A precise description of clinical features at presentation and analysis of clinical and biologic prognostic factors in splenic marginal zone lymphoma (SMZL) are still lacking. Here we describe the clinical and biologic features of a series of 60 SMZL patients diagnosed after splenectomy. Analysis for overall survival (OS), failure-free survival (FFS), and the probability of obtaining a response was performed using univariate and multivariate tests. The median age of the patient was 63 years (range, 35-84 years). Performance status according to the Eastern Cooperative Oncology Group (ECOG scale) was 0 = 16%, 1 = 58%, and 2 = 25%. Of the 60 patients, 53 (86.6%) were at Ann Arbor stage IV. All 60 patients received splenectomies, 29 of 60 also received chemotherapy, and 2 received spleen radiotherapy. A complete response (CR) was achieved by 38.3% of patients, and a partial response (PR) was achieved by 55%. Mean OS of the series was 103 months (range, 2-164 months); mean FFS was 40 months (range, 3-164 months). At 5 years from diagnosis, 39 patients (65%) were alive. Patients dying from the disease had a relatively aggressive clinical course, with a short survival (17.5 months [range, 2-72 months]). Significant prognostic factors in multivariate analysis were (1) (for OS and FFS) lack of response to therapy (CR versus noncomplete response [nCR]) and involvement of nonhematopoietic sites, and (2) (for the probability of obtaining CR) bone marrow involvement. Chemotherapy did not influence OS or FFS. p53 overexpression predicted a shorter OS in the univariate analysis. These data confirm the relative indolence of this disease, indicating the existence of a subset of more aggressive cases, which should stimulate the search for predictive biologic factors and alternative therapies.
Introduction
Since the name splenic marginal zone lymphoma (SMZL) was coined by Schmid et al in 1992,1 the characteristics of this entity have been somewhat blurred by its rarity and the lack of precise histological criteria for recognition. This, together with the fact that the name suggests marginal zone derivation, has led to a poor definition of the limits between SMZL and other types of lymphoma that reputedly originate in the marginal zone, such as extranodal marginal zone lymphomas (mucosa-associated lymphoid tissue) and nodal marginal zone lymphomas.2-6 Thus, knowledge of the clinical characteristics of patients with SMZL and the identification of clinical and biologic prognostic parameters has been hindered by the small size of series or the frequent inclusion of patients with other clinicopathological conditions in the SZML series.
This report describes the clinical features, response to therapy, and follow-up of a series of 60 patients. These data have been correlated with the presence of 7q deletion, p53 anomalous overexpression, and growth fraction. The inclusion criterion restricted our series to patients diagnosed after splenectomy, to increase its homogeneity and the accuracy of diagnosis, which has to date been based mainly on the recognition of the characteristic infiltration pattern in the spleen.
A group of patients having a relatively aggressive clinical course with low survival probability has been defined.
Patients and methods
Records at the Department of Pathology Hospital Virgen de la Salud, Toledo, Spain, of 275 splenectomy specimens corresponding to cases diagnosed as non-Hodgkin lymphoma (NHL), from our institution and from consultation cases submitted to the Department of Pathology, were reviewed. Adequate follow-up was obtained in 60 patients diagnosed with SMZL using the criteria defined by Isaacson and Piris.6 All slides from these cases were reviewed by 2 investigators (M.M. and M.A.P.).
The following data were recorded: (1) demographics; (2) symptoms at diagnosis; (3) clinical and biochemical characteristics at diagnosis (location of disease, laboratory data); (4) reason for and date of splenectomy; (5) spleen weight; (6) additional therapies other than surgery (chemotherapy: date, reason for delivery, regime employed, number of courses; radiation therapy: reason for delivery, fields, doses delivered); (7) follow-up data (including CR or PR, date and clinical characteristics of relapse when applicable, rescue therapy); and (8) outcome (date and cause of death when applicable, follow-up time, updated situation).
Histopathology
In all cases the diagnosis of SMZL was made using splenectomy specimens according to previously reported criteria.6Cases with inadequate clinical data, without paraffin-embedded material, or with poor-quality immunohistochemical studies for diagnosis were excluded.
Tissue samples
Immunostaining techniques.
In all cases paraffin and/or frozen slides of splenectomy and bone marrow sections were available. In 11 cases additional biopsies were available (10 peripheral lymph nodes and 1 liver). Tissue biopsy specimens were fixed in B-5 or formalin, routinely processed, and stained with hematoxylin-eosin and Giemsa. Bone marrow biopsy specimens were fixed in B-5, decalcified with ethylenediaminetetra-acetic acid, paraffin-embedded, and sectioned in the usual manner.
Immunohistochemical examination was performed in all cases on formalin-fixed or B-5 paraffin-embedded sections, for diagnostic purposes, with a panel of antibodies including CD20, CD3, CD23, CD43, cyclin D1, bcl2, MIB1, p53, IgD, κλ, and CD5. To summarize, after incubation with the primary antibody, immunodetection was performed with peroxidase-labeled streptavidin biotin (LSAB-DAKO), using diaminobencidine chromogen as substrate. All immunostaining was performed using the TechMate 500 (DAKO, Copenhagen, Denmark) automatic immunostaining device.
The proliferation index was evaluated using the MIB1 antibody (ki67) (Immunotech, Marseille, France). MIB1 staining was quantified in splenic sections using the Quantitative Proliferation Index application of the Computerized Analyzer System (CAS 200, Becton Dickinson, San Jose, CA). Splenic marginal zone areas were selected, focusing in all cases on the areas with the highest growth fraction. Representative fields down to a minimum of 20 000 μ were selected (approximately 4 fields with 45 × objective and 8 × ocular lenses). For statistical analysis, the median value of MIB1 (23) was used to separate different groups.
Monoclonal antibody for p53 (DO7; Novocastra, Newcastle upon Tyne, United Kingdom) was used. Only specimens that showed a distinct reactivity in the majority of tumor cells were considered positive.
Molecular analysis and p53 gene mutations.
del 7q32.
7q31-32 deletion, a relatively specific cytogenetic marker present in 40% of patients with SMZL, was analyzed by loss of heterozygosity and conventional cytogenetic technique; some of these results also have been recently reported.8
Response criteria.
The peculiar clinicobiologic characteristics of SMZL make it difficult to use standard response criteria.9 Other authors have used specific criteria for this lymphoma.2 For these reasons, we used the following criteria to score clinical response: (1) a complete response (CR) consisted of no evidence of disease, including in the bone marrow; (2) a good clinical and hematological response (GHR) consisted of no evidence of active disease (no symptoms, no cytopenia, no lymphocytosis/< 5% lymphocytes/only shown by flow cytometry, bone marrow unknown/< 5% of tumor lymphocytes/only shown by flow cytometry, and no lymph node involvement or extramedullary disease); (3) a stable disease or partial remission consisted of the persistence of any symptom, analytical data, or location of disease as in the initial diagnosis or the failure to fulfill criteria for CR, GHR, or PD; and (4) progressive disease (PD) consisted of the presence of new symptoms or locations of disease, or an increase of 50% or more of blood lymphocyte count or of bone marrow infiltrate, or an increase of 25% or more in the size of previous organomegaly. Transformation to a more aggressive histology was also considered as PD.
Statistics.
All data were analyzed with the SSPS software package (Scientific Software for Professional Statistics, Chicago, IL) and with EPIINFO2000 (World Health Organization, Geneva, Switzerland).
Overall survival (OS) was defined as the time elapsed from diagnosis to death or last follow-up. Failure-free survival (FFS) was defined as the time from onset of the therapy to the date of first relapse or progression of disease, death from any cause, or loss of follow-up. Follow-up evaluation of patients who did not experience one of these events was censored at the date of last contact. The definition used here fit well into the criteria defined to standardize clinical response in NHL.9
Univariate and multivariate analyses were used to identify the prognostic factors that might influence OS, FFS, and response to therapy.
Univariate analysis.
OS and FFS curves were estimated by the Kaplan-Meier method. The univariate association between individual clinical features and OS and FFS was determined using the log-rank test. Cox proportional hazards univariate analysis was also performed independently for each variable to calculate the relative risk for OS and FSS, as well as the confidence intervals (CIs). The analysis of complete response was performed using the chi-square of Fisher exact tests for categorical variables and the Student t or Mann-Whitney tests for continuous variables.
Multivariate analysis.
Cox stepwise proportional hazards model was used to identify the factors that might significantly influence OS and FFS. The logistic regression model was used for CR. All variables withP ≤ .05 or that were considered clinical or biologically relevant were included in the multivariate analysis.
In all of the above-mentioned analyses, 2-sided Pvalues ≤ .05 were considered statistically significant.
The variables analyzed were age (≤ 60 vs > 60 years), lactate dehydrogenase (≤ normal vs > normal), peripheral lymph nodes (no vs yes), bone marrow and hepatic involvement (no vs yes), spleen weight, performance status (ECOG 0-1 vs 2-3), involvement of nonhematopoietic sites (other than spleen, liver, bone marrow, or lymph nodes) (0 vs ≥ 1), Mib1 (≤ 23 vs > 23), p53 immunostaining (+ve vs −ve), and 7q deletion (no vs yes). Initially, clinical stage (Ann Arbor stage I-II vs III-IV) was to be included as another variable. However, given that most patients from this series had stage IV disease (86.6%), clinical stage should be ruled out as a variable in the analysis of prognostic factors, although it has been included in the descriptive analysis.
Results
Clinical findings
Patient population.
A total of 60 patients were considered to fit the diagnostic criteria for SMZL. There were 38 (63%) male and 22 (37%) female patients. Median age was 63 years (range, 35-84 years). Of the 60 patients, 10 (16.6%) had ECOG 0 at diagnosis, 35 (58.3%) had ECOG 1, and 15 (25%) had ECOG 2.
Symptoms at diagnosis.
The presence of splenomegaly was recorded as the most frequent symptom at diagnosis (in 73% of patients). General symptoms (in 58% of patients) and abdominal discomfort or pain (in 33% of patients) were the next most frequent symptoms. The disease was diagnosed as a casual finding in one case (2% of patients). A summary of all symptoms at diagnosis is shown in Table1.
Signs and symptoms of SMZL
| Sign/symptom . | n . | % . |
|---|---|---|
| Splenomegaly | 44 | 73 |
| B symptoms | 35 | 58 |
| Abdominal pain | 20 | 33 |
| Anemia | 17 | 28 |
| Thrombocytopenia | 13 | 22 |
| Leucocytosis | 8 | 13 |
| AIHA | 8 | 13 |
| Other reasons | 6 | 10 |
| Infections | 5 | 8 |
| Casual finding | 1 | 2 |
| Sign/symptom . | n . | % . |
|---|---|---|
| Splenomegaly | 44 | 73 |
| B symptoms | 35 | 58 |
| Abdominal pain | 20 | 33 |
| Anemia | 17 | 28 |
| Thrombocytopenia | 13 | 22 |
| Leucocytosis | 8 | 13 |
| AIHA | 8 | 13 |
| Other reasons | 6 | 10 |
| Infections | 5 | 8 |
| Casual finding | 1 | 2 |
The sum of percentages is greater than 100 because most patients showed more than 2 signs or symptoms at diagnosis.
AIHA indicates autoimmune hemolytic anemia.
Location of disease at diagnosis.
Of the patients, 50 (83%) had bone marrow involvement and 19 (31%) had liver involvement. Tumor involvement of peripheral blood (defined as the presence of absolute lymphocytosis or > 5% of tumor lymphocytes in peripheral blood) was detected in 42 patients (68%). All disease locations are shown in Table2. Because of the high frequency of bone marrow or liver involvement, most patients in the series were Ann Arbor stage IV (52; 86.6%) (Table3).
Location of disease at diagnosis
| Location . | n (%) . |
|---|---|
| Spleen | 60 (100) |
| Bone marrow | 50 (83) |
| Liver | 19 (31) |
| Peripheral blood | 39 (65) |
| Abdominal lymphadenopathies | 15 (25) |
| Mediastinal lymphadenopathies | 2 (3) |
| Peripheral lymphadenopathies | 10 (17) |
| Involvement of nonhematopoietic sites | 4 (6.6) |
| Location . | n (%) . |
|---|---|
| Spleen | 60 (100) |
| Bone marrow | 50 (83) |
| Liver | 19 (31) |
| Peripheral blood | 39 (65) |
| Abdominal lymphadenopathies | 15 (25) |
| Mediastinal lymphadenopathies | 2 (3) |
| Peripheral lymphadenopathies | 10 (17) |
| Involvement of nonhematopoietic sites | 4 (6.6) |
Biologic and laboratory characteristics.
Data from the whole series are shown in Table4. Data concerning the presence of paraprotein were obtained from only 40 patients (66%). Of these, 35 (87%) had no paraprotein; 4 (10%) had an IgM monoclonal paraprotein, and 1 (3%) had an IgG kappa paraprotein.
Biochemical and laboratory characteristics
| Parameter . | n (%) . | Range . | Median . |
|---|---|---|---|
| Hemoglobin level, g/dL | 5 -15 | 10.91 | |
| Lower than or equal to 110 | 17 (28.3) | ||
| Higher than 110 | 43 (71.6) | ||
| Platelet count, × 109 | 25-390 | 143 | |
| Lower than or equal to 150 | 13 (21.6) | ||
| Higher than 150 | 47 (78.4) | ||
| Leukocyte count, × 106 | 1 270 -84 000 | 12 300 | |
| Lower than or equal to 4 | 18 (30) | ||
| Higher than 4 | 42 (70) | ||
| Lymphocyte count, × 106 | 150 -75 000 | 8 480 | |
| Absolute lymphocytosis | 35 (58.3) | ||
| LDH level | 197 -1 655 | 498 | |
| Lower than or equal to 480 | 30 | ||
| Higher than 480 | 20 | ||
| Spleen weight, g | 480 -5 360 | 1 650 |
| Parameter . | n (%) . | Range . | Median . |
|---|---|---|---|
| Hemoglobin level, g/dL | 5 -15 | 10.91 | |
| Lower than or equal to 110 | 17 (28.3) | ||
| Higher than 110 | 43 (71.6) | ||
| Platelet count, × 109 | 25-390 | 143 | |
| Lower than or equal to 150 | 13 (21.6) | ||
| Higher than 150 | 47 (78.4) | ||
| Leukocyte count, × 106 | 1 270 -84 000 | 12 300 | |
| Lower than or equal to 4 | 18 (30) | ||
| Higher than 4 | 42 (70) | ||
| Lymphocyte count, × 106 | 150 -75 000 | 8 480 | |
| Absolute lymphocytosis | 35 (58.3) | ||
| LDH level | 197 -1 655 | 498 | |
| Lower than or equal to 480 | 30 | ||
| Higher than 480 | 20 | ||
| Spleen weight, g | 480 -5 360 | 1 650 |
Immunohistochemical and cytogenetic findings
MIB1 immunostaining was available in 52 cases, and the percentage of positive cells staining varied from 2 to 47 (median, 23).
The deletion of 7q31-32 was studied in 32 cases. This alteration was present in 10 cases (31.2%).
p53 expression was investigated in 43 cases and was positive in 5 cases. All positive cases were characterized by strong p53 expression in the majority of tumor cells, with concomitant absence of p21. In 2 of these cases the p53 gene mutation was confirmed by molecular studies (Table 5).
Biological and cytogenetic data
| Molecular data . | n (%) . |
|---|---|
| Mib1 | |
| Less than or equal to 23 | 26 (50) |
| More than 23 | 26 (50) |
| P53 | |
| Negative | 38 (88) |
| Positive | 5 (12) |
| 7q deletion | |
| No | 22 (69) |
| Yes | 10 (31) |
| Molecular data . | n (%) . |
|---|---|
| Mib1 | |
| Less than or equal to 23 | 26 (50) |
| More than 23 | 26 (50) |
| P53 | |
| Negative | 38 (88) |
| Positive | 5 (12) |
| 7q deletion | |
| No | 22 (69) |
| Yes | 10 (31) |
Therapy and outcome
Therapy.
Obviously, all patients underwent splenectomy, as this was an inclusion criterion for the study. In most of them (51; 85%) splenectomy was performed for diagnostic purposes (Table6). In 29 patients (48.3%) chemotherapy was received apart from splenectomy. Of these, 12 (41%) received CHOP-like chemotherapy, 10 (34%) received clorambucil-prednisone, and 7 (24%) received other chemotherapy combinations. Only 2 patients received splenic irradiation.
Therapy received
| Therapy . | n (%) . | CR (%) . |
|---|---|---|
| Splenectomy only | 29 (48.3) | |
| Splenectomy + chemotherapy | 29 (48.3) | |
| CHOP-like | 12 (20) | 8 of 20 (67) |
| Clorambucil-prednisone | 10 (16.7) | 5 of 10 (50) |
| Others | 7 (11.7) | 1 of 7 (14) |
| Radiation therapy on spleen6-150 | 2 (3.3) |
| Therapy . | n (%) . | CR (%) . |
|---|---|---|
| Splenectomy only | 29 (48.3) | |
| Splenectomy + chemotherapy | 29 (48.3) | |
| CHOP-like | 12 (20) | 8 of 20 (67) |
| Clorambucil-prednisone | 10 (16.7) | 5 of 10 (50) |
| Others | 7 (11.7) | 1 of 7 (14) |
| Radiation therapy on spleen6-150 | 2 (3.3) |
Delivered before splenectomy.
Outcome.
The number of patients reaching CR after therapy was 23 (38.3%); GHR, 25 (41.7%); and PR, 8 (13.3%). The percentages of CR attained with each chemotherapy regimen (pooled in 3 groups) are shown in Table 6. Also, 4 patients (6.7%) had an early death (< 3 months after diagnosis), and 8 patients (13.3%) underwent transformation to high-grade B-cell lymphoma.
Follow-up
The median time of follow-up in the whole series was 32 months (range, 2-162 months). Only one patient was lost for follow-up at 13 months. When analysis was performed, 18 patients (39%) were alive without disease, 22 (36.7%) were alive with disease, 16 (26.7%) had died because of the disease, 3 (5%) had died from other causes, and 1 (1.7%) was lost for follow-up.
Survival
OS.
Mean survival time for the whole series was 103 months (8.5 years), with a range from 2 to 164 months. Median survival was not reached at the moment of analysis. At 5 years from diagnosis, 39 patients (65%) were alive. In sharp contrast with this favorable survival for the group as a whole, patients who died from the lymphoma had a much lower median survival (median, 17.5 months [1.4 years]; range, 2-72 months).
FFS.
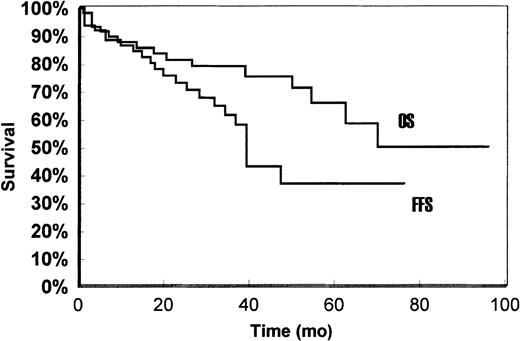
Median FFS time was 40 months (3.3 years) for the whole series (range, 3-164 months). Both curves are shown in Figure1.
The stratification of OS and FFS between different groups is shown under “Prognostic factors.”
Prognostic factors
Prognostic factors that may influence OS, FFS, response to therapy, and risk of relapse were investigated. The variables analyzed are shown in “Patients and methods.”
Univariate analysis
OS.
Four factors were found to be associated with poorer survival: failure to obtain CR, involvement of nonhematopoietic sites at diagnosis, high ECOG score at diagnosis, and p53 expression (Table7).
Prognostic factors for OS (Cox univariate analysis)
| Variable . | RL . | RR . | CI 95% . | P . |
|---|---|---|---|---|
| Age | ≤ 65 | 3.87 | 1.27 -11.77 | .16 |
| Sex | Female | 2.08 | 0.77 -5.6 | .14 |
| LDH | Normal | 0.63 | 0.19 -2.07 | .45 |
| ECOG (2-3) | 0-1 | 4.11 | 1.46 -11.55 | .0074 |
| Bone marrow involvement | Absent | 0.95 | 0.21 -4.23 | .95 |
| Liver involvement | Absent | 4.11 | 1.46 -11.55 | .08 |
| Involvement of nonhematopoietic sites | Absent | 3.54 | 0.99 -12.7 | .05 |
| Nodal involvement | Absent | 1.84 | 0.68 -5.00 | .22 |
| Response to therapy | Complete | 9.80 | 1.25 -76.36 | .029 |
| Chemotherapy | ||||
| 1 | 0 | 1:0.83 | 0.20 -3.41 | .79 |
| 2 | 0 | 2:1.08 | 0.26 -4.43 | .90 |
| 3 | 0 | 3:2.00 | 0.55 -7.20 | .28 |
| Mib-1 | ≤ 23 | 1.02 | 0.28 -3.60 | .97 |
| p53 | Negative | 4.93 | 1.46 -16.66 | .01 |
| del7q | Positive | 1.42 | 0.35 -5.37 | .6 |
| Variable . | RL . | RR . | CI 95% . | P . |
|---|---|---|---|---|
| Age | ≤ 65 | 3.87 | 1.27 -11.77 | .16 |
| Sex | Female | 2.08 | 0.77 -5.6 | .14 |
| LDH | Normal | 0.63 | 0.19 -2.07 | .45 |
| ECOG (2-3) | 0-1 | 4.11 | 1.46 -11.55 | .0074 |
| Bone marrow involvement | Absent | 0.95 | 0.21 -4.23 | .95 |
| Liver involvement | Absent | 4.11 | 1.46 -11.55 | .08 |
| Involvement of nonhematopoietic sites | Absent | 3.54 | 0.99 -12.7 | .05 |
| Nodal involvement | Absent | 1.84 | 0.68 -5.00 | .22 |
| Response to therapy | Complete | 9.80 | 1.25 -76.36 | .029 |
| Chemotherapy | ||||
| 1 | 0 | 1:0.83 | 0.20 -3.41 | .79 |
| 2 | 0 | 2:1.08 | 0.26 -4.43 | .90 |
| 3 | 0 | 3:2.00 | 0.55 -7.20 | .28 |
| Mib-1 | ≤ 23 | 1.02 | 0.28 -3.60 | .97 |
| p53 | Negative | 4.93 | 1.46 -16.66 | .01 |
| del7q | Positive | 1.42 | 0.35 -5.37 | .6 |
For chemotherapy, 0 indicates no chemotherapy; 1, CHOP-like; 2, clorambucil-prednisone; and 3, other.
RL indicates reference level; RR, relative risk; CI, confidence interval.
Response to therapy.
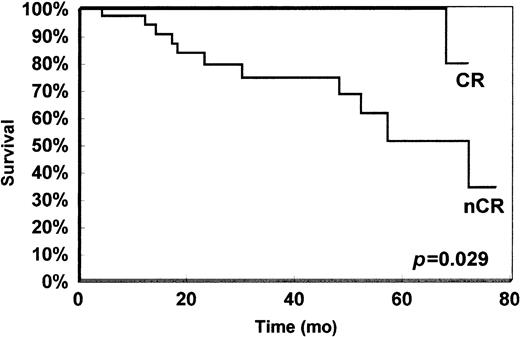
Patients who attained CR had a mean survival of 145 months (12 years; median not reached), whereas patients with GHR and PR had a median survival of 57 and 72 months, respectively (log-rankP < .0273). Given that no significant differences were found between GHR and PR, response was aggregated in 2 groups here for the rest of the analysis: complete response (CR) and noncomplete response (nCR). When they were pooled, statistically significant differences remained between complete responders and noncomplete responders (Figure 2).
Survival of patients who obtained complete response (CR) and noncomplete response (nCR).
Survival of patients who obtained complete response (CR) and noncomplete response (nCR).
Involvement of nonhematopoietic sites.
Infiltration of organs other than liver, spleen, lymph node, or bone marrow occurred in 4 patients (6.6%). Their median survival time was 52 months (4.3 years), compared with a median survival not yet reached (mean, 113 months [9.4 years]) for patients without involvement of nonhematopoietic organs (log-rank,P = .05).
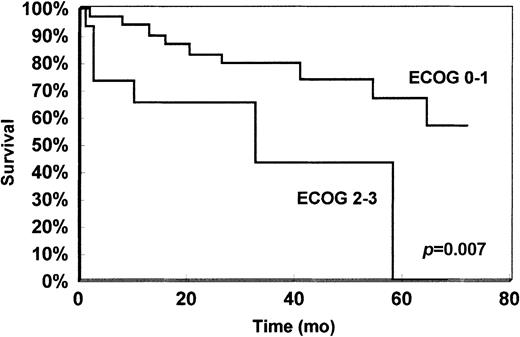
ECOG.
The 4 groups of the ECOG score could not be separated, because no patient with ECOG 0 died, and there was only one patient with ECOG 3; analysis was therefore performed by comparing ECOG 0-1 versus ECOG 2-3. Differences in survival between these 2 groups were statistically significant (log-rank, P = .007) (Figure3).
Survival of patients with performance status ECOG 0-1 versus 2-3 at diagnosis.
Other variables.
No other variable had significant impact on OS. Surprisingly, bone marrow involvement did not reach statistical significance (log-rank,P = .95) as a prognostic factor in univariate analysis. This was also the case for liver involvement (P = .89).
Statistical analysis of the impact of the type of chemotherapy delivered on OS was carried out by grouping chemotherapy as shown in Table 6. Previously, survival of patients who had received chemotherapy of any type was compared with that of patients not receiving chemotherapy in the attempt to find confounding factors (clinical aggressiveness, age, staging). No statistically significant differences could be identified between the survival probability of both groups (chemotherapy and nonchemotherapy receivers), nor were any differences found when types of chemotherapy were compared (log-rank,P = .62). Additionally, no significant difference could be found when grouping patients receiving chemotherapy in CHOP and non-CHOP regimens. Although patients receiving CHOP had a mean OS longer than those receiving non-CHOP chemotherapy (128 months versus 72 months, respectively), these differences did not attain statistical significance (log-rank, P = .72).
FFS.
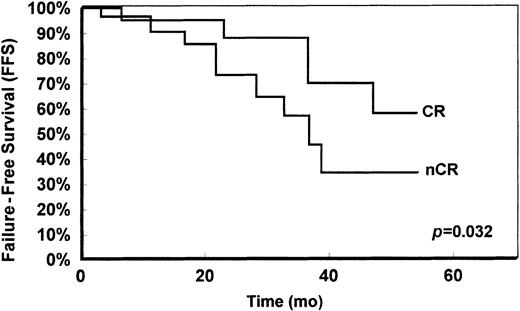
There were 2 factors found to impact negatively on FFS: liver involvement (P = .043) and response to therapy (Table8). Patients who obtained CR had a median FFS yet to be reached, with a mean FFS of 113 months (9.4 years), whereas noncomplete responders had a median FFS of 37 months (3.1 years) (log-rank, P = .032) (Figure4).
Prognostic factors for FFS (Cox univariate analysis)
| Variable . | RL . | RR . | CI 95% . | P . |
|---|---|---|---|---|
| Age | ≤ 65 | 1.36 | 0.55 -3.34 | .49 |
| Sex | Female | 0.83 | 0.32 -2.17 | .76 |
| LDH | Normal | 1.27 | 0.48 -3.32 | .61 |
| ECOG (2-3) | 0-1 | 1.84 | 0.65 -5.15 | .24 |
| Bone marrow involvement8-150 | ||||
| Liver involvement | Absent | 2.48 | 1.02 -6.03 | .043 |
| Involvement of nonhematopoietic sites | Absent | 2.21 | 0.50 -9.62 | .209 |
| Nodal involvement | Absent | 1.66 | 0.68 -4.03 | .26 |
| Response to therapy | ||||
| Noncomplete | Complete | 3.22 | 1.04 -9.98 | .032 |
| Chemotherapy | ||||
| 1 | 0 | 1.13 | 0.38 -3.37 | .82 |
| 2 | 0 | 0.54 | 0.11 -2.62 | .44 |
| 3 | 0 | 1.49 | 0.44 -5.06 | .51 |
| Mib-1 | ≤ 23 | 1.19 | 0.39 -3.59 | .75 |
| p53 | Negative | 2.43 | 0.54 -11.55 | .26 |
| del7q | Positive | 2.28 | 0.68 -7.64 | .17 |
| Variable . | RL . | RR . | CI 95% . | P . |
|---|---|---|---|---|
| Age | ≤ 65 | 1.36 | 0.55 -3.34 | .49 |
| Sex | Female | 0.83 | 0.32 -2.17 | .76 |
| LDH | Normal | 1.27 | 0.48 -3.32 | .61 |
| ECOG (2-3) | 0-1 | 1.84 | 0.65 -5.15 | .24 |
| Bone marrow involvement8-150 | ||||
| Liver involvement | Absent | 2.48 | 1.02 -6.03 | .043 |
| Involvement of nonhematopoietic sites | Absent | 2.21 | 0.50 -9.62 | .209 |
| Nodal involvement | Absent | 1.66 | 0.68 -4.03 | .26 |
| Response to therapy | ||||
| Noncomplete | Complete | 3.22 | 1.04 -9.98 | .032 |
| Chemotherapy | ||||
| 1 | 0 | 1.13 | 0.38 -3.37 | .82 |
| 2 | 0 | 0.54 | 0.11 -2.62 | .44 |
| 3 | 0 | 1.49 | 0.44 -5.06 | .51 |
| Mib-1 | ≤ 23 | 1.19 | 0.39 -3.59 | .75 |
| p53 | Negative | 2.43 | 0.54 -11.55 | .26 |
| del7q | Positive | 2.28 | 0.68 -7.64 | .17 |
For Chemotherapy, 0 indicates no chemotherapy; 1, CHOP-like; 2, clorambucil-prednisone; 3, other.
RL indicates reference level; RR, relative risk; CI, confidence interval.
Bone marrow could not be analyzed because of colinearity (see text).
FFS of patients obtaining complete response (CR) and noncomplete response (nCR).
Bone marrow involvement could not be analyzed because of colinearity, as no patient without bone marrow involvement was classified as failed.
Probability of obtaining response.
Of the analyzed variables, only bone marrow involvement was statistically significant (Fisher exact text; P = .037) for the probability of obtaining response.
Multivariate analysis
OS.
Only response to therapy (CR vs nCR; P = .026) and the presence of involvement of nonhematopoietic sites (P = .05) remained independently significant as factors associated with OS probability (Table9).
Multivariate analysis
| Variable . | RL . | RR . | CI (95%) . | P . |
|---|---|---|---|---|
| Overall survival9-150 | ||||
| Response to therapy | Complete | 0.089 | 0.011 -0.716 | .026 |
| Involvement of nonhematopoietic sites | Absent | 4.676 | 0.962 -22.74 | .05 |
| Failure-free survival9-151 | ||||
| Response to therapy | ||||
| Noncomplete | Complete | 3.935 | 1.202 -12.877 | .023 |
| Involvement of nonhematopoietic sites | Absent | 4.901 | 1.001 -23.895 | .049 |
| Probability to obtain CR | ||||
| Bone marrow involvement | Absent | 0.172 | 0.031 -0.951 | .043 |
| Variable . | RL . | RR . | CI (95%) . | P . |
|---|---|---|---|---|
| Overall survival9-150 | ||||
| Response to therapy | Complete | 0.089 | 0.011 -0.716 | .026 |
| Involvement of nonhematopoietic sites | Absent | 4.676 | 0.962 -22.74 | .05 |
| Failure-free survival9-151 | ||||
| Response to therapy | ||||
| Noncomplete | Complete | 3.935 | 1.202 -12.877 | .023 |
| Involvement of nonhematopoietic sites | Absent | 4.901 | 1.001 -23.895 | .049 |
| Probability to obtain CR | ||||
| Bone marrow involvement | Absent | 0.172 | 0.031 -0.951 | .043 |
Prognostic factors independently associated with OS, FFS, and the probability of obtaining CR (Cox stepwise proportional hazards model).
RL indicates reference level; RR, relative risk; and CI, confidence interval.
Model χ2: 10.9; P = .006.
Model χ2: 21.54; P = .0001.
FFS.
The same factors as in OS retained independent significance as factors conditioning FFS: response to therapy (CR vs nCR;P = .023) and involvement of nonhematopoietic sites (P = .049).
Probability of obtaining CR.
Bone marrow involvement was the only variable independently associated with the probability of obtaining CR. Patients with bone marrow involvement had a significantly lower percentage of CR than those without bone marrow involvement (P = .043).
Relapse and progression pattern
Twenty patients who had obtained CR or some kind of response (GHR or PR) relapsed (if CR had been reached) or had progressive disease (nCR patients). Of 23 patients with CR, 5 (21.7%) relapsed, and 15 of 33 (45.4%) patients with nCR progressed. Both relapse and progression were grouped as failure for analysis purposes.
The most frequent site of failure was peripheral lymph nodes (75% of failures), followed by abdominal lymph nodes (50%), peripheral blood (40%), bone marrow (35%), and liver (25%). As a whole, 17 of 20 patients who failed (85%) had a lymphatic site as the location of failure. Of these patients, 4 (20% of all failures) showed mediastinal lymph nodes.
Discussion
Splenic marginal zone lymphoma is a relatively rare entity, and just a few hundred cases have been previously reported in the literature before this series. Three series with a significant number of cases apart from this one have been reported: Mulligan et al2 report 50 cases; Troussard et al, 100 cases3; and recently, Berger et al have reported 124 cases,5 although this series groups SMZL and other lymphoma types. However, in the series by Mulligan and Troussard diagnosis was carried out on the basis of the presence of villous lymphocytes in peripheral blood smears, and consequently cases are reported as splenic marginal lymphoma with villous lymphocytes (SLVL). Although many authors consider that this entity actually corresponds to SMZL,4,6 the fact is that villous lymphocytes may appear in peripheral blood not only in SMZL, but also in mantle cell lymphomas (MCL)10 (in this case bearing the translocation t(11;14) and bcl-1 rearrangement, both of which are characteristics of MCL11) and follicular lymphoma.6 Given that in the series by Mulligan and Troussard 36 of 50 patients and 28 of 100 underwent splenectomy, respectively, some doubts might be raised about whether all the cases collected in these series actually represent the same entity. All the other published series contain a low number of cases (from 3 to 14). In this respect, it is interesting that in our series all patients with peripheral blood expression had bone marrow involvement. However, 11 of 50 patients (22%) with bone marrow involvement had no expression in peripheral blood. This might suggest that, for practical purposes, peripheral blood smear is an insufficient diagnostic method and may exclude a significant proportion of patients. Finally, because of the rarity of SMZL, all of the published series on SMZL are necessarily retrospective, which is an additional difficulty for the analysis of prognostic factors and for establishing the optimal therapy for this disease.
For these reasons, the importance of this revision is that all patients were standardized by a common criterion: to be included it was necessary that splenectomy had been performed previously and that spleen samples were readily accessible to the investigators. This fact enabled us to perform analysis on a quite homogeneous population (all patients had received the same therapy on entrance in the study), which, at least as a starting point, should make it possible to reach more confident conclusions.
Little is known about the prognostic factors that determine outcome or survival in SMZL, and only 2 series apart from this one report on them.3,5 In the series by Troussard,3lymphocyte count, leukocyte count, and the use of chemotherapy as the initial treatment impacted negatively and in a statistically significant way on survival in multivariate analysis. However, this was not the case for any of these factors in our series. Similarly, in the series by Berger et al5 none of the parameters studied was associated with poorer survival. In our series, lack of response to therapy (complete versus noncomplete response) and involvement of nonhematopoietic sites were the 2 factors that impacted negatively on OS in multivariate analysis. The importance of response to therapy in our series is in sharp contrast with the results of Troussard et al.3 In their series, chemotherapy is a negative factor for OS. They explain the negative influence of chemotherapy on OS because this disease mainly affects an elderly population and they deduce that the unfavorable effect of chemotherapy on survival could be attributed to the toxicity of chemotherapy. An alternative interpretation is that patients selected for chemotherapy present with a more aggressive disease than those treated exclusively with splenectomy. However, this question can be addressed only by well-designed randomized prospective trials, which would be difficult to set up because of the rarity of the disease.
In Berger et al's series the involvement of nonhematopoietic sites had no prognostic significance, whereas in ours it impacted significantly not only on OS, but also on FFS (Table 9). It should be emphasized that we considered nonhematopoietic sites of involvement to be sites other than spleen, lymph node, bone marrow, or liver. We made this consideration because bone marrow and liver infiltration are so frequently reported in SMZL that their involvement may conceivably be considered to be a natural evolution of the disease. On the contrary, the involvement of other extranodal locations is rare and may reflect a more aggressive disease, as the results of this series support.
In our series, 5 patients had p53 (+) disease. Of these, 4 died because of the disease, with a median survival of only 17 months. Indeed, p53 mutation impacted significantly on OS in univariate analysis (P = .01), although it retained no significance in multivariate analysis. p53 mutations have been proposed as a marker of aggressive transformation or refractoriness to therapy.12,13 In this sense, the results from Baldini et al12 are similar to ours. However, in that series of 15 patients, the disease in 4 of the 5 p53-mutated patients evolved into aggressive, fatal NHL, whereas in our series the disease in only 1 of 5 p53 (+) patients did so. In spite of this, the median survival of these 5 patients was far lower than that of the series as a whole. Similar results have more recently been found by Gruszka-Westwood et al,13 showing an adverse effect of p53 alterations in the clinical behavior of SLVL patients.
Another biologic factor explored in this series was the frequency of 7q loss. This is the most frequent cytogenetic abnormality that has been found to be relatively specific for SMZL.8 This study fails to show a clear prognostic value for this alteration, although this could be dependent on the relatively small size of the series included here.
Finally, no intent has been made to correlate clinical behavior in this series with the presence of somatic mutation in the IgHV genes, which is now recognized to constitute a favorable prognostic marker in both B-cell chronic lymphocytic lymphoma (B-CLL) and SMZL.14
To our knowledge, no series has previously described the failure pattern of the disease. We have noted some quite interesting findings in connection with this. One of the most remarkable is that 85% of patients with relapsed or progressive disease have nodal involvement, a surprising finding given the relatively low frequency of nodal involvement at initial diagnosis (Table 2). This emphasizes the prudence of separating nodal involvement by SMZL from primary nodal MZL, a differential diagnosis for which additional molecular markers are urgently required.
The treatment of SMZL is also controversial. In all large series a significant group of patients received no therapy.2,3,5These patients do not seem to do worse than those initially treated. For these reasons, and assuming that SMZL is an indolent disease, some recommend a “wait and see” conservative therapeutic approach. However, the data from this series introduce a caveat to this approach. Although in general SMZL behaves as an indolent disease, there is a significant group of patients who died from the disease in a relatively short interval of time (median survival was 1.4 years versus 8.5 years for the whole series). Unfortunately, to date we have no means of identifying in advance which patients will have an unfavorable outcome, with the exception of p53 overexpression, which is present only in a limited number of cases. These data seem to be in agreement with the proposal of Mulligan et al,2 who recommend splenectomy whenever it is feasible and when there is cytopenia or other indications for the procedure. Splenectomy has the additional advantage of making a more precise diagnosis possible, excluding other lymphoma types such as MCL or follicular lymphoma, which are characterized by a different clinical evolution. Moreover, other authors have noted that splenectomy has a beneficial effect, with reduction or disappearance of atypical circulating cells or monoclonal bands.15
The role of chemotherapy is still a matter of debate. One of the striking findings in this series is the relatively low percentage (38%) of patients who attain CR after chemotherapy. This is in agreement with the report by Berger et al,5 who found that bone marrow involvement at diagnosis persists after chemotherapy. To date no prospective study has compared diverse chemotherapy regimens for SMZL. In the series published, one of the most commonly used is CHOP, which in our series seems to be associated with a longer OS, although this finding lacks any statistical significance. However, no differences were found in OS between patients receiving and not receiving chemotherapy. Because of this, chemotherapy should probably be reserved for use with progression or relapse of the disease.
Other options have been recently proposed for the treatment of SMZL, such as fludarabine.15 Although this needs to be explored in prospective analysis in larger series of patients, initial results in short series seem to be promising.16
To summarize, the data from this series confirm the relative indolence of this disease and also show the existence of a subset of cases characterized by a more aggressive disease course, which should stimulate the search for clinical or biologic markers that might make it possible to distinguish between these different clinical outcomes.
Supported by grants FIS no. 99/0705 and no. 01/0035 from the Fondo de Investigaciones Sanitarias, Ministerio de Sanidad y Consumo; and by grant no. 1FD97-0431 from the Comision Interministerial de Ciencia y Tecnologı́a, Spain.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Miguel A. Piris, Programa de Patologı́a Molecular, Centro Nacional de Investigaciones Oncológicas, Melchor Fernández Almagro, 3, Madrid 28029, Spain; e-mail:mapiris@cnio.es.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal