It has been suggested that a switch in chemokine receptor expression underlies Langerhans cell migration from skin to lymphoid tissue. Activated cells are thought to down-regulate CCR6, whose ligand macrophage inflammatory protein-3α (MIP-3α)/CCL20 is expressed in skin, and up-regulate CCR7, whose ligands are in lymphoid tissues. In Langerhans cell histiocytosis (LCH), pathologic Langerhans cells (LCs) accumulate in several tissues, including skin, bone, and lymphoid organs. We have examined 24 LCH cases and find that pathologic LCs expressed CCR6 and CCR7 coincidentally in all cases. Furthermore, MIP-3α/CCL20 is expressed by keratinocytes in involved skin and by macrophages and osteoblasts in involved bone. Expression of CCR6 by pathologic LCs may contribute to their accumulation in nonlymphoid organs such as skin and bone, whereas CCR7 expression may direct them to lymphoid tissue. Histiocytes in Rosai-Dorfman disease and hemophagocytic syndrome also coexpressed CCR6 and CCR7, suggesting that this may be a general attribute of abnormal histiocytes.
Introduction
The Langerhans cell histiocytoses (LCHs) are clonal disorders of dendritic cells in which infiltrative lesions cause tissue destruction in a variety of organs.1,2 One of the cardinal manifestations of LCH is the accumulation of partially activated pathologic Langerhans cells (LCs) in target tissues such as skin or bone, suggesting an abnormality of cell trafficking. A tightly coordinated pattern of chemokine receptor expression has been proposed to underlie the migration of normal LCs.3-5 Resting LCs express CCR6 whose ligand, macrophage inflammatory protein-3α (MIP-3α)/CCL20, is secreted by cutaneous keratinocytes and is up-regulated by inflammation.6 When LCs attracted by increased MIP-3α/CCL20 expression are activated by local inflammatory mediators, they down-regulate CCR6 and up-regulate CCR7. Loss of CCR6 releases mature LCs from the local MIP-3α/CCL20-rich environment and permits them to respond to ligands for CCR7, namely, Epstein-Barr virus–induced molecule-1 ligand chemokine (ELC)/CCL19 and secondary lymphoid organ chemokine (SLC)/CCL21, which are expressed in the T-cell zones of lymph nodes. Failure of pathologic LCs to emigrate from target tissues raises the possibility that this well-orchestrated pattern of chemokine receptor expression may be disrupted in LCH. We tested this idea by examining the expression of CCR6 and CCR7 in LCH and other histiocytoses.
Study design
Tissue
Paraffin blocks of tissues from patients with LCH or other histiocytic processes were identified by pathologists at Children's Hospital (Boston, MA). Archival tissue samples were acquired in accordance with the Dana-Farber Cancer Institute's institutional review board (IRB)–reviewed rules. Histologic sections were reviewed again by one of us (M.D.F.) to confirm diagnoses.
Immunohistochemistry
Antibodies were obtained from the following sources: mouse antihuman CCR6, monoclonal IgG2b (clone 53103.111) from R & D Systems (Minneapolis, MN); mouse antihuman CCR7, monoclonal IgG1 (clone CCR7.6B3) from eBioscience (San Diego, CA); goat antihuman MIP-3α/CCL20 from R & D Systems; mouse antihuman CD1a (clone O10) from Coulter-Immunotech (Miami, FL); rabbit antihuman S100 from Dako (Carpinteria, CA); species- and isotype-matched controls were from R & D Systems. Epitope retrieval was accomplished by steaming deparaffinized sections for 40 minutes in 1 mM EDTA (ethylenediaminetetraacetic acid; pH 8.0; for anti-CCR7 and anti-MIP-3α/CCL20) or in 10 mM citrate (pH 6.0; for anti-CCR6), or steaming for 25 minutes in 1 mM EDTA (pH 8.0; for anti-CD1a). After incubation in primary antibody (anti-CCR6, anti-CCR7 at 1:200, anti-CD1a at 1:100, anti-S100 at 1:3000) or control antibody, rabbit antimouse immunoglobulin (Dako) was added at 1:150 followed by horseradish peroxidase (HRP)–labeled polymer conjugated to goat antirabbit immunoglobulin (Envision+ detection system; Dako). After incubation in anti-MIP-3α/CCL20 at 1:200 or Tris (tris(hydroxymethyl)aminomethane) buffer, peroxidase-conjugated rabbit antigoat immunoglobulin (Dako) was added at 1:100 followed by HRP-labeled polymer conjugated to goat antirabbit immunoglobulin. Antibody localization was effected using a peroxidase reaction with DAB+ (3,3′-diaminobenzidine tetrahydrochloride; Dako) as chromogen. Slides were counterstained with methyl green.
Results and discussion
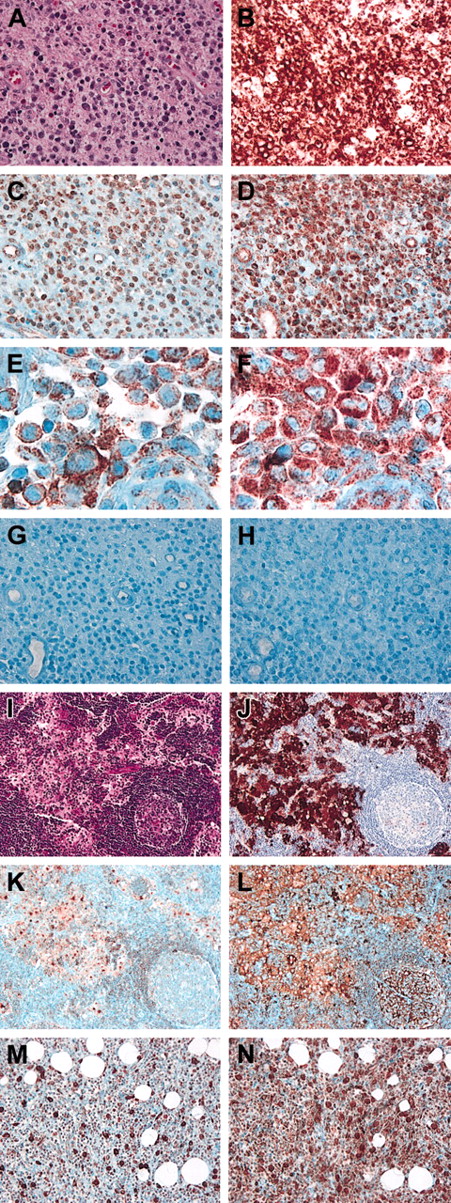
Twenty-four LCH cases were analyzed by immunohistochemistry for CCR6 and CCR7 expression. In every case, CD1a+ pathologic LCs coexpressed both chemokine receptors. Figure 1A-H shows an example in which serial sections from an involved lymph node were stained for CD1a, CCR6, and CCR7. Nearly all the cells in this heavily infiltrated area were CD1a+, CCR6+, and CCR7+. Pathologic LCs within a section stained with variable intensity for CCR6, but stained uniformly for CCR7. Higher power views (Figure 1E) confirmed that all cells having a nuclear morphology typical of lesional LCH cells stained for CCR6. Incidentally, we found that endothelium was also prominently CCR7+ (Figure 1D).
CCR6 and CCR7 expression in histiocytic processes.
(A-H) Serial sections of LCH-involved lymph node, demonstrating coexpression of CCR6 and CCR7 by CD1a+ pathologic LCs. (A) Hematoxylin and eosin. (B) Anti-CD1a. (C) Anti-CCR6 showing pathologic LCs staining with variable intensities. (D) Anti-CCR7 showing uniform staining of all pathologic LCs (note endothelial cell staining as well). (E) Anti-CCR6 at high power showing typical LCH lesional cells all staining for CCR6. (F) Anti-CCR7 at high power showing cells in the same field and having the same morphology as those in panel E staining for CCR7. (G) IgG2B isotype control for anti-CCR6. (H) IgG1 isotype control for anti-CCR7. (I-L) Serial sections of RDD-involved lymph node, demonstrating coexpression of CCR6 and CCR7 in areas containing S100+ RDD histiocytes. (I) Hematoxylin and eosin. (J) Anti-S100. (K) anti-CCR6. (L) Anti-CCR7. Note reactive germinal center in the lower right portion of panels I-L in which B cells are CCR6− and CCR7+. (M-N) Serial sections of HPS-involved soft tissue, demonstrating coexpression of CCR6 and CCR7 by histiocytes. (M) Anti-CCR6. (N) Anti-CCR7; note large, intensely positive histiocytes in panels M and N. All panels are original magnification × 400, except for E and F, which are × 1000.
CCR6 and CCR7 expression in histiocytic processes.
(A-H) Serial sections of LCH-involved lymph node, demonstrating coexpression of CCR6 and CCR7 by CD1a+ pathologic LCs. (A) Hematoxylin and eosin. (B) Anti-CD1a. (C) Anti-CCR6 showing pathologic LCs staining with variable intensities. (D) Anti-CCR7 showing uniform staining of all pathologic LCs (note endothelial cell staining as well). (E) Anti-CCR6 at high power showing typical LCH lesional cells all staining for CCR6. (F) Anti-CCR7 at high power showing cells in the same field and having the same morphology as those in panel E staining for CCR7. (G) IgG2B isotype control for anti-CCR6. (H) IgG1 isotype control for anti-CCR7. (I-L) Serial sections of RDD-involved lymph node, demonstrating coexpression of CCR6 and CCR7 in areas containing S100+ RDD histiocytes. (I) Hematoxylin and eosin. (J) Anti-S100. (K) anti-CCR6. (L) Anti-CCR7. Note reactive germinal center in the lower right portion of panels I-L in which B cells are CCR6− and CCR7+. (M-N) Serial sections of HPS-involved soft tissue, demonstrating coexpression of CCR6 and CCR7 by histiocytes. (M) Anti-CCR6. (N) Anti-CCR7; note large, intensely positive histiocytes in panels M and N. All panels are original magnification × 400, except for E and F, which are × 1000.
To determine whether coincident CCR6 and CCR7 expression was unique for LCH histiocytes, we examined 7 cases of Rosai-Dorfman disease (RDD) and 2 cases of malignancy-associated hemophagocytic syndrome (HPS). S100+ RDD histiocytes coexpressed CCR6 and CCR7 as did HPS histiocytes (Figure 1I-N). As in the LCH cases, CCR6 staining intensity varied among histiocytes in the same section, whereas CCR7 staining was more uniform. The staining pattern in the lymph node in panels K and L of Figure 1 provided validation for the specificity of our immunohistochemical staining: follicular B cells stained for CCR7 but not CCR6, consistent with previous reports.7 8
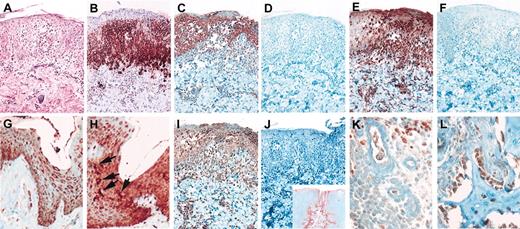
To test whether the ligand for CCR6, MIP-3α/CCL20, was expressed in tissues affected by LCH, we examined involved skin and bone. An example is shown in Figure 2 in which CCR6+ pathologic LCs have accumulated close to the base of the epidermal cells, many of which are themselves CCR6+ (Figure 2A-D). As in Figure 1, essentially all of the CCR6+ pathologic LCs are also CCR7+ (Figure 2E-F). Most of the keratinocytes are CCR7+ as well; however, expression tended to be stronger in more superficial layers of the epidermis. In contrast, nonspecifically inflamed skin had scattered normal LCs that expressed high levels of CCR7 but not CCR6 (Figure 2G-H), although it is possible that some degree of CCR6 expression could be obscured by keratinocytes that also expressed CCR6.
MIP-3α/CCL20, CCR6, and CCR7 expression in LCH skin and bone lesions.
(A-F, I-J) LCH skin lesion. (A) Hematoxylin and eosin. (B) Anti-CD1a. (C) Anti-CCR6. (D) IgG2B isotype control for anti-CCR6. (E) Anti-CCR7. (F) IgG1 isotype control for anti-CCR7. (G) Nonspecific inflammatory skin lesion, anti-CCR6 showing keratinocyte staining. (H) Nonspecific inflammatory skin lesion, anti-CCR7 showing scattered cells with LC morphology staining intensely for CCR7 (arrows) as well as keratinocyte staining. (I) LCH lesion (same case as panels A-F), anti-MIP-3α/CCL20 showing staining of keratinocytes as well as infiltrating cells. (J) Buffer control for panel I; inset, anti-MIP3a/CCL20 staining of tonsil showing expression by crypt epithelium. (K) LCH bone lesion, anti-MIP-3α, showing intense staining of macrophages (top) and light staining of infiltrating pathologic LCs (left). (L) LCH bone lesion, anti-MIP-3α, showing staining of osteoblasts. Panels A-J are original magnification × 200; J inset is original magnification × 20; panels K and L are original magnification × 400.
MIP-3α/CCL20, CCR6, and CCR7 expression in LCH skin and bone lesions.
(A-F, I-J) LCH skin lesion. (A) Hematoxylin and eosin. (B) Anti-CD1a. (C) Anti-CCR6. (D) IgG2B isotype control for anti-CCR6. (E) Anti-CCR7. (F) IgG1 isotype control for anti-CCR7. (G) Nonspecific inflammatory skin lesion, anti-CCR6 showing keratinocyte staining. (H) Nonspecific inflammatory skin lesion, anti-CCR7 showing scattered cells with LC morphology staining intensely for CCR7 (arrows) as well as keratinocyte staining. (I) LCH lesion (same case as panels A-F), anti-MIP-3α/CCL20 showing staining of keratinocytes as well as infiltrating cells. (J) Buffer control for panel I; inset, anti-MIP3a/CCL20 staining of tonsil showing expression by crypt epithelium. (K) LCH bone lesion, anti-MIP-3α, showing intense staining of macrophages (top) and light staining of infiltrating pathologic LCs (left). (L) LCH bone lesion, anti-MIP-3α, showing staining of osteoblasts. Panels A-J are original magnification × 200; J inset is original magnification × 20; panels K and L are original magnification × 400.
All skin samples showed MIP-3α/CCL20 expression by keratinocytes and some LCs (Figure 2I). Because of the technical challenge of detecting secreted proteins by immunohistochemistry, we validated the use of the MIP-3Α/CCL20 antibody by staining tonsil (Figure 2J inset). We detected high-level MIP-3α/CCL20 expression by crypt epithelial cells, but only weak or negative staining of mucosal epithelial cells, essentially as previously described.9 Thus, keratinocytes in skin affected by LCH express the CCR6 ligand MIP-3α/CCL20. We also examined several bone samples and detected MIP-3α/CCL20 expression by resident macrophages and osteoblasts (Figure 2K-L).
Our results show that histiocytes in LCH, RDD, and HPS coexpress CCR6 and CCR7. On one hand, expression of CCR6, which is characteristic of resting LCs, is surprising given reports that pathologic LCs have a marker profile associated with activation, including expression of CD2, CD11b, CD44, CD54, B7-1, and B7-2,10-12 and loss of E-cadherin.13 On the other hand, pathologic LCs have some characteristics of normal resting LCs including persistence of Birbeck granules,14 inefficient antigen presentation, cytokine secretion patterns similar to resting LCs,15 and expression of L-selectin.16 This combination of resting and activated phenotypes indicates that pathologic LCs may suffer from a maturation defect; their expression of CCR6 would be consistent with the immature component of this compound phenotype. Expression of CCR7 by CCR6+ histiocytes would be consistent with its mature, activated component. In contrast, coexpression of these receptors in RDD and HPS may simply reflect gene activation in a more mature macrophage-derived cell type.
Although our study has not directly demonstrated a mechanism for the pattern of pathologic LC infiltration in LCH, the chemokine and chemokine receptor expression we describe is consistent with a model in which coexpression of CCR6 and CCR7 results in histiocyte migration into tissues that express cognate ligands: MIP-3α/CCL20 in skin and bone and ELC/CCL19 and SLC/CCL21 in secondary lymphoid organs. Notably, the major site of extranodal involvement by RDD is skin,17which may also be explained by our model. These results suggest that CCR6 and CCR7 antagonists may be therapeutically useful in the histiocytoses. At the very least, blockade of these receptors might stimulate the emigration of inflammatory pathologic LCs from involved tissue thereby providing substantial palliative relief. In addition, however, evidence is accumulating for the antiapoptotic activities of chemokines,18 especially for malignant cells, and interrupting chemokine-dependent survival pathways in pathologic LCs could result in even more profound benefits.
The authors thank Christine Penta for administrative assistance, and Dorie and Michael Mufson for their support.
Supported by National Institutes of Health grants CA53091 and AI50225, and a generous grant from Team Histio of the Dana-Farber Cancer Institute/Jimmy Fund Marathon Walk.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Barrett J. Rollins, M430, Dana-Farber Cancer Institute, 44 Binney St, Boston, MA 02115; e-mail:barrett_rollins@dfci.harvard.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal