11, and/or peripheral or retroperitoneal adenopathy ≤ 10 cm in its largest diameter). Patients with chronic lung disease with a diffusing capacity of less than 60% and/or with cardiac disease with clinical congestive heart failure or an abnormal left ventricular ejection fraction (< 50%) on echocardiogram or multiple gated acquisition (MUGA) scan were excluded.
The protocol was approved by the institutional review board. Patients were enrolled by telephone call or fax to the MSKCC Clinical Trials Office. All patients signed an informed consent. Randomization was performed after a check for eligibility. Patients were stratified according to clinical stage (IA or IIA, IIIA, IB or IIB).
The ABVD regimen consisted of doxorubicin 25 mg/m2, bleomycin 10 units/m2, vinblastine 6 mg/m2, and dacarbazine 375 mg/m2 intravenously on days 1 and 15. Chemotherapy was recycled every 28 days for 6 cycles. Prophylactic use of filgrastim was permitted for subsequent treatment of patients who developed neutropenia and fever or in whom the absolute neutrophil count (ANC) of less than 1000/mm3 necessitated a treatment delay. Patients weighing 70 kg or less received 300 μg and those more than 70 kg received 480 μg daily on days 4 to 11. Pulmonary function tests were repeated after 4 cycles of chemotherapy in all asymptomatic patients; the tests were repeated before 4 cycles if pulmonary symptoms occurred. For patients in whom the diffusing capacity of the lung for carbon monoxide (DLCO) decreased by 20% or greater, bleomycin was omitted from cycles 5 and 6. Bleomycin was also omitted from chemotherapy for all patients who developed pulmonary symptoms before cycle 5 with a similarly documented drop in DLCO.
The planned RT dose for patients achieving a complete remission (CR) or partial remission (PR) on the chemotherapy + RT arm of the trial was 3600 cGy in 180-cGy daily fractions to all fields starting 4 to 6 weeks after completion of chemotherapy. Prior to December 1998, the following fields were used: supradiaphragmatic stages IA, IB, IIA, and IIB—mantle field; infradiaphragmatic stages IA, IB, IIA, and IIB—splenic inverted Y field; stage IIIA without pelvic or inguinal disease—mantle field followed by splenic–para-aortic field (subtotal lymphoid irradiation, STLI); and IIIA with pelvic or inguinal involvement—mantle field followed by splenic-inverted Y field (total lymphoid irradiation, TLI). After December 1998, the RT fields were decreased to involved field (IF) according to the guidelines of Yahalom and Mauch16 as follows: cervical/supraclavicular region, mediastinal/hilar region, axillary region, para-aortic region, spleen, pelvis, and unusual sites at the discretion of the radiation oncologist.
Criteria for responses and toxicity
Analysis was by intent-to-treat. Tumor measurement was in centimeters, and the longest diameter and its perpendicular were applied at the widest portion of the tumor recorded. Patients were considered to be in CR if all clinical evidence of disease and symptoms disappeared for at least 4 weeks. Patients with residual masses that, upon biopsy, showed no evidence of active disease were considered to be in a CR. An 85% reduction in the size of mediastinal and/or abdominal masses (CR unconfirmed [CRu])15 with subsequent stability at least 6 months off treatment were also considered to be in a CR. Patients were considered to be in a partial remission (PR) if they did not meet the criteria for a CR and there was at least a 75% decrease in the sum of the products of the diameters of the measured lesions. Patients were considered to have failed to achieve a major response if initial lesions increased or failed to decrease in size; if they did not decrease by at least 75% within 6 weeks for patients to be considered in CR or PR; or if new lesions developed during treatment. Patients who died from toxicity on treatment were also considered to have failed to achieve a major response.
Toxicity was assessed according to the National Cancer Institute Common Toxicity Criteria v. 1.0 and later 2.0 (National Cancer Institute, Bethesda, MD).
Statistical methods
The statistics in the original protocol were based on several considerations. The probability of relapse from CR for these early-stage Hodgkin disease patients was predicted to be approximately 10% at 5 years. The study was based on 4 years of accrual (n = 90 per arm) and a 2-year minimum follow-up period (a 6-year study). It was anticipated that good power (ie, .84) would exist for detecting a 30.8% probability of relapse at 5 years in the no-RT arm (ie, a hazard ratio of 3.5). This calculation was based on the use of a 2-sided asymptotic t test that assumes an underlying exponential failure time distribution. The hypothesis tested was that radiation therapy added to chemotherapy would result in a superior outcome to chemotherapy alone.
Data and safety monitoring were scheduled yearly for 5 times over an 8-year period starting in the second year. The initial study design (90 patients per arm) was based on the use of a 2-sided test. This approach was overly conservative since it was felt to be highly unlikely that patients who did not receive RT would have a more favorable CR duration. Therefore, early stopping rules were based on a one-sided test (α= .05).
At the fifth meeting of the Data Safety and Monitoring Committee, May 2000, it was recommended that the trial be closed. The slower-than-anticipated accrual was noted. The total accrual was 152 patients, and it was felt that the addition of another 28 patients to meet the target accrual of 180 patients would not add to the statistical power of the results. On the other hand, since this trial was actually conducted over 10 years with an increased median follow-up of 5 years, with 76 patients per arm, there was still an 80% power (with the same type I error of 0.05) to detect the 20% difference (hazard ratio, 3.5) between the 2 arms by using Schoenfeld's formula.17
Overall survival (OS), freedom from disease progression (FFP), and CR duration curves were calculated according to the product-limit method of Kaplan and Meier.18 Freedom from disease progression was defined as the time from enrollment until any progression of disease; this included both disease progression with no response to the chemotherapy and disease recurrence after a PR or CR. Stage I patients whose measurable nodal disease was excised for diagnosis were excluded from the calculations of the percentage of CR and CR duration. Patients with major protocol violations were excluded from the calculations of FFP. However, all patients enrolled were included in the calculations of overall survival (intent-to-treat).
Comparisons of OS, FFP, and CR duration were performed with the log-rank test.19 Comparisons of the percentage of patients in CR or the percentage with toxicity were performed using the Pearson (uncorrected) chi-square test.
Patient characteristics
Between May 1990 and June 2000, 152 patients were randomized: 76 to ABVD + RT and 76 to ABVD alone. The median follow-up time is 67 months (range, 1-125 months). Of the 76 patients randomized to receive RT, 65 actually received it. Of the 11 patients randomized to receive RT who never received it, 6 refused RT, 4 progressed on chemotherapy prior to receiving RT, and 1 never received RT because of bleomycin pulmonary toxicity on chemotherapy. The actual doses of RT administered to all sites were 3600 cGy in 59 patients (1 patient received an additional 900-cGy boost to a bulky site), and 1 patient received each of the following doses: 1800 cGy, 2520 cGy, 3240 cGy, 3300 cGy, 4000 cGy, and 4500 cGy. There were 11 patients on the ABVD + RT arm who received IF RT, and the rest received modified EF RT as described. Patients in each arm of the trial were matched according to age. However, possibly because of the small numbers of patients, the distributions of sex, stage, and histology were somewhat unbalanced between the 2 arms (Table 1). Subset analysis of the entire group according to sex, histology, and stage using the log-rank test failed to detect significant differences in CR duration (sex, P = .83; stage, P = .31; histology, P = .93), freedom from progression (sex, P = .23; stage, P = .57; histology, P = .99), or overall survival (sex, P = .46; stage, P = .60; histology, P = .51).
Patient characteristics
. | Total . | ABVD + RT . | ABVD . |
|---|---|---|---|
| Total patients | 152 | 76 | 76 |
| No. ineligible | 0 | 0 | 0 |
| Median age, y (range) | 31.5 (15-68) | 29 (15-66) | 33 (16-68) |
| Sex, no. (%) | |||
| Male | 87 (57) | 38 | 49 |
| Female | 65 (43) | 38 | 27 |
| Histology, no. (%) | |||
| NS | 115 (76) | 59 | 56 |
| MC | 21 (14) | 7 | 14 |
| LP | 14 (9) | 8 | 6 |
| Not subclassified | 2 (1) | 2 | 0 |
| Stage, no. (%) | |||
| IA | 28 (18) | 9 | 19 |
| IIA | 88 (58) | 51 | 37 |
| IIB | 16 (11) | 7 | 9 |
| IIIA | 20 (13) | 9 | 11 |
| ESR, no (%) | 134 | 66 | 68 |
| A more than 50 mm/h | 19 (14) | 10 | 9 |
| B more than 30 mm/h | 7 (5) | 4 | 3 |
| No. of sites involved, no. (%) | 152 | 76 | 76 |
| 1 to 2 | 61 (40) | 35 | 26 |
| 3 | 33 (22) | 14 | 19 |
| More than 3 | 58 (38) | 27 | 31 |
. | Total . | ABVD + RT . | ABVD . |
|---|---|---|---|
| Total patients | 152 | 76 | 76 |
| No. ineligible | 0 | 0 | 0 |
| Median age, y (range) | 31.5 (15-68) | 29 (15-66) | 33 (16-68) |
| Sex, no. (%) | |||
| Male | 87 (57) | 38 | 49 |
| Female | 65 (43) | 38 | 27 |
| Histology, no. (%) | |||
| NS | 115 (76) | 59 | 56 |
| MC | 21 (14) | 7 | 14 |
| LP | 14 (9) | 8 | 6 |
| Not subclassified | 2 (1) | 2 | 0 |
| Stage, no. (%) | |||
| IA | 28 (18) | 9 | 19 |
| IIA | 88 (58) | 51 | 37 |
| IIB | 16 (11) | 7 | 9 |
| IIIA | 20 (13) | 9 | 11 |
| ESR, no (%) | 134 | 66 | 68 |
| A more than 50 mm/h | 19 (14) | 10 | 9 |
| B more than 30 mm/h | 7 (5) | 4 | 3 |
| No. of sites involved, no. (%) | 152 | 76 | 76 |
| 1 to 2 | 61 (40) | 35 | 26 |
| 3 | 33 (22) | 14 | 19 |
| More than 3 | 58 (38) | 27 | 31 |
NS indicates nodular sclerosis; MC, mixed cellularity; LP, lymphocyte predominance; ESR, erythrocyte sedimentation rate.
Results
Response to treatment and survival
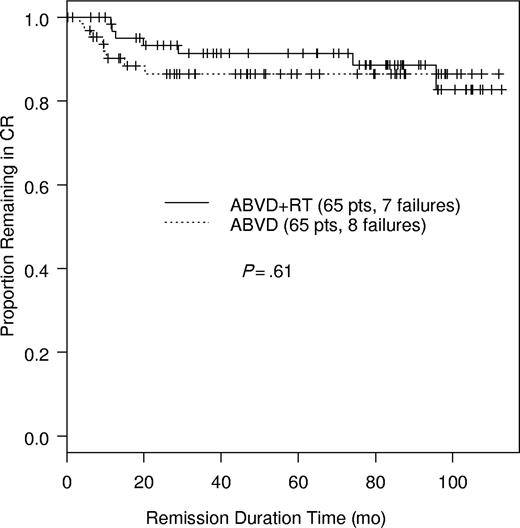
Of the 152 patients, 138 were assessable. There were 14 patients not assessable for response: 1 had a major protocol violation (discontinued treatment after 5 cycles of chemotherapy on the ABVD-alone arm), 2 were lost to follow-up (1 discontinued treatment after 3 cycles on the ABVD + RT arm; 1 discontinued treatment after 4½ cycles on the ABVD + RT arm), and 11 stage IA patients had all measurable disease resected prior to treatment. These 11 patients were followed for disease progression and survival; 5 of 11 were on the ABVD + RT arm and 6 were on the ABVD-alone arm. The 3 patients who discontinued chemotherapy refused further treatment; none was withdrawn by the treating physician because of toxicity. For treatment with ABVD + RT, 65 patients (94%) achieved a CR and 4 (6%) did not have a major response. For ABVD alone, 65 patients (94%) achieved a CR, 1 (1.5%) a PR, and 3 (4.5%) did not have a major response (Table 2). At 60 months, 91% (95% confidence interval [CI], 0.844-0.989) of patients randomized to receive ABVD + RT and 87% (95% CI, 0.782-0.957) of patients randomized to receive ABVD alone remain in CR (P = .61, log-rank) (Figure 1). The 95% CI for CR duration differences at 5 years is –8% to 15%.
Outcome: responses
. | Total, no (%) . | ABVD + RT, no (%) . | ABVD, no (%) . |
|---|---|---|---|
| Total | 152 | 76 | 76 |
| Assessable | 138 | 69 | 69 |
| Not assessable | 14* | 7 | 7 |
| CR | 130 (94) | 65 (94) | 65 (94) |
| PR | 1 (1) | 0 | 1 (1.5) |
| No major response | 7 (5) | 4 (6) | 3 (4.5) |
. | Total, no (%) . | ABVD + RT, no (%) . | ABVD, no (%) . |
|---|---|---|---|
| Total | 152 | 76 | 76 |
| Assessable | 138 | 69 | 69 |
| Not assessable | 14* | 7 | 7 |
| CR | 130 (94) | 65 (94) | 65 (94) |
| PR | 1 (1) | 0 | 1 (1.5) |
| No major response | 7 (5) | 4 (6) | 3 (4.5) |
Results include 1 protocol violation, 2 lost to follow-up, and 11 stage 1 with all measurable disease excised prior to treatment (see “Response to treatment and survival”).
Of the 4 patients who failed to achieve a major response to ABVD + RT, 2 patients progressed as diffuse large B-cell lymphomas before receiving RT. One with stage IA lymphocyte predominant Hodgkin disease remains in remission following high-dose chemotherapy, total lymphoid irradiation, and autologous bone marrow transplantation. The second patient with stage IIA nodular sclerosis Hodgkin disease failed to respond to high-dose chemotherapy and autologous bone marrow transplantation and died. The 2 patients who progressed with Hodgkin disease were both treated with high-dose chemotherapy, total lymphoid irradiation, and autologous peripheral blood stem cell transplantation. One, a 24-year-old woman with stage IIB nodular sclerosis Hodgkin disease, is alive with Hodgkin disease and the other, a 39-year-old man with stage IA nodular sclerosis Hodgkin disease, remains in remission.
Of the 3 patients counted as nonresponders on the ABVD-alone arm of the trial, 2 died of toxic complications while on chemotherapy. One was a 67-year-old woman with clinical stage IIB mixed cellularity Hodgkin disease who died of sepsis in the setting of neutropenia after one cycle of ABVD. The other was a 65-year-old woman with stage IIA nodular sclerosis Hodgkin disease who died of bleomycin pulmonary toxicity following 4 cycles of ABVD. The third patient who failed to respond had stage IIIA nodular sclerosis histology and died of progressive Hodgkin disease.
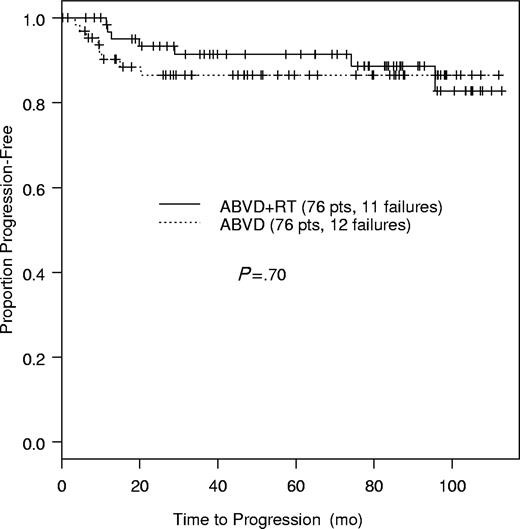
There were 15 patients who relapsed from CR: 7 on the ABVD + RT arm and 8 on the ABVD-alone arm (Table 3). Documented by repeat biopsies were 6 of the 7 relapses on the ABVD + RT arm and 7 of the 8 on the ABVD-alone arm. At 60 months, the FFP for ABVD + RT was 86% (95% CI, 0.781-0.95) and 81% (95% CI, 0.721-0.915) for ABVD alone (P = .61, log-rank) (Figure 2). The 95% CI for the FFP differences at 5 years is –8% to 18%. Of the 7 relapses from CR that occurred on the ABVD + RT arm, 1 was within the RT portal, 4 were both inside and outside the RT portal, 1 was in initial nodal sites in a patient who refused RT, and the site(s) of recurrence was unknown in the seventh. All 8 of the relapses from CR in the ABVD-alone arm would have been within RT portals if it had been administered. Of the relapses, 7 were in initially involved nodal sites and 1 was in a new nodal site.
Relapses from complete and partial remission
. | Relapses . | . | |
|---|---|---|---|
| Treatment . | ABVD + RT . | ABVD . | |
| Number | 7 | 9 | |
| Age, y | 24, 26, 27, 38, 39, 39, 53 | 23, 23, 24, 27, 29, 30, 31, 35, 39 | |
| Sex | |||
| Female | 2 | 6 | |
| Male | 5 | 3 | |
| Initial stage | |||
| IA | 1 | 0 | |
| IIA | 5 | 6 | |
| IIB | 0 | 1 | |
| IIIA | 1 | 2 | |
| Initial response | |||
| CR | 7 | 8 | |
| PR | 0 | 1 | |
. | Relapses . | . | |
|---|---|---|---|
| Treatment . | ABVD + RT . | ABVD . | |
| Number | 7 | 9 | |
| Age, y | 24, 26, 27, 38, 39, 39, 53 | 23, 23, 24, 27, 29, 30, 31, 35, 39 | |
| Sex | |||
| Female | 2 | 6 | |
| Male | 5 | 3 | |
| Initial stage | |||
| IA | 1 | 0 | |
| IIA | 5 | 6 | |
| IIB | 0 | 1 | |
| IIIA | 1 | 2 | |
| Initial response | |||
| CR | 7 | 8 | |
| PR | 0 | 1 | |
Of the 7 relapses from CR on the ABVD + RT arm, 1 died of Hodgkin disease following autologous peripheral blood stem cell transplantation and then a nonablative allogeneic bone marrow transplantation. Of the relapsed patients, 3 are alive with Hodgkin disease. The remaining 3 patients are alive in a subsequent remission, 1 following autologous peripheral blood stem cell transplantation. Of the 8 patients who relapsed from CR on the ABVD-alone arm, 3 died of Hodgkin disease and 5 are alive in a subsequent remission. Of these 5 patients, 3 were treated with autologous peripheral blood stem cell transplantation.
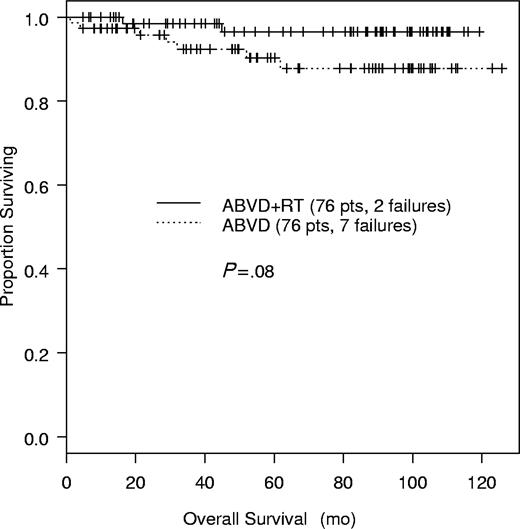
At 60 months, the OS is 97% (95% CI, 0.92-1.00) for ABVD + RT and 90% (95% CI, 0.832-0.981) for ABVD alone (P = .08, log-rank) (Figure 3). The 95% CI for the OS differences at 5 years is –4% to 12%. There were 2 patients who died on the ABVD + RT arm of the trial, 1 of Hodgkin disease and the other of diffuse large B-cell lymphoma, as described. On the ABVD-alone arm, 7 patients died. The 2 deaths due to toxicity of chemotherapy that occurred on treatment, 1 of bleomycin pulmonary toxicity and the other of sepsis, as also described. A third patient died of gastric adenocarcinoma in continued remission of his Hodgkin disease 24 months after completing ABVD. The remaining 4 patients died of Hodgkin disease.
A secondary analysis of the 138 assessable patients (Table 2) was performed on the outcomes only for patients who completed the protocol treatment. There were 8 patients on the ABVD + RT arm and 4 on the ABVD-alone arm who did not complete protocol treatment. Of the 8 patients on the ABVD + RT arm, 3 refused RT, 4 progressed on chemotherapy prior to receiving RT, and 1 had bleomycin pulmonary toxicity that made it impossible to administer RT. Of the 4 patients on the ABVD-alone arm, 2 died of toxicity on chemotherapy as described (1 neutropenia and sepsis, 1 bleomycin toxicity), 1 received RT in error, and 1 did not complete chemotherapy because of a serious but not fatal motorcycle accident. For the remaining 130 patients, the differences in outcomes in the 2 arms were not statistically significant by the log-rank test (CR duration, P = .68; FFP, P = .31; and OS, P = .18).
Toxicity
The most frequent acute toxicity was leukopenia. There were 27 patients (18%) who developed grades 3 and 4 leukopenia. Grade 3 neutropenia was seen in 61 patients (40%) and grade 4 neutropenia, in 26 (17%). Neutropenia was usually seen following the first or second cycle of treatment. For patients with delays in treatment or decreases in drug doses (by 25% for doxorubicin and vinblastine) because of leukopenia/neutropenia, an amendment was made in the protocol in February 1992 permitting the use of prophylactic filgrastim for subsequent ABVD treatments. At some time during treatment, 94 patients (62%) received prophylactic filgrastim. There were 12 patients (8%) hospitalized for neutropenia, and there was 1 death during treatment due to overwhelming sepsis and pneumonia in the setting of neutropenia. Other hematologic toxicity included grade 4 thrombocytopenia in 3 patients (2%), a grade 3 decrease in hemoglobin in 5 patients (3%), and a grade 4 decrease in 2 patients (1%).
The major nonhematologic toxicity was pulmonary and related to bleomycin. There were 33 patients (22%) who had discontinuation of bleomycin because of a more than 20% decrease in DLCO. These patients were continued on treatment with the omission of bleomycin. There were 10 symptomatic patients who received brief courses of glucocorticoids. None of these patients developed chronic symptomatic pulmonary disease. Of the patients who had bleomycin discontinued, 18 were on the ABVD + RT arm; bleomycin was discontinued after 2 cycles of ABVD in 1 patient, 3 cycles in 2 patients, 4 cycles in 8 patients, 4½ cycles in 5 patients, and 5 cycles in 2 patients. Of the patients who had bleomycin discontinued, 15 were on the ABVD-alone arm; bleomycin was discontinued after 1½ cycles in 1 patient, 2½ cycles in 1 patient, 3 cycles in 1 patient, 3½ cycles in 1 patient, 4 cycles in 6 patients, 4½ cycles in 2 patients, 5 cycles in 1 patient, and 5½ cycles in 2 patients. There was one death due to bleomycin during treatment in a 65-year-old woman. Omission of bleomycin did not obviously affect outcome. There was no significant difference in major response for patients who received bleomycin during the full 6 cycles of treatment compared with those who had bleomycin omitted from any number of cycles of treatment or those who received bleomycin during 4 or fewer cycles of treatment (Fisher exact test).
The only other nonhematologic toxicities seen with any frequency were grade 3 nausea in 15 patients (10%) and grade 3 emesis in 7 patients (5%). Aggressive antiemetic regimens using dexamethasone with either ondansetron or granisetron were used.
There have been 8 second malignancies so far, 3 on the arm with ABVD alone and 5 on the arm with ABVD and RT. The 3 secondary malignancies on the arm with ABVD alone were a fatal gastric carcinoma and 2 synchronous nonfatal skin cancers (skin basal cell carcinoma and localized melanoma in a single patient), 12 and 47 months, respectively, following completion of treatment. Both occurred during continued remission of Hodgkin disease. On the ABVD + RT arm, one patient developed a follicular thyroid carcinoma, and diffuse large B-cell non-Hodgkin lymphomas occurred in 2 patients on chemotherapy prior to the RT. Following completion of the RT, 2 patients on that arm developed carcinomas: one a papillary thyroid carcinoma at 68 months and the other one a parotid carcinoma at 48 months. One occurred within and the other one at the margins of the RT portals.
Discussion
This report describes the results of a randomized trial of ABVD + RT versus ABVD alone for early-stage nonbulky Hodgkin disease. It was conducted over a 10-year period in a single institution. The sample size was sufficient to determine that the expected superiority of combined modality treatment as described in “Statistical methods” was not achieved. No differences were seen in the treatment outcomes between CMT and CT alone, but the sample size was insufficient to detect a difference of less than 20% or equivalence in outcomes. A small nonrandomized study from Spain demonstrated a progression-free survival of 86% and an OS of 92% at 56 months for 6 cycles of ABVD without RT for stages I and II Hodgkin disease, results similar to our experience.20,21
The good results of this trial are consistent with our previous experience and those of others with combined modality trials for early-stage Hodgkin disease.11-13 Short-term toxicity was mild for most patients in the present study. However, there were 2 deaths related to chemotherapy (1 sepsis, 1 bleomycin lung), and 1 patient could not receive RT because of bleomycin pulmonary toxicity. Nausea and vomiting were usually well controlled with the use of antiemetics. Approximately one fifth of the patients had bleomycin dropped from chemotherapy either because of an asymptomatic decrease in diffusing capacity or mild pulmonary symptoms. A few of the symptomatic patients had brief courses of systemic glucocorticoids, but there have been no patients who developed chronic symptomatic pulmonary toxicity. Monitoring of diffusing capacity after 4 cycles of ABVD (8 treatments) and discontinuation of bleomycin with a decrease in diffusing capacity seems to have been successful in preventing permanent lung damage without affecting treatment outcome. This confirms our experience with some of these patients and other patients in a previous report.22
Second solid tumor malignancies, particularly related to RT, are a major concern. Recently, 4 long-term follow-up studies in patients treated for Hodgkin disease demonstrated the high incidence of second malignancies with long-term follow-up.23-26 The 25- to 30-year actuarial risk of second malignancies was 22% to 27%. Although RT and CMT seem to be the major treatment risk factor for most of the solid tumors, there is some suggestion that MOPP chemotherapy alone is associated with an increased risk of adenocarcinoma of the lung.26,27 The 2 early cases of diffuse large B-cell lymphoma may represent evolution of the underlying malignant process from Hodgkin disease to B-cell non-Hodgkin lymphoma.28 The late occurrences of non-Hodgkin lymphomas have been reported with all treatment modalities: chemotherapy, RT, and CMT.25 Like the solid tumors, these lymphomas may be secondary to treatment. There is insufficient follow-up time to assess the long-term toxicities of treatment, including second malignancies, in the present study.
There have been few randomized trials of chemotherapy alone versus combined modality treatment in early-stage Hodgkin disease. A variant of MOPP chemotherapy with low-dose cyclophosphamide, vinblastine, procarbazine, and prednisone (CVPP) alone for 6 cycles was compared with 6 cycles of CVPP and IF RT for 277 clinical stage (CS) IA and IIA patients in a trial of Grupo Argentina de Tratamiento de Leucemia Aguda (GATLA) and Grupo Latinamericano de Tratamiento de Hemopatias Malignas (GLATHEM) groups in Argentina. At 7 years of follow-up, differences in the disease-free survival (DFS) and overall survival for CVPP alone and CVPP + RT were not statistically significant in a subgroup analysis of 177 “favorable” patients, although longer DFS and OS were observed for CVPP + RT for “unfavorable” patients.29 A recent randomized trial from India comparing ABVD + RT versus ABVD alone in all stages of Hodgkin disease found a significant difference in event-free and overall survival in favor of ABVD + RT, but there was no significant difference in either outcome in a subset analysis of patients with stages I and II disease.30 The Hodgkin Disease–6 (HD-6) trial of the National Cancer Institute of Canada and the Eastern Cooperative Oncology Group randomized Hodgkin disease patients with nonbulky CSs IA and IIA without abdominal nodal involvement to “standard treatment” (favorable, EF RT; unfavorable, 2 ABVD + EF RT) or ABVD alone (4-6 cycles, approximately 30% received 4). There was a 6% difference in estimated 5-year progression-free survival, a difference that was statistically significant. There was no difference in overall survival.31 The Children's Cancer Group reported on trials on 829 pediatric Hodgkin disease patients with all stages. The 501 patients who achieved a CR with chemotherapy were randomized to low-dose involved-field radiotherapy (IFRT) or no further treatment. An analysis by “intent-to-treat” demonstrated a borderline significant increase in 3-year EFS (P = .057) in the group receiving CMT, and the increase was significant by an “as-treated” analysis (P = .0024). There was no difference in OS.32 In stages III and IV Hodgkin disease the European Organization of Research and Treatment of Cancer (EORTC) has recently reported the results of a large trial of 739 patients treated with 6 to 8 cycles of MOPP/ABV hybrid chemotherapy with a randomization of patients achieving a CR (421 patients) to IF RT or no RT. There was no difference in the 5-year event-free survivals and a trend toward a decreased overall survival in the CMT arm.33
Although no statistically significant differences in CR duration, FFP, and survival were seen between patients treated with ABVD alone and ABVD + RT, our trial lacks statistical power to determine if the 2 treatment approaches truly result in the same outcome. Differences in survival are particularly difficult to demonstrate in randomized studies for early-stage Hodgkin as was first demonstrated years ago in the pivotal randomized trial of involved field versus extended field RT.10
This problem of interpreting differences in outcome with small numbers of patients is demonstrated by the number of deaths on each arm of the trial. The difference between 7 deaths on the chemotherapy-only arm and 2 deaths on the chemotherapy + RT arm approaches statistical significance in actuarial analysis (Figure 3, P = .08). However, 2 of the 7 deaths on the chemotherapy-only arm were due to and occurred during chemotherapy treatment and could have occurred on either arm of the trial. A third death due to gastric carcinoma on the ABVD-alone arm also could have occurred on either arm. This illustrates the requirement for the very large numbers of patients to demonstrate the equivalency of 2 different treatment regimens with respect to both toxicity as well as effectiveness with strong statistical power. Also at the current median follow-up time, it may be too early to see all the expected treatment-related cancers. Longer follow-up is necessary to determine if the development of late complications of therapy will alter these results.
In an attempt to minimize the number of patients with a CR on the ABVD + RT arm who might refuse to receive RT, patients were randomized to each arm prior to treatment. This resulted in 9 patients not receiving assigned RT for a variety of reasons. This could potentially have confounded results, although an “as-treated analysis” failed to demonstrate differences in outcome between the 2 arms of the trial. In other studies, patients were randomized to RT or no RT after achieving a response to chemotherapy, a design that could avoid potential confusion in interpretation of results.32
It is possible that the late complications of treatment could be substantially reduced by the omission of RT from the treatment of nonbulky early-stage Hodgkin disease patients. Alternatively, the more refined techniques and limited treatment portals of current involved field RT techniques combined with fewer chemotherapy drugs and cycles might reduce the long-term toxicity. Also, a larger randomized study with greater statistical power might demonstrate a significant but small advantage in event-free survival for combined modality treatment compared with chemotherapy alone. A definitive answer to the effectiveness and toxicity of chemotherapy alone versus combined modality treatment will require both the short-term analysis reported here (median, 5 years) and longer term analysis (median, more than 10 years) in order to fully assess the benefits of either approach.
There are 2 potential approaches for further research. One would be to identify which patients with nonbulky early-stage Hodgkin disease will benefit from consolidative RT in addition to chemotherapy. Functional imaging with fluorodeoxyglucose (FDG) positron emission tomography has promise in predicting the absence of active Hodgkin disease following treatment,34 and a chemotherapy trial testing its use in this population of patients will be conducted in the intergroup setting under the leadership of the Cancer and Acute Leukemia Group B. The other approach would be large randomized trials with adequate statistical power and follow-up time to establish whether the outcome with standard chemotherapy is equivalent to combined modality treatment (with standard or shorter chemotherapy) for the overall population of patients with nonbulky early-stage Hodgkin disease.
Prepublished online as Blood First Edition Paper, August 17, 2004; DOI 10.1182/blood-2004-04-1311.
Supported by The Lymphoma Foundation, The Ernest and Jeanette Dicker Foundation, The Lymphoma Research Fund-HD, and CA-05826.
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal