The current interpretation of chronic lymphocytic leukemia (CLL) as a malignancy characterized by the accumulation of lymphocytes reluctant to undergo apoptosis has to be consistent with the need for a proliferative compartment that keeps nourishing the accumulation compartment. As virtually all circulating CLL lymphocytes are long-lived elements arrested in the G0/early G1 phase of the cell cycle, it may be asked to what extent CLL cells proliferate and how the neglected aspect of proliferation relates to the disease's natural history. These questions are even more relevant as the analysis of immunoglobulin heavy chain variable region (IgVH) sequences has revealed 2 molecularly recognizable distinct clinical entities, mutated and unmutated CLL, the median survival of mutated CLL being significantly longer.1,2 IgVH somatic hypermutations increase diversity of the B-cell receptor (BCR) during T-cell–dependent normal immune responses that occur within germinal centers (GCs). It is thus generally accepted that the mutated CLL cell has transited through the GC and that antigen (Ag) stimulation may influence the disease evolution. The phenotype of unmutated cases resembles that of Ag-experienced B cells,3 suggesting some sort of Ag contact also in unmutated cases.
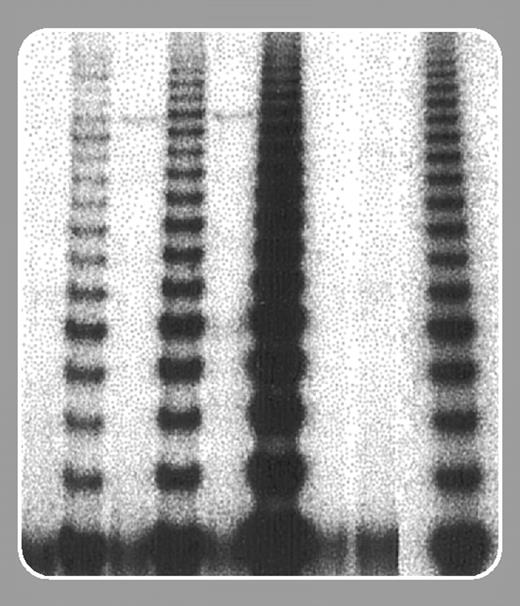
Damle and colleagues (page 375) have tackled these issues by investigating telomere length and telomerase activity in CLL cells classified according to IgVH mutational status. Telomere erosion is a normal process that accompanies cell division, and telomere length reflects the number of replications. When telomere length shortens to a level that may endanger a cell's life, the enzyme telomerase compensates by adding hexameric repeats to telomere ends. Telomerase activity is promptly triggered by cell activation: B cells, upon activation by Ag encounter within the GC, extend their telomeres to permit preservation of more adaptive BCRs. In cancer the presence of active telomerase frequently identifies more aggressive disease variants. The temporal relationships of telomerase activity and telomere elongation are dynamic and not easily interpretable, primarily because it is difficult to know at what point in the replicative history of a B lymphocyte telomerase activity was initiated.
Damle and coworkers raise 3 interesting points: (1) CLL cells as a whole have significantly shorter telomeres than normal B cells, implying that a considerable number of cell divisions must have occurred within the leukemic clone. (2) Leukemic cells from unmutated cases have significantly shorter telomeres than mutated cases and enhanced telomerase activity. It follows that unmutated cells are senescent, have undergone several replications, and have had several opportunities to acquire chromosomal aberrations. Also, since short telomeres are associated with genomic instability, these cells are prone to develop further genomic aberrations. Hence they are endowed with a more aggressive potential. It will be important to determine which stimuli—Ag's? Interactions with the microenvironment?— activate telomerase in vivo and rescue these potentially harmful elements. (3) Leukemic cells from mutated cases have telomeres of variable length with minimal telomerase activity. Thus, mutated clones are made of cells of variable ages that have had a variable (though overall reduced compared with unmutated clones) number of divisions, hence a lower chance to undergo genomic aberrations, which explains the patients' better prognosis.
Future investigations will explore (1) whether telomere shortening (and telomerase activity) are equally distributed among all clonal cells or whether an intraclonal heterogeneity might favor the evolution of a dangerous subclone; (2) if mutated and unmutated cases differ in cell kinetics in vivo; and (3) when, in a B cell's life, telomere shortening occurred in relationship with leukemic transformation.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal