Abstract
The protein products of the recombination activating genes (RAG1 and RAG2) initiate the formation of immunoglobulin (Ig) and T-cell receptors, which are essential for B- and T-cell development, respectively. Mutations in the RAGgenes result in severe combined immunodeficiency disease (SCID), generally characterized by the absence of mature B and T lymphocytes, but presence of natural killer (NK) cells. Biochemically, mutations in the RAG genes result either in nonfunctional proteins or in proteins with partial recombination activity. The mutated RAGgenes of 9 patients from 7 families were analyzed for their recombination activity using extrachromosomal recombination substrates, rearrangement of endogenous Ig loci in RAGgene–transfected nonlymphoid cells, or the presence of Ig gene rearrangements in bone marrow (BM). Recombination activity was virtually absent in all 6 patients with mutations in the RAG core domains, but partial activity was present in the other 3 RAG-deficient patients, 2 of them having Omenn syndrome with oligoclonal T lymphocytes. Using 4-color flow cytometry, we could define the exact stage at which B-cell differentiation was arrested in the BM of 5 RAG-deficient SCID patients. In 4 of 5 patients, the absence of recombination activity was associated with a complete B-cell differentiation arrest at the transition from cytoplasmic (Cy) Igμ− pre–B-I cells to CyIgμ+ pre–B-II cells. However, the fifth patient showed low frequencies of precursor B cells with CyIgμ and surface membrane IgM, in line with the partial recombination activity of the patient's mutatedRAG gene and the detection of in-frame Ig gene rearrangements in BM.
Introduction
Human severe combined immunodeficiency disease (SCID) refers to a group of disorders, which can be classified based on the pattern of inheritance and the immunologic phenotype.1One type of SCID is characterized by autosomal recessive inheritance, absence of T and B lymphocytes in peripheral blood (PB), but presence of natural killer (NK) cells (non-T non-B SCID). A number of patients suffering from non-T non-B SCID carry mutations in the recombination activating genes (RAG) 1 or 2.2 The 2 humanRAG genes are located in a tail-to-tail orientation on chromosome 11p13 and are expressed during T- and B-cell development in the thymus and bone marrow (BM), respectively.3-7 The RAG proteins are essential to initiate recombination of immunoglobulin (Ig) and T-cell receptor (TCR) loci.8-10 They introduce double-strand breaks at the recombination signal sequences (RSSs) flanking the variable (V), diversity (D), and joining (J) gene segments, which are then joined to form a V(D)J exon encoding the antigen-binding part of Ig and TCR molecules.11 12
The RAG1 and RAG2 proteins both contain a core domain, which is essential for recombination activity.13-16 Although the N-terminus of RAG1 and the C-terminus of RAG2 seem to be dispensable for recombination activity, it has been shown that they might be specifically required for Ig gene recombination.17-21 Most mutations in the RAG genes causing non-T non-B SCID affect the core domain and encode nonfunctional proteins (“null” alleles).2 On the other hand, some RAGmutations in the core domain are associated with partial VDJ recombination activity, causing a variant of non-T non-B SCID, called Omenn syndrome (OS).22 OS is characterized by oligoclonal, autoreactive T cells with a T-helper 2 phenotype, absence of B lymphocytes, but high serum IgE levels. The clinical phenotype of OS resembles the clinical phenotype resulting from maternal-fetal T-cell engraftment (MFT) in a newborn with non-T non-B SCID.
The absence of T or B lymphocytes (or both) in the PB of patients suffering from RAG-deficient SCID results from a differentiation arrest during T- and B-cell development in the thymus and BM, respectively. The localization of this differentiation arrest has been defined in murine thymus and BM.23,24 However, no such data are available in humans. From a theoretical viewpoint, one would expect that RAG-deficient SCID patients have a complete B-cell differentiation arrest at the transition from cytoplasmic (Cy) Igμ− to CyIgμ+ precursor B cells, but this has not been shown yet.25 Here we present data on 9 RAG-deficient SCID patients from 7 families. The recombination activity of the mutated RAG genes was analyzed using extrachromosomal recombination substrates, rearrangement of endogenous Ig loci in (mutated) RAG gene–transfected human nonlymphoid cells, or the occurrence of Ig gene rearrangements (immunogenotype) in BM of the SCID patients. In addition, from 5 RAG-deficient SCID patients, the composition of the precursor B-cell compartment in BM could be analyzed with 4-color flow cytometric immunophenotyping.
Materials and methods
Cell samples
Over the last 15 years, we received BM samples from 7 B cell–negative SCID patients, and Epstein-Barr virus (EBV)–transformed B-cell lines derived from BM precursor B cells of 2 siblings with B cell–negative SCID.26
The BM samples from the 7 SCID patients were subjected to Ficoll-Paque (density: 1.077 g/mL; Pharmacia, Uppsala, Sweden) density centrifugation. The recovered mononuclear cells (MCs) were frozen and stored in liquid nitrogen and thawed later for flow cytometric immunophenotyping studies. Granulocytes were used for DNA extraction.27
We have previously reported on an extensive study concerning the composition of the precursor B-cell compartment in the BM of 18 healthy children using triple labelings.28 We repeated our flow cytometric analyses using quadruple labelings in thawed BM samples from 6 of these healthy children (age range, 1 year 7 months to 5 years 11 months; mean age, 3 years 10 months; 4 boys, 2 girls), who were BM donors for their siblings.
All cell samples were obtained according to the informed consent guidelines of the Medical Ethics Committees of the Leiden University Medical Center and the University Hospital Rotterdam.
DNA extraction, PCR amplification, and analysis of Ig gene rearrangements
DNA was extracted from BMMCs and transfected φNX-WTA cells (a human epithelial kidney cell line) with the QIAamp Blood kit (Qiagen, Chatsworth, CA).29 Polymerase chain reaction (PCR) was performed as described previously.30 In each 100-μL PCR 0.1 to 1 μg DNA, 10 to 12.5 pmol 5′ and 3′ oligonucleotides, and 1 U AmpliTaq Gold polymerase (Applied Biosystems, Foster City, CA) were used. Most oligonucleotides for amplification of theIGH, IGK, and IGL genes were published before.31-33 PCR conditions were 7 minutes at 95°C, followed by 45 seconds at 94°C, 90 seconds at 57 to 65°C, 2 minutes at 72°C for 40 cycles, followed by a final extension step (7 minutes at 72°C). DNA from BMMCs was analyzed for DH-JH and VH-JHrearrangements.32 The PCR products were cloned in the pGEM-T easy vector and subsequently sequenced. When IGHrearrangements were identified, DNA from BMMCs was also analyzed for Vκ-Jκ and Vλ-Jλrearrangements.34 Involved Ig gene segments were identified using IMGT, the international ImMunoGeneTics databasehttp://imgt.cnusc.fr:8104 (Initiator and coordinator: Marie-Paule Lefranc, Montpellier, France,lefranc@ligm.igh.cnrs.fr).35
LR-PCR for amplification of RAG genes
The entire RAG1 or RAG2 gene was amplified in a single long-range (LR)–PCR reaction (100 μL), using 4 U rTth DNA polymerase XL (Applied Biosystems) for subsequent sequencing analysis of the LR-PCR product or 5 U Pfu enzyme mix (Stratagene, La Jolla, CA) for cloning the LR-PCR product; we used 30 or 14 pmol oligonucleotides, respectively. The sequences of the oligonucleotides used for the LR-PCR were TGAGGCTAATACAATGTGGAA (RAG1 forward), ACAACCTTGGCTTTGATTTAC (RAG1 reverse), TTCGGCTAGTCTTTATTCAC (RAG2 forward), and CTTTGGCACATCATTCA (RAG2 reverse), respectively. Restriction-sites for BamHI and NotI were incorporated into the 5′ and 3′ oligonucleotides used for cloning, respectively. LR-PCR conditions were 2 minutes, 94°C, followed by 15 seconds, 94°C, 30 seconds, 57°C, and 4 minutes, 68°C for 40 cycles using 10-second autoextension from cycle 21 onward. In case of cloning, the LR-PCR conditions were 45 seconds, 94°C, followed by 45 seconds, 94°C, 45 seconds, 62°C, and 3.5 to 6.5 minutes, 72°C for 30 to 35 cycles using 10-sec autoextension from cycle 21 onward. After the last cycle final extension was performed for 10 minutes at 72°C.
Fluorescent sequencing reaction and analysis
The LR-PCR products of RAG1 and RAG2 were purified using QIAquick PCR purification kit (Qiagen). Five to 9 μL purified PCR product was sequenced with 5 μL dRhodamine dye terminator mix (Applied Biosystems), using 3.3 pmol internal sequencing primers. All sequencing was performed as described before,32 using an ABI Prism 377 fluorescent sequencer (Applied Biosystems).
Cloning of mutated and wild-type RAG genes
The LR-PCR products containing the entire RAG1 orRAG2 open reading frame were isolated after digestion withBamHI and NotI and cloned into theBamHI-NotI cut vector pEBB under control of the EF-1 promoter.18 The cloned wild-type and mutatedRAG genes were sequenced to exclude the presence of PCR-induced mutations.
V(D)J recombination assay using an extrachromosomal recombination substrate
Two micrograms pEBB-RAG1 (mutated or wild type) together with 2 μg pEBB-RAG2 (mutated or wild type) and 1 μg of the extrachromosomal recombination substrate (pDVG93) were transfected into Chinese hamster ovary (CHO9) cells using SuperFect Transfection Reagent (Qiagen). Transfected cells were cultured for 2 days before harvesting. Plasmid pDVG93 contains 2 RSS elements with the same orientation. On V(D)J recombination, the sequence in between the 2 RSS elements is inverted, which can be detected by PCR.20Nontransfected pDVG93 plasmids can be discriminated from transfected plasmids based on digestion of DpnI restriction sites, which become resistant on demethylation after transfection.
A real-time quantitative (RQ)–PCR assay was developed to quantify the recombination activity. For this purpose, we designed primers DG89 and DG147 and TaqMan probe FM23 for quantitative detection of inversional rearrangements as well as a set of control primers and TaqMan probe for quantitative detection of all transfected pDVG93 plasmids with multipleDpnI restriction sites between the primers.20DNA recovered from the transfection experiments was DpnI digested to remove nontransfected plasmids, added to the TaqMan universal PCR master mix (Applied Biosystems), and equally divided over 4 tubes, 2 tubes for specific amplification and 2 for control amplification. RQ-PCR was performed as described before using an ABI Prism 7700 (Applied Biosystems).36 The PCR cycle at which a fluorescent signal became detectable (threshold cycle or CT) was comparable in the duplicate tubes (ΔCT < 1.0). The level of recombination activity of the mutated RAG genes was compared to that of wild-typeRAG genes. All RQ-PCR experiments were performed multiple times, showing virtually identical results.
Transfection of wild-type RAG genes was used as a positive control for recombination activity. Using these RQ-PCR results, standard curves for the specific and the control amplification were generated. All standard curves met the following requirements: slopes between −3.3 and −3.7 to ensure optimal amplification, correlation coefficient close to 1.0, and a fluorescent signal intensity (ΔRn) greater than 1.0. Using the relative standard curve method with separate tubes (Applied Biosystems, user bulletin no. 2, relative quantitation of gene expression), the relative recombination activity of the wild-type RAG genes was arbitrarily set to 100%. The relative recombination activity of mutated RAG genes was calculated from the specific standard curve and corrected using the control standard curve.
Analysis of V(D)J recombination of endogenous Ig loci following transfection of cloned RAG genes in combination with E47 in φNX-WTA cells
Transfection was performed as described before.37In short, 6 μg pEBB-RAG1 (mutated or wild type) together with 6 μg pEBB-RAG2 (mutated or wild type) and 6 μg βhAP-E47 (under control of the human β-actin promoter) were transfected into confluent φNX-WTA human kidney epithelial cells using the calcium-phosphate method.37 Transfected cells were cultured for 3 days before harvesting. DNA was isolated and analyzed for rearrangement of endogenous loci, such as DH4-JH, Vκ1-Jκ, and Vλ3-Jλ1/2/3. These rearrangements were earlier shown to be specifically induced on transfection of E47 and RAG1 and RAG2.37
Flow cytometric analysis of BM samples from healthy children and SCID patients
Fifty-microliter aliquots of thawed BMMCs (10 × 106 cells/mL) were incubated for 10 minutes at room temperature with combinations of optimally titrated monoclonal antibody (mAb): 50 μL fluorescein isothiocyanate (FITC)–conjugated mAb, 50 μL phycoerythrin (PE)–conjugated mAb, 50 μL peridinin chlorophyl protein–cyanin 5.5 (PerCP-Cy5.5)–conjugated mAb, and 50 μL allophycocyanin (APC)–conjugated mAb were used to detect membrane-bound antigens. After incubation, the cells were washed and further processed depending on the type of quadruple labeling. The 14 applied quadruple labelings are summarized on a Web page (http://www.eur.nl/fgg/immu/tables/Table1.htm).
Quadruple labelings for membrane-bound antigens (labelings 1-7) were directly analyzed by flow cytometry using FACSCalibur (Becton Dickinson, San Jose, CA). For quadruple labelings involving intracellular staining of Cy CD79a, CyIgμ, and CyVpreB,38 and intranuclear staining of terminal deoxynucleotidyl transferase (TdT) (labelings 8-14), we first performed the membrane labelings, followed by permeabilization of the BM cells using IntraPrep Permeabilization Reagent (Immunotech, Marseille, France), and subsequent intracellular staining.39 40
Results
Patient characteristics and mutations in the RAGgenes
Based on clinical characteristics and immunophenotyping results of PB, 9 patients from 7 families were diagnosed as having B cell–negative SCID (Table 1). SCID-1 was studied extensively and published before.20 MFT in patients diagnosed with OS (SCID-1 and SCID-5) was excluded by HLA typing and by detection of a homozygous RAG gene mutation in PBMC DNA.
Mutation analysis in patients presenting with B cell–negative SCID
| Family . | Diagnosis* . | Mutation . | Polymorphism . | Consanguinity of parents . | ||
|---|---|---|---|---|---|---|
| DNA level† . | Protein level . | DNA level† . | Protein level . | |||
| RAG-SCID 1 | OS | RAG1631delT1-153 | Codon 199 stop | RAG1G858A1-153 | Arg249His | Yes |
| RAG-SCID 2‡ | T−B−SCID | RAG2 1913delG1-153 | Codon 247 stop | RAG1 A2571G1-153 | Lys820Arg | Yes |
| RAG-SCID 3 | T−B−SCID | RAG2A2643C1-155 | His481Pro | Yes | ||
| RAG-SCID 4‡ | T−B−SCID | RAG2 1913delG1-155 | Codon 247 stop | RAG1 A2571G1-155 | Lys820Arg | Unknown |
| RAG-SCID 5 | OS | RAG2T2558A1-153 | Trp453Arg | RAG1G858A1-153 | Arg249His | No |
| RAG-SCID 6 | T−B− SCID | RAG2C1247T1-155 | Gln16 stop | No | ||
| RAG-SCID 7 | T−B− SCID | RAG1G1323A1-155 | Arg404Gln | RAG1G858A1-155 | Arg249His | No |
| Family . | Diagnosis* . | Mutation . | Polymorphism . | Consanguinity of parents . | ||
|---|---|---|---|---|---|---|
| DNA level† . | Protein level . | DNA level† . | Protein level . | |||
| RAG-SCID 1 | OS | RAG1631delT1-153 | Codon 199 stop | RAG1G858A1-153 | Arg249His | Yes |
| RAG-SCID 2‡ | T−B−SCID | RAG2 1913delG1-153 | Codon 247 stop | RAG1 A2571G1-153 | Lys820Arg | Yes |
| RAG-SCID 3 | T−B−SCID | RAG2A2643C1-155 | His481Pro | Yes | ||
| RAG-SCID 4‡ | T−B−SCID | RAG2 1913delG1-155 | Codon 247 stop | RAG1 A2571G1-155 | Lys820Arg | Unknown |
| RAG-SCID 5 | OS | RAG2T2558A1-153 | Trp453Arg | RAG1G858A1-153 | Arg249His | No |
| RAG-SCID 6 | T−B− SCID | RAG2C1247T1-155 | Gln16 stop | No | ||
| RAG-SCID 7 | T−B− SCID | RAG1G1323A1-155 | Arg404Gln | RAG1G858A1-155 | Arg249His | No |
Diagnoses were obtained in PB.
Patients from different families with identical mutations.
Homozygous mutation, both parents were carrier.
Seemingly homozygous mutation, but deletion of the other allele was not ruled out.
We detected mutations in the RAG1 or RAG2 genes in all 9 B cell–negative SCID patients (Table 1). The RAG1genes contained 4 different mutations, including one novel. Two of the 4 mutations (Arg249His and Lys820Arg) represented polymorphisms. The Arg249His mutation has been shown to be a functionally intact polymorphism by recombination activity studies,2 whereas the Lys820Arg mutation was interpreted as a polymorphism based on its allelic frequency.41 In this study, we show that the Lys820Arg mutation indeed retained intact recombination activity (see below). The other 2 RAG1mutations (codon 199 stop in SCID-1 and Arg404Gln in SCID-7), were shown by recombination activity studies (see below) to have a disease-causing effect.
We detected 4 different mutations in the RAG2 genes, including 3 novel mutations (Table 1). The disease-causing effect of the 3 novel mutations (codon 247 stop in SCID-2 and SCID-4, His481Pro in SCID-3, and Gln16 stop in SCID-6) was shown by recombination activity studies (see below). It has been shown before that the Trp453Arg mutation in SCID-5 retained partial RSS nicking and hairpin formation function, as well as a reduced capacity to form signal and coding joints, compatible with the clinical diagnosis of OS in SCID-5 (Table 1).42 For this reason, we did not clone the Trp453Arg mutation for recombination studies.
According to the information obtained by the clinicians, families SCID-2 and SCID-4 were unrelated. Nevertheless, we identified the same disease-causing mutation in RAG2 (codon 247 stop) and the same polymorphism in RAG1 (Lys820Arg) in both families.
V(D)J recombination activity
After transfection, plasmid pDVG93 was used as template for PCR and subsequent hybridization with a radioactive probe (results not shown), as well as for RQ-PCR reaction after digestion with the restriction enzyme DpnI. The results of the RQ-PCR reaction are shown in Table 2. Transfection of the wild-type RAG1 gene or the Lys820Arg mutation resulted in identical amplification curves. After correction for transfection efficiency and the amount of pDVG93 added to the RQ-PCR reaction, the relative recombination activities were comparable, indicating that the Lys820Arg mutation represents a functional polymorphism.
Relative recombination activity of mutated RAGgenes
| Patient . | RAG1 protein . | RAG2 protein . | Relative recombination activity using pDVG93 (%)* . | E47 induced rearrangements of endogenous loci in ϕNX-WTA cells . | ||
|---|---|---|---|---|---|---|
| Vκ1-Jκ . | DH4-JH . | Vλ3-Jλ . | ||||
| Healthy control | Wild type | Wild type | 100 | + | + | + |
| RAG-SCID 1 | N-terminal truncation | Wild type | 9.3 ± 2.9 | + | − | + |
| RAG-SCID 2 and 4 | Lys820Arg | Codon 247 stop | 1.4 ± 1.6 | − | − | − |
| Lys820Arg | Wild type | 115.1 ± 54.4 | + | + | + | |
| Wild type | Codon 247 stop | 1.6 ± 2.4 | − | − | − | |
| RAG-SCID 3 | Wild type | His481Pro | 3.2 ± 2.0 | + | − | + |
| RAG-SCID 6 | Wild type | Gln16 stop | 0 | − | − | − |
| RAG-SCID 7 | Arg404Gln | Wild type | 1.3 ± 1.5 | − | − | − |
| Mock transfection† | — | — | 0 | − | − | − |
| Patient . | RAG1 protein . | RAG2 protein . | Relative recombination activity using pDVG93 (%)* . | E47 induced rearrangements of endogenous loci in ϕNX-WTA cells . | ||
|---|---|---|---|---|---|---|
| Vκ1-Jκ . | DH4-JH . | Vλ3-Jλ . | ||||
| Healthy control | Wild type | Wild type | 100 | + | + | + |
| RAG-SCID 1 | N-terminal truncation | Wild type | 9.3 ± 2.9 | + | − | + |
| RAG-SCID 2 and 4 | Lys820Arg | Codon 247 stop | 1.4 ± 1.6 | − | − | − |
| Lys820Arg | Wild type | 115.1 ± 54.4 | + | + | + | |
| Wild type | Codon 247 stop | 1.6 ± 2.4 | − | − | − | |
| RAG-SCID 3 | Wild type | His481Pro | 3.2 ± 2.0 | + | − | + |
| RAG-SCID 6 | Wild type | Gln16 stop | 0 | − | − | − |
| RAG-SCID 7 | Arg404Gln | Wild type | 1.3 ± 1.5 | − | − | − |
| Mock transfection† | — | — | 0 | − | − | − |
Mean of 4 RQ-PCR reactions using plasmids from 4 different transfections.
Mock transfection consisted of H2O in case of transfection of CHO9 cells and of E47 without wt RAG genes in case of transfection of ϕNX-WTA cells.
After correction for transfection efficiency and the amount of pDVG93 added to the RQ-PCR reaction, the mutated RAG genes of SCID-1 and SCID-3 showed the highest residual recombination activities (Table 2). SCID-1 suffered from an OS-like T+/B− SCID.20 The RAG1631delT mutation in this patient was shown to result in an N-terminal truncation of RAG1, leaving the core domain unaffected.20SCID-3 suffered from a genuine non-T, non-B SCID. The amino acid substitution (His481Pro) in this patient was located outside the core domain in the C-terminus of RAG2. The RAG core domain mutations in SCID-2, SCID-4, SCID-6, and SCID-7 resulted in very low relative recombination activities (Table 2). It has been published recently that a RAG1 Arg404Trp mutation (comparable to the Arg404Gln mutation in SCID-7) resulted in complete absence of recombination activity as well.43
Rearrangement of endogenous Ig loci after transfection of φNX-WTA human kidney epithelial cells
To study the ability of mutated RAG genes to rearrange endogenous Ig loci, we transfected wild-type or mutated RAGgenes together with transcription factor E47 in φNX-WTA cells. φNX-WTA cells are human kidney epithelial cells that do not express RAG proteins and for this reason provide a good model system to study the effect of cloned RAG mutations. Transfection of E47 together with wild-type RAG genes was shown to specifically induce DH4-JH, Vκ1-Jκ, and Vλ3-Jλ rearrangements.37Therefore, we analyzed the occurrence of these rearrangements in our transfection assay (Table 2). Transfection of E47 without wt RAGgenes did not result in rearrangements.
The mutated RAG genes of SCID-1 and SCID-3 with the highest relative recombination activity in the extrachromosomal recombination assay were also able to perform Vκ1-Jκ and Vλ3-Jλ rearrangements when cotransfected with E47 (Table 2). Except for the Lys820Arg polymorphism in RAG1, we could not detect DH4-JH rearrangements after transfection of mutated RAG genes.
Ig gene rearrangements in BMMCs
To study the in vivo capacity of mutated RAG genes to rearrange Ig loci during human B-cell differentiation, DNA was isolated from BMMCs of several RAG-deficient SCID patients and investigated for the occurrence of incomplete DH-JH and complete VH-JH rearrangements. IGHrearrangements were detected in only 2 of 7 RAG-deficient SCID patients studied (Table 3), the same patients (SCID-1 and SCID-3) who were shown to harbor partial recombination activity (Table 2). The 2 patients with IGH rearrangements were also analyzed for the presence of IGK andIGL rearrangements. As expected in patients suffering from RAG-deficient SCID, no somatic mutations could be detected (Table3).
Analysis of IGH, IGK, and IGL gene rearrangements in BMMCs of RAG-deficient SCID patients
| Patient . | Origin of DNA . | Analyzed gene . | PCR products . | V gene segment . | Del . | Junctional region . | Del . | D gene segment . | Del . | Junctional region . | Del . | J gene segment . | Frame . | Somatic mutations . | No. of identical clones . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RAG-SCID 1 | BMMC | IGH | Identified | DH2-15 | − 5 | T | − 2 | JH4 | NA | NA | 1 | ||||
| IGK | Not identified | ||||||||||||||
| IGL | Identified | Vλ2 | − 4 | CCT | – | – | – | – | 0 | Jλ3 | + | Absent | 1 | ||
| RAG-SCID 3 | BMMC | IGH | Identified | VH3-7 | 0 | TTGTA | − 2 | DH3-22 | 0 | – | − 1 | JH3b | + | Absent | 4 |
| VH5-51 | − 1 | GC | − 1 | DH2-15/ INV | − 15 | GGGCTACGGGG | − 6 | JH4b | + | Absent | 6 | ||||
| DH3-10 | − 7 | G | − 11 | JH2 | NA | NA | 4 | ||||||||
| DH2-21 | − 7 | AAGAC | − 4 | JH3b | NA | NA | 1 | ||||||||
| DH4-23 | − 3 | GACTGCGA | − 11 | JH4 | NA | NA | 1 | ||||||||
| DH4-17 | − 1 | ACTAG | − 4 | JH5 | NA | NA | 3 | ||||||||
| IGK | Not identified | ||||||||||||||
| IGL | Identified | Vλ3-10∗01 | 0 | – | – | – | – | – | 0 | Jλ3∗01 | + | Absent | 3 |
| Patient . | Origin of DNA . | Analyzed gene . | PCR products . | V gene segment . | Del . | Junctional region . | Del . | D gene segment . | Del . | Junctional region . | Del . | J gene segment . | Frame . | Somatic mutations . | No. of identical clones . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RAG-SCID 1 | BMMC | IGH | Identified | DH2-15 | − 5 | T | − 2 | JH4 | NA | NA | 1 | ||||
| IGK | Not identified | ||||||||||||||
| IGL | Identified | Vλ2 | − 4 | CCT | – | – | – | – | 0 | Jλ3 | + | Absent | 1 | ||
| RAG-SCID 3 | BMMC | IGH | Identified | VH3-7 | 0 | TTGTA | − 2 | DH3-22 | 0 | – | − 1 | JH3b | + | Absent | 4 |
| VH5-51 | − 1 | GC | − 1 | DH2-15/ INV | − 15 | GGGCTACGGGG | − 6 | JH4b | + | Absent | 6 | ||||
| DH3-10 | − 7 | G | − 11 | JH2 | NA | NA | 4 | ||||||||
| DH2-21 | − 7 | AAGAC | − 4 | JH3b | NA | NA | 1 | ||||||||
| DH4-23 | − 3 | GACTGCGA | − 11 | JH4 | NA | NA | 1 | ||||||||
| DH4-17 | − 1 | ACTAG | − 4 | JH5 | NA | NA | 3 | ||||||||
| IGK | Not identified | ||||||||||||||
| IGL | Identified | Vλ3-10∗01 | 0 | – | – | – | – | – | 0 | Jλ3∗01 | + | Absent | 3 |
PCR products of the IGH gene could not be identified using DNA from BMMCs in patients RAG-SCID 2.1, 2.2, 4, 5, and 6.
Del indicates deletion of germline gene segment nucleotides; NA, not applicable; INV, inverted.
Patients SCID-7.1 and 7.2 were 2 sisters suffering from the sameRAG1 mutation. This Arg404Gln mutation was shown to cause a complete loss of function (Table 2). The EBV-transformed B-cell lines of both patients were reported to have germline IGH,IGK, and IGL genes, as assessed by Southern blotting.26
Composition of the BM lymphocyte gate and design of an optimal B-cell gate
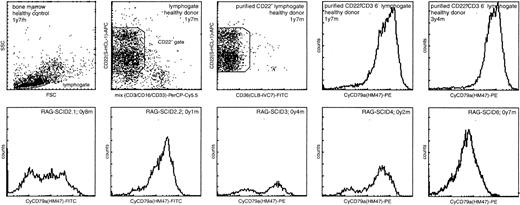
As shown previously, the composition of the BM lymphocyte gate in healthy children is highly variable, because of “contamination” with T lymphocytes, NK cells, myeloid precursors, and normoblasts.28 Therefore, reliable comparison of B-cell subpopulations in BM samples from healthy children and RAG-deficient SCID patients requires analysis within a well-defined and “purified” B-cell gate (Figures 1 and2).
BM samples of RAG-deficient SCID patients contained increased numbers of the most immature CD22+/CyCD79a− pro-B cells.
CyCD79a expression of the precursor B-cell compartment was analyzed within a lymphocyte gate and a CD22+ gate, which was “purified” by exclusion of cells with expression of CD3, CD16, or CD33. In healthy children the CD22+/CyCD79a−pro-B-cell subset represented a minor fraction of the total precursor B-cell compartment. In most RAG-deficient SCID patients this CyCD79a− subset was relatively large but variable in size. Furthermore, the level of CyCD79a expression in the SCID patients (mainly pre–B-I cells) was lower than in the healthy controls (mainly pre–B-II cells and immature B cells). The age at BM sampling is indicated.
BM samples of RAG-deficient SCID patients contained increased numbers of the most immature CD22+/CyCD79a− pro-B cells.
CyCD79a expression of the precursor B-cell compartment was analyzed within a lymphocyte gate and a CD22+ gate, which was “purified” by exclusion of cells with expression of CD3, CD16, or CD33. In healthy children the CD22+/CyCD79a−pro-B-cell subset represented a minor fraction of the total precursor B-cell compartment. In most RAG-deficient SCID patients this CyCD79a− subset was relatively large but variable in size. Furthermore, the level of CyCD79a expression in the SCID patients (mainly pre–B-I cells) was lower than in the healthy controls (mainly pre–B-II cells and immature B cells). The age at BM sampling is indicated.
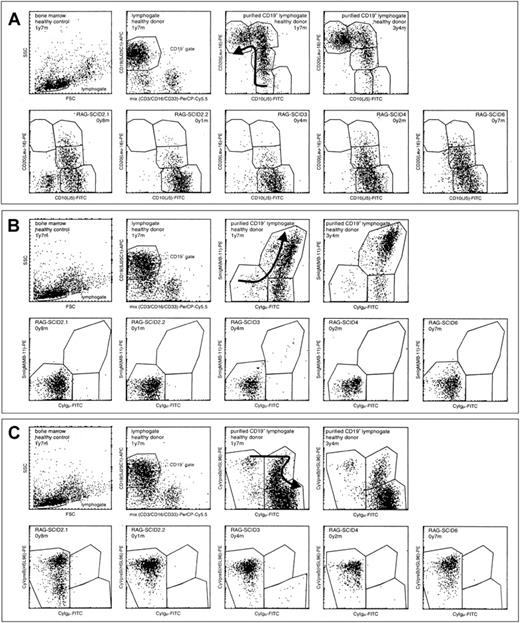
Flow cytometric analysis of thawed BM samples from 5 RAG-deficient SCID patients compared to 2 healthy children.
The precursor B-cell compartment was analyzed within a lymphocyte gate and a CD19+ gate, which was purified by exclusion of cells expressing CD3, CD16, or CD33. (A) Analysis of CD10 and CD20 expression within the purified CD19+ lymphocyte gate. (B) Analysis of Cylgμ and SmlgM expression within the purified CD19+lymphocyte gate. (C) Analysis of Cylgμ and CyVpreB expression within the purified lymphocyte gate. The sequential order of the B-cell differentiation stages is indicated with arrows in the youngest healthy child. The composition of the precursor B-cell compartment in the 2 healthy children was representative of that in other healthy children (n = 6). In general, RAG-deficient SCID patients lacked the more mature B-cell differentiation stages with a strong relative increase in the immature B-cell differentiation stages. According to Nomura et al, expression of CyVpreB precedes expression of CD19.45Within a CD19+ lymphocyte gate, all cells should thus be CyVpreB+ or CyIgμ+ (C). Therefore, we suggest that the double-negative events represent apoptotic cells. The age at BM sampling is indicated.
Flow cytometric analysis of thawed BM samples from 5 RAG-deficient SCID patients compared to 2 healthy children.
The precursor B-cell compartment was analyzed within a lymphocyte gate and a CD19+ gate, which was purified by exclusion of cells expressing CD3, CD16, or CD33. (A) Analysis of CD10 and CD20 expression within the purified CD19+ lymphocyte gate. (B) Analysis of Cylgμ and SmlgM expression within the purified CD19+lymphocyte gate. (C) Analysis of Cylgμ and CyVpreB expression within the purified lymphocyte gate. The sequential order of the B-cell differentiation stages is indicated with arrows in the youngest healthy child. The composition of the precursor B-cell compartment in the 2 healthy children was representative of that in other healthy children (n = 6). In general, RAG-deficient SCID patients lacked the more mature B-cell differentiation stages with a strong relative increase in the immature B-cell differentiation stages. According to Nomura et al, expression of CyVpreB precedes expression of CD19.45Within a CD19+ lymphocyte gate, all cells should thus be CyVpreB+ or CyIgμ+ (C). Therefore, we suggest that the double-negative events represent apoptotic cells. The age at BM sampling is indicated.
During our initial flow cytometric analyses of SCID BM samples, we detected coexpression of CD36 and the pan B-cell markers CD22, CyCD79a, and CD19 in SCID patients and virtually not in healthy controls. CD36 is expressed on platelets, mature monocytes, and macrophages, during stages of erythroid cell development and on some macrophage-derived dendritic cells. Therefore, we added CD36 as exclusion marker to some essential labelings (labelings 5, 10, and 14; seehttp://www.eur.nl/fgg/immu/tables/Table1.htm), resulting in increased purity of the B-cell gates.
We have shown previously that CD22 is a reliable pan B-cell marker, which is rarely expressed on CD3+ T cells, CD33+ myeloid cells, or CD16+ NK cells.28 We identified the entire B-cell compartment as being CD22+. In healthy children the CyCD79a+and the CD19+ fractions within the CD22+ B-cell compartment were very large (labelings 5 and 14; see Web page), that is, 98.7% and 97.6%, respectively. The percentages of the different subpopulations within the CyCD79a+ or CD19+gates were recalculated into percentages of the CD22+population, by multiplying with 0.987 and 0.976, respectively. The same approach was followed for SCID patients, who contained a substantially larger fraction of CD22+/CyCD79− pro-B cells (Figure 1).
B-cell subsets in BM from healthy donors
Based on detailed triple flow cytometric labelings, we previously presented the composition of the precursor B-cell compartment in healthy children and found that its composition is stable during childhood.28,44 Because we now extended our flow cytometric protocol to 14 quadruple labelings, we have repeated our flow cytometric analyses on thawed BM samples from 6 of the previously studied healthy children, resulting in the recognition of 9 consecutive stages. We have previously compared the composition of the precursor B-cell compartment in fresh BM and thawed BMMCs from healthy children and we could not detect major selective loss of particular precursor B-cell subsets.28
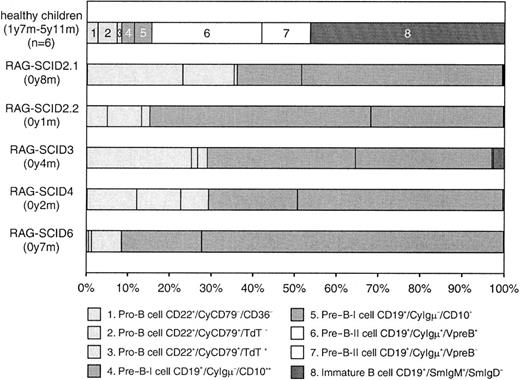
The mature B-cell population in BM varied between healthy children mainly because of blood contamination with CD10−/SmIgM+/SmIgD+ B lymphocytes.28 To correct for this variance in our comparative studies between precursor B cells in normal BM and in BM from SCID patients, we excluded the mature CD10−/SmIgM+/SmIgD+ B-cell population (stage 9) from our calculations. Consequently, the percentages of stages 1 to 8 were recalculated and set at 100% (Figure3).
Composition of the precursor B-cell compartment in RAG-deficient SCID patients compared with healthy children.
The precursor B-cell compartment was set at 100% after exclusion of CD10−/SmIgM+/SmIgD+ mature B cells.28 All RAG-deficient SCID patients showed a similar differentiation arrest with approximately 99% of the precursor B cells in the pro-B and pre–B-I stages (stages 1-5), thereby revealing an arrest at the transition from CyIgμ− pre–B-I (stages 4 and 5) to CyIgμ+ pre–B-II-cells (stages 6 and 7, white bars). Only in SCID-3 was some leakiness observed with more than 3% Ig+ B cells. These Ig+ B cells were mainly SmIgM+ immature B cells (stage 8, dark bar), which is also shown in Figure 2B. The age of BM sampling is indicated.
Composition of the precursor B-cell compartment in RAG-deficient SCID patients compared with healthy children.
The precursor B-cell compartment was set at 100% after exclusion of CD10−/SmIgM+/SmIgD+ mature B cells.28 All RAG-deficient SCID patients showed a similar differentiation arrest with approximately 99% of the precursor B cells in the pro-B and pre–B-I stages (stages 1-5), thereby revealing an arrest at the transition from CyIgμ− pre–B-I (stages 4 and 5) to CyIgμ+ pre–B-II-cells (stages 6 and 7, white bars). Only in SCID-3 was some leakiness observed with more than 3% Ig+ B cells. These Ig+ B cells were mainly SmIgM+ immature B cells (stage 8, dark bar), which is also shown in Figure 2B. The age of BM sampling is indicated.
Flow cytometric analysis of precursor B cells in BM of SCID patients
The BM samples from 7 RAG-deficient SCID patients were available, but BM samples from OS patients SCID-1 and SCID-5 could not be analyzed using flow cytometry due to the very low percentage of precursor B cells (< 2% CD22+/CD36− precursor B cells within the lymphocyte gate).
In BM from healthy children, approximately 15% of the precursor B-cell compartment consisted of CyIgμ− precursor B cells, whereas in BM from all 5 analyzed RAG-deficient SCID patients approximately 99% (97%-100%) of the precursor B-cell compartment was located in these stages (Figure 3). Although this differentiation arrest was virtually identical in the 5 evaluated SCID patients, some CyIgμ+ pre–B-II cells and SmIgM+ immature B cells could be detected in SCID-3 (Figures 2 and 3). Furthermore, the composition of the remaining precursor B-cell compartment (pro-B cell and pre–B-I cell subsets) in the 5 SCID patients was highly variable, even in the 3 patients with the same homozygous RAG2mutation (SCID-2.1, 2.2, and 4).
Discussion
We have identified 9 patients from 7 families with B cell–deficient SCID due to RAG mutations. The mutations in the RAG genes of SCID-2, SCID-4, SCID-6, and SCID-7 affected the core domains of the RAG proteins and were shown to abrogate recombination activity (almost) completely. The other 3 RAGmutations were located outside the core domain (SCID-1, SCID-3, and SCID-5) and were all associated with partial recombination activity (Table 4). The partial recombination activity was reported previously for the Trp453Arg RAG2 mutation of OS patient SCID-5,42 whereas the mutated RAG genes of SCID-1 and SCID-3 were shown to have partial recombination activity in our extrachromosomal recombination assay. In line with some remaining recombination activity of the C-terminal mutated RAG2 protein in SCID-3, some SmIgM+ immature B cells were detectable in the BM of this patient (Figures 2 and 3). Consequently, complete and in-frame IGH and IGL rearrangements were detectable in the BM precursor B cells (Table 3). The amino acid substitution in the C-terminus of the RAG2 protein in SCID-3 was located outside the functionally important core domain, but this mutation might result in diminished protein stability, thereby explaining the strongly reduced recombination activity.
Summary of RAG gene mutations, their recombination activity, and effects on the in vivo lymphoid compartment
| Gene . | Mutation . | Recombination activity . | Diagnosis4-150 . | Lymphoid compartment . | ||
|---|---|---|---|---|---|---|
| Precursor B cells in BM . | Immunogenotype . | |||||
| Relative size . | Differentiation arrest . | |||||
| RAG1 | N-terminal truncation | Strongly decreased | OS in SCID-1 | < 2% | Not evaluable | Oligoclonal T cells |
| Arg249His | Normal (polymorphism) | |||||
| Arg404Gln | Absent | T−B−in SCID-7 | No BM available | No Ig rearrangements4-151 | ||
| Lys820Arg | Normal (polymorphism) | |||||
| RAG2 | Gln16 stop | Absent | T−B− in SCID-6 | 57% | Absolute arrest | No Ig rearrangements |
| Codon 247 stop | Absent | T−B− in SCID-2 and -4 | 5%-57%‡ | Absolute arrest | No Ig rearrangements | |
| Trp435Arg | Strongly decreased4-153 | OS in SCID-5 | < 2% | Not evaluable | Oligoclonal T cells | |
| His481Pro | Strongly decreased | T−B− in SCID-3 | 4% | Leakiness | IGH/IGLrearrangements | |
| Gene . | Mutation . | Recombination activity . | Diagnosis4-150 . | Lymphoid compartment . | ||
|---|---|---|---|---|---|---|
| Precursor B cells in BM . | Immunogenotype . | |||||
| Relative size . | Differentiation arrest . | |||||
| RAG1 | N-terminal truncation | Strongly decreased | OS in SCID-1 | < 2% | Not evaluable | Oligoclonal T cells |
| Arg249His | Normal (polymorphism) | |||||
| Arg404Gln | Absent | T−B−in SCID-7 | No BM available | No Ig rearrangements4-151 | ||
| Lys820Arg | Normal (polymorphism) | |||||
| RAG2 | Gln16 stop | Absent | T−B− in SCID-6 | 57% | Absolute arrest | No Ig rearrangements |
| Codon 247 stop | Absent | T−B− in SCID-2 and -4 | 5%-57%‡ | Absolute arrest | No Ig rearrangements | |
| Trp435Arg | Strongly decreased4-153 | OS in SCID-5 | < 2% | Not evaluable | Oligoclonal T cells | |
| His481Pro | Strongly decreased | T−B− in SCID-3 | 4% | Leakiness | IGH/IGLrearrangements | |
The immunophenotype was obtained from PB.
The immunogenotype in SCID-7 was detected in EBV-transformed B-cell lines.
5% within lymphocyte gate in SCID-2.1, 57% in SCID-2.2, and 47% in SCID-4.
The recombination activity in SCID-5 was taken from the literature.42
We found that approximately 99% (97%-100%) of the precursor B-cell compartment in the SCID patients consisted of CyIgμ−precursor B cells (pro-B cells and pre–B-I cells), in contrast to approximately 15% in healthy children. The localization of the virtually complete arrest at the transition between CyIgμ− and CyIgμ+ pre-B cells in all 5 RAG-deficient SCID patients is in line with the essential role of the RAG proteins in initiation of the VDJ recombination process. This contrasts with the leakiness of the B-cell differentiation arrest in patients with X-linked agammaglobulinemia (XLA).28 45 Only in SCID-3 some minor leakiness was seen (3% Ig+ B cells and detectable Ig gene rearrangements), which was clearly related to the low levels of recombination activity. These data show that in RAG-deficient SCID patients the immunophenotypic and immunogenotypic B-cell differentiation arrests are closely linked (Table 4).
As was observed earlier, a small subpopulation of CD34+/CD20+ precursor B cells was detectable within the CD19+ gate in BM from healthy children.28 However, in BM from most SCID patients a substantial CD34+/CD20+/CD19+population could be identified. We observed that the CD34+/CD20+ population is also relatively large in the precursor B-cell compartment of XLA patients, suggesting that down-regulation of CD34 is normally associated with pre-BCR signaling.28
We observed that CD36 coexpressed with the pan B-cell markers CD22, CyCD79a, and CD19 on BM cells in SCID patients, but virtually not in healthy controls. We also detected coexpression of these markers on BM cells of XLA patients. The CD36+/CD22+ cells might represent early myeloid-lymphoid precursor cells, which are detectable in BM of SCID and XLA patients due to the relative increase in early precursor B cells. However, so far we have no explanation for the coexpression of CD36 and the slightly later expressed pan B-cell markers CyCD79a and CD19.
Although it has been shown that OS is caused by mutated RAGgenes with partial recombination activity,22 it is not understood why these patients present with oligoclonal T lymphocytes, in the absence of B lymphocytes. The presence of high serum IgE levels suggests that Ig-producing plasma cells might be present in patients with OS. However, in BM samples from 2 patients with OS (SCID-1 and SCID-5), flow cytometric analysis was impossible because the percentage CD22+/CD36− precursor B cells was less than 2% of lymphocytes, revealing a severe suppression of the B-cell compartment. One would expect OS patients to have the same percentage of precursor B cells as other RAG-deficient SCID patients, but this was not the case in our OS patients. This might at least partly be caused by the relatively high frequency of oligoclonal T cells within the BM lymphocyte gate (73% and 67% in our OS patients).
In conclusion, we observed a complete B-cell differentiation arrest at the pre-BCR checkpoint in the BM of RAG-deficient SCID patients with absence of recombination activity. One patient (SCID-3) showed some SmIgM+ immature B cells, which corresponded with partial recombination activity of the mutated RAG2 protein and the presence of in-frame Ig gene rearrangements. The partial recombination activity in 2 other patients was associated with OS and oligoclonal T cells.
The authors thank Dr H. Karasuyama for making available the monoclonal antibody HSL96 directed against the human VpreB protein, and Miss G. van der Linden and Miss K. Wiertz for technical assistance.
Supported by Revolving Fund project of the University Hospital Rotterdam, The Netherlands.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Jacques J. M. van Dongen, Department of Immunology, Erasmus MC, University Medical Center Rotterdam, dr. Molewaterplein 50, 3015 GE Rotterdam, The Netherlands; e-mail:vandongen@immu.fgg.eur.nl.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal