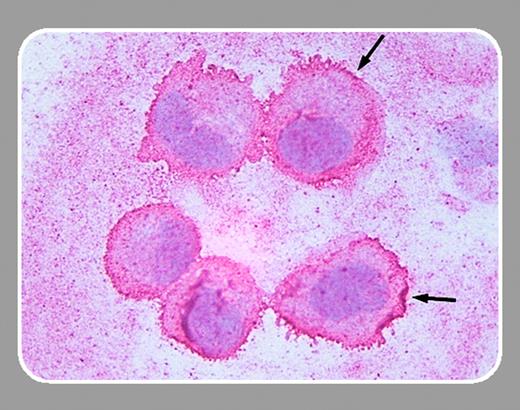
Hemolytic uremic syndrome (HUS) is principally a thrombotic disease caused by Shiga toxins released during intestinal infection with enterohemorrhagic bacteria such as Escherichia coli O157:H7. Shiga toxins damage renal and other endothelial cells, resulting in coagulation activation characterized by increased thrombin generation and fibrin turnover starting at least 4 to 5 days prior to development of HUS. Coagulation activation results in localized microvascular thrombosis, followed by microangiopathic hemolytic anemia, thrombocytopenia, and renal failure. There are 2 principal forms of Shiga toxin, designated Stx1 and Stx2, with Stx2 showing greater pathogenicity. Until recently it was thought that the primary mechanism of Shiga toxin injury was cell destruction by inhibition of protein synthesis. Recent studies indicate that subinhibitory concentrations of Shiga toxin induce expression of a number of endothelial genes, including monocyte chemoattractant protein-1 and interleukin-8.
In this issue Matussek and colleagues (page 1323) expand this work by comparing the endothelial response to Stx1 and Stx2 using whole genome arrays, reverse transcriptase–polymerase chain reaction (RT-PCR), and protein expression experiments. Both Stx1 and Stx2 induced expression of a relatively small number of endothelial genes (about 25 of 12 000 tested), most often in the chemokine and cytokine families. Overall, Stx2 tended to induce a stronger response, and some genes were up-regulated in only Stx1 or Stx2, suggesting possible differences in the inflammatory response modulating endothelial injury. Matussek and colleagues have shown again that analysis of array data alone may be deceptive. The array data indicated that Stx1 did not induce expression of some genes that were later found to be stimulated using RT-PCR and protein expression studies (false negatives). Analysis of Stx2 gene regulation is further complicated by the large number of allelic variants of Stx2 that have been described. In summary, their work provides a list of new gene expression targets for further study that may shed light on the pathogenesis of Shiga toxin–related endothelial injury.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal