Abstract
Matrix metalloproteinase 2 (MMP2) has been reported to be secreted by collagen-stimulated platelets, and active MMP2 has been shown to play a role in platelet aggregation. It has been demonstrated that MMP2 activation is dependent on the complex (membrane type 1 [MT1]-MMP/tissue inhibitor of MMP2 [TIMP2]) receptor and MMP2. We have investigated human platelets as a possible source of MT1-MMP, and we have studied its role in MMP2 activation and in platelet aggregation. Gelatin zymograms showed the existence of MMP2 at proforms (68 kd) and activated-enzyme forms (62-59 kd) in supernatants of resting and activated platelets, respectively. No gelatinolytic activity was associated with the platelet pellet after aggregation, suggesting a total release of MMP2 during cell activation. By Western blot analysis in nonreduced conditions, MT1-MMP was found on resting platelet membranes in 2 forms–the inactive 45-kd form and an apparent 89-kd form, which totally disappeared under reduced conditions. After platelet degranulation, only the 45-kd form was detected. Reverse transcription–polymerase chain reaction experiments showed the expression in platelets of messenger RNA encoding for MMP2, MT1-MMP, and TIMP2. Flow cytometry analysis showed that MT1-MMP, MMP2, and TIMP2 expressions were enhanced at the activated platelet surface. MMP inhibitors, recombinant TIMP2, and synthetic BB94 inhibited collagen-induced platelet aggregation in a concentration-dependent manner, indicating the role of activated MT1-MMP in the modulation of platelet function. In conclusion, our results demonstrate the expression of the trimolecular complex components (MT1-MMP/TIMP2/MMP2) by blood platelets as well as the ability of MMP inhibitors to modulate the aggregating response.
Introduction
Remodeling of the extracellular matrix plays a critical role in the reorganization of connective tissue under both normal and pathophysiologic conditions. Extracellular matrix turnover is initiated by proteolytic enzymes, mainly by serine proteinases of the plasminogen system and matrix metalloproteinases (MMPs).1 MMPs are a family of related proteinases whose principal function appears to be the breakdown of extracellular matrix proteins during processes of tissue remodeling associated with growth, development, and repair. Several MMPs are expressed in cancers at levels that are higher than those found in normal tissue or benign adenomas. It has been suggested that MMPs and tissue inhibitors of metalloproteinase (TIMPs) in circulating body fluids may contribute to the regulation of tumor metastasis, invasion, and angiogenesis.2,3 Recent studies have shown that the MMP2:TIMP2 ratio could be a predictor of invasion, metastasis, and recurrence in urothelial4 and in prostate cancer patients.5 In addition, an increasing number of studies of MMPs in soluble form—detected and measured in plasma and serum—are being carried out to help in the prognosis of various diseases. The purpose of these studies is to correlate MMP serum levels to pathologic clinical features. Overexpression in human tissues of MMP2 by tumor and stromal cells can be correlated with invasive and metastatic behaviors of tumors and with poor prognosis. Furthermore, MMP2 plasma levels were used as markers of liver disease in chronic hepatitis C6and were correlated with histologic stages of hepatitis.7High levels of membrane type 1 (MT1)-MMP, the MMP2 physiologic activator, is associated with invasiveness of certain cancers.8-11 Moreover, MT1-MMP messenger RNA (mRNA) was found highly expressed in urothelial carcinomas compared with its expression in normal urothelial mucosa.12 MMP2 is the most abundant MMP, constitutively secreted in a latent form by many cell types of mesenchymal origin.13 MMP2 is unique among MMPs in that its proform is not activated by enzymatic digestion with exogenous proteinases such as urokinase, plasmin, plasma kallikrein, elastase, or cathepsin G, the putative physiologic activators of other pro-MMPs.14 MMP2 is synthesized and secreted as a zymogen and is activated on the cell surface by 3 different recently discovered MT-MMPs.15-17 Apart from the common and conserved typical MMP structure, these membrane-bound MMPs have a transmembrane domain at the C-terminus. Although MT2-MMP and MT3-MMP were also shown to activate pro-MMP2, MT1-MMP is the one with the best documented correlation to the invasive phenotype of different types of cancer, as is active MMP2. The expression of MT1-MMP has been studied in many cell types and is well correlated with activation of pro-MMP2.9-11,18 The role of MT1-MMP in pro-MMP2 activation through TIMP2 complex formation is now recognized.19 In addition, TIMP2 has recently been proposed as a regulator of pro-MMP2 activation, by limiting the TIMP2/MT1-MMP receptor complex formation.20 Excess or default of TIMP2 are both inhibitory for MMP2 activation.21 22
Blood platelets, principal cells of primary hemostasis, play major roles in thrombosis, clot lysis, atherosclerosis, metastasis, and inflammation. At the site of vessel injury, platelets become activated and release several mediators that modify tissue integrity. They may be considered secreting cells, and their ability to release proteinases during activation was recently emphasized.23 It is well known that interactions between soluble molecules and platelets result in a clot formation, but platelets have also been shown to facilitate metastasis by interacting with tumor cells. Interestingly, it was shown that tumor cells, able to cause metastasis in vivo, had the ability in vitro to induce platelet aggregation.24 To date, only 2 papers have reported a relationship between gelatinase secretion and human platelets. One paper described tumor cells' ability to induce in vitro platelet aggregation and showed that platelets could stimulate tumor cells to secrete MMPs, thereby facilitating metastasis.25 More recently, Sawicki et al26reported the release of MMP2 by human platelets and claimed that MMP2 was involved in platelet-aggregating response. They showed that active but not latent MMP2 enhanced platelet aggregation triggered by collagen and that the inhibition of MMP2 activation inhibited platelet aggregation. However, the mechanism of MMP2 activation was not elucidated.
In the present work, we show the expression of MT1-MMP in blood platelets and its role in platelet aggregation within the trimolecular complex MT1-MMP/TIMP2/MMP2. We also demonstrate the modulatory effect of natural (TIMP2) and synthetic (BB94) MMP inhibitors on the platelet response.
Materials and methods
Materials
Collagen Horm was provided by Nycomed (Münich, Germany). Gelatine, arachidonic acid (AA), adenosine 5′-diphosphate (ADP), fibrinogen, bovine serum albumin (fraction V), human thrombin, and mouse monoclonal immunoglobulin (Ig) G1 antibodies were from Sigma Chemical Co (St Louis, MO). Agarose and the enzymes for reverse transcription (RT) were from Gibco BRL (Gaithersburg, MD). Human high molecular weight urokinase was from Hoechst-Behring (Puteaux, France). The molecular weight standards for the sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) gels were from Bio-Rad (Hercules, CA). Human monoclonal antibodies to MMP2 [Ab-3], MMP9 [Ab-1], TIMP2 [Ab-1], and MT1-MMP [Ab-1]15 and human recombinant TIMP1 and TIMP2 were obtained from Oncogene Science (Genzyme, Cambridge, MA). The ECL kit, the goat antimouse IgG and (α-32P) dCTP were from Amersham Life Science (Buckinghamshire, United Kingdom). The MMP synthetic inhibitor BB94 (Batimastat; P. D. Brown, L. Bawden, K. Miller, Patent, WO 93/21942, 199327) was from British Biotech (Oxford, United Kingdom). All other reagents were of analytical grade.
Preparation of human platelets
Blood was obtained from healthy human volunteers who had not received any medication for at least 10 days and was anticoagulated with one-sixth of its final volume by citric acid–citrate dextrose (7 mmol/L, 93 mmol/L, and 139 mmol/L, respectively, pH 6.4) containing heparin (20 IU/mL). Washed platelets were prepared according to Mustard et al28 except that apyrase was omitted and prostacyclin (PGI2) (1 nmol/L) was added during the first 2 steps of washing. The platelets were resuspended in Tyrode's buffer and adjusted to a final concentration of 5 ×108 cells/mL.
Platelet aggregation
Aggregation was monitored at 37°C by measuring the variation of light transmission according to method of Born29 with a Chronolog aggregometer. Briefly, 400-μL samples of washed platelets supplemented with fibrinogen (0.28 mg/mL) and stirred at 1100 rpm were preincubated with MMPs inhibitors, TIMP1, TIMP2, and BB94 at different concentrations. After 2 minutes of incubation, pretreated platelets were then challenged with different agonists (AA, collagen, ADP, thrombin). The percentage of aggregation was determined 3 minutes after addition of the stimulating agent.
Flow cytometry analysis
Membrane surface expression of MMP2, MT1-MMP, TIMP2, and MMP9 by resting and activated platelets was studied by flow cytometry. Nonstirred washed platelets (5 × 108/mL) were incubated in an aggregometer cuve at 37°C for 5 minutes in the presence or in the absence of 0.5-μg/mL collagen. The platelets were then immediately fixed in 1% formaldehyde for 30 minutes, adjusted to 106 cells/mL, and distributed in a 96-well culture plate. Platelets were incubated 30 minutes in the dark at 4°C with MMP2, MT1-MMP, TIMP2, or MMP9 monoclonal antibody or with a mouse IgG (control isotype). The samples were then washed twice in Tyrode's buffer and incubated for 30 minutes at 4°C with fluorescein isothiocyanate–conjugated goat antimouse IgG (20 μg/mL). Finally, samples were washed, centrifuged, and resuspended in 0.6 mL of Tyrode's buffer. Analysis was performed using FACScan instrument (Becton Dickinson, San Jose, CA).
Membrane preparation
Plasma membranes were prepared from human mesangial cells and from human washed platelets as previously described30 and stored at −80°C.
Gelatin zymography and reverse zymography
The gelatinolytic activity in pellets and supernatant of resting and activated platelets was visualized on zymograms performed under nonreduced conditions, using SDS-polyacrylamide gels containing 1-mg/mL gelatin (7.5% PAGE for gelatin zymography and 14% for reverse zymography). After electrophoresis the gels were soaked in 2.5% Triton X-100 for 1 hour to remove SDS and incubated in Tris-HCl (50 mmol/L, pH 7.5), CaCl2 (5 mmol/L), and ZnCl2 (1 μmol/L) overnight at 37°C and stained with Coomassie blue dye. Reverse gelatin zymography was performed by incubating SDS-PAGE gels in the same buffer containing 1 volume of HT1080 serum-free conditioned medium.
Immunoblot analysis
After SDS-PAGE, in nonreduced or reduced conditions (1-mmol/L β-mercaptoethanol), the proteins were transferred onto polyvinylidene difluoride membrane (Millipore Corp, Bedford, MA) with a Trans-Blot semidry transfer cell (Bio-Rad). After blocking 1 hour at 37°C in Tris-HCl (50 mmol/L, pH 7.5), NaCl (100 mmol/L), triethanolamine-buffered saline (TBS) containing 2% bovine serum albumin, and 0.1% Tween 20, the membrane was incubated with monoclonal antibodies anti-TIMP2 (1 μg/mL) or anti–MT1-MMP (10 μg/mL) for 18 hours at 4°C. After extensive washing in TBS–0.1% Tween 20, the membrane was incubated with goat antimouse IgG for 1 hour at room temperature. After extensive washing, the blots were revealed by chemoluminescence with the ECL kit.
Amplification of platelet MT1-MMP, MMP2, and TIMP2
Total RNA from human platelets was isolated by the method of Chomczynski and Sacchi.31 The mRNA was reverse transcribed using random hexamers. A total of 25 ng of complementary DNA was used as a template in each polymerase chain reaction (PCR). The sense primer 5′-CCCTATGCCTACATCCGTGA-3′ and the antisense primer 5′-TCCATCCATCACTTGGTTAT-3′, complementary to nucleotides 598 to 617 and 1148 to 1167, respectively, of human MT1-MMP were used as described.15,18 For MMP2, the sense primer 5′-TTTTCTCGAATCCATGATGG-3′ and the antisense primer 5′-CTGGTGCAGCTCTCATATTT-3′, complementary to nucleotides 428 to 447 and 1028 to 1047, respectively, were used according to Martin et al.32 For TIMP2, the sense primer 5′-GTTTTGCAATGCAGATGTAG-3′ and the antisense primer 5′-ATGTGGAGAAACTCCTGCTT-3′, complementary to nucleotides 381 to 400 and 901 to 920, respectively, were used as described.32 PCR was performed by standard techniques using Taq polymerase, repeating 35 cycles of a 60-second denaturation step at 94°C, a 60-second annealing step at 60°C, and a 60-second extension step at 72°C for MT1-MMP; denaturation was 60 seconds at 95°C and annealing 90 seconds at 52°C for MMP2 and TIMP2. The respective amplified PCR products were analyzed on a 1.5% agarose gel and scanned.
Results
Expression and release of MMP2, MT1-MMP, and TIMP2 by aggregated platelets
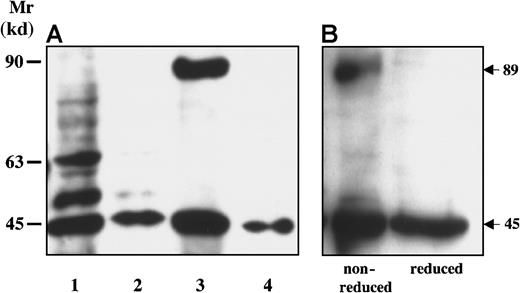
Control and collagen- (1 μg/mL) aggregated platelets were centrifuged, and the supernatants and the pellets were collected and analyzed by gelatin zymography under nonreduced conditions. In the supernatants of resting platelets, gelatin zymograms showed the presence of a unique gelatinolytic band of 68 kd corresponding to latent MMP2 (Figure 1, lane1). After stimulation, 2 activated forms of 62 and 59 kd appeared in the supernatants (Figure 1, lane 2). No gelatinolytic activity associated with the platelet pellet could be detected (Figure 1, lane 3).
Expression of MMP2 by human platelets.
Human washed platelets were resuspended in Tyrode's buffer and were divided into 2 groups corresponding to resting and collagen- (1 μg/mL) aggregated platelets. Supernatants from resting and activated platelets as well as the platelet pellet solubilized in the sample buffer (lane 3) were studied by gelatin zymography in a 7.5% acrylamide gel containing 1-mg/mL gelatin under nonreduced conditions. Gelatinolytic activity at 68 kd and at 62 to 59 kd was visualized, indicating the presence of MMP2 in proform in resting platelets (lane 1) and in proform and activated forms in activated platelets (lane 2).
Expression of MMP2 by human platelets.
Human washed platelets were resuspended in Tyrode's buffer and were divided into 2 groups corresponding to resting and collagen- (1 μg/mL) aggregated platelets. Supernatants from resting and activated platelets as well as the platelet pellet solubilized in the sample buffer (lane 3) were studied by gelatin zymography in a 7.5% acrylamide gel containing 1-mg/mL gelatin under nonreduced conditions. Gelatinolytic activity at 68 kd and at 62 to 59 kd was visualized, indicating the presence of MMP2 in proform in resting platelets (lane 1) and in proform and activated forms in activated platelets (lane 2).
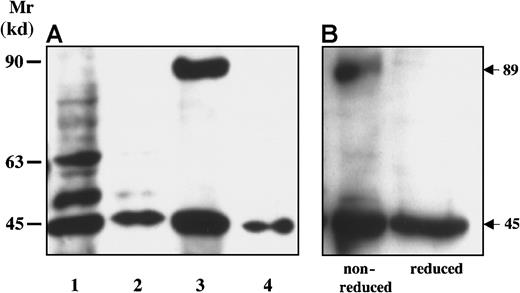
Western blot analysis of cell membranes showed that resting platelets (Figure 2A, lane 3) expressed MT1-MMP in 2 forms: the inactive 45-kd MT1-MMP similar to that in membranes of urokinase-treated mesangial cells (Figure 2A, lane 2) and another unusual 89-kd form. After platelet aggregation, only the 45-kd band remained associated with the platelet membranes (Figure 2A, lane 4). To study whether the 89-kd band was a new molecular form of MT1-MMP or a complex containing MT1-MMP, we performed SDS-PAGE under reduced conditions (1-mmol/L β-mercaptoethanol), and the proteins were analyzed by Western blot. The results showed that in reduced conditions the 89-kd band disappeared, whereas the 45-kd band remained unchanged with anti–MT1-MMP (Figure 2B).
Expression of MT1-MMP on platelet membranes.
(A) Human mesangial cell membranes (HMCs, lane 1), HMC membranes treated by urokinase (100 nmol/L for 24 hours) (lane 2), human resting platelet membranes (lane 3), and aggregated platelet membranes (lane 4) were analyzed by immunoblotting using an antihuman MT1-MMP monoclonal antibody. (B) Human platelet membranes were analyzed by immunoblot in nonreduced and reduced conditions.
Expression of MT1-MMP on platelet membranes.
(A) Human mesangial cell membranes (HMCs, lane 1), HMC membranes treated by urokinase (100 nmol/L for 24 hours) (lane 2), human resting platelet membranes (lane 3), and aggregated platelet membranes (lane 4) were analyzed by immunoblotting using an antihuman MT1-MMP monoclonal antibody. (B) Human platelet membranes were analyzed by immunoblot in nonreduced and reduced conditions.
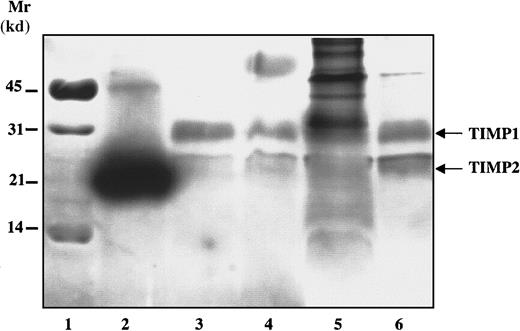
By reverse zymography, both TIMP1 and TIMP2 were detected in platelet supernatants of resting (Figure 3, lane 3) and activated (Figure 3, lane 4) platelets as well as in purified platelet membranes (Figure 3, lane 6).
Expression of TIMP1 and TIMP2 in human platelets.
Resting and collagen- (1 μg/mL) activated platelets were centrifuged and analyzed for TIMP expression by reverse zymography. Lane 1: molecular weight markers; lane 2: human recombinant TIMP2; lane 3: supernatants from resting platelets; lane 4: supernatants from activated platelets; lane 5: activated platelet pellet; lane 6: purified platelet membranes.
Expression of TIMP1 and TIMP2 in human platelets.
Resting and collagen- (1 μg/mL) activated platelets were centrifuged and analyzed for TIMP expression by reverse zymography. Lane 1: molecular weight markers; lane 2: human recombinant TIMP2; lane 3: supernatants from resting platelets; lane 4: supernatants from activated platelets; lane 5: activated platelet pellet; lane 6: purified platelet membranes.
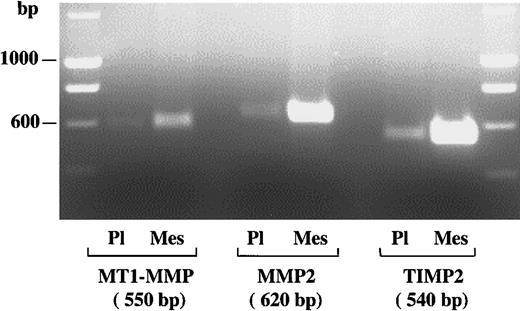
Expression of mRNAs encoding for MMP2, MT1-MMP, and TIMP2 in platelets
RT-PCR was performed on total RNA extracted from washed human platelets. The resulting products were compared with those obtained from human mesangial cells as control. We found mRNAs encoding for MT1-MMP, MMP2, and TIMP2 as single bands of 550, 620, and 540 base pairs, respectively, as predicted by the selected primers. RT-PCR products from platelets were of the same size as in control mesangial cells, but mRNA transcript levels were in lower amounts in platelets than in mesangial cells (Figure 4).
Expression of MT1-MMP, MMP2, and TIMP2 mRNA transcripts in platelets.
Using RT-PCR analysis, the expression of MT1-MMP, MMP2, and TIMP2 mRNA transcripts was studied in washed platelets and compared with corresponding mRNA transcripts expressed by human mesangial cells. PCR products stained with ethidium bromide were electrophoresed in a 1.5% agarose gel. The figure shows RT-PCR products of total RNA derived from platelets (Pl) and mesangial cells (Mes) using specific primers for MT1-MMP, MMP2, and TIMP2. Left and right panels represent the molecular size markers, and the bands of 550, 620, and 540 base pairs correspond to MT1-MMP, MMP2, and TIMP2, respectively.
Expression of MT1-MMP, MMP2, and TIMP2 mRNA transcripts in platelets.
Using RT-PCR analysis, the expression of MT1-MMP, MMP2, and TIMP2 mRNA transcripts was studied in washed platelets and compared with corresponding mRNA transcripts expressed by human mesangial cells. PCR products stained with ethidium bromide were electrophoresed in a 1.5% agarose gel. The figure shows RT-PCR products of total RNA derived from platelets (Pl) and mesangial cells (Mes) using specific primers for MT1-MMP, MMP2, and TIMP2. Left and right panels represent the molecular size markers, and the bands of 550, 620, and 540 base pairs correspond to MT1-MMP, MMP2, and TIMP2, respectively.
Enhanced expression of trimolecular complex components during platelet activation
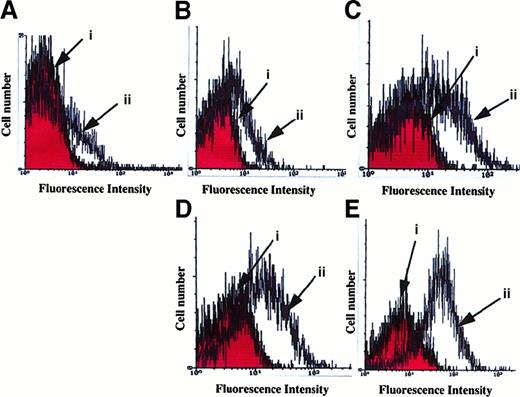
To study platelet surface expression of MT1-MMP, MMP2, and TIMP2, resting and activated platelets were used. Flow cytometry analysis showed the expression at the cell surface of MMPs and of TIMP2 before activation. As shown by an increase of fluorescence intensity when platelets were incubated with specific monoclonal antibody to MMP2 and MT1-MMP, compared with appropriate isotype, platelet activation enhanced the expression of MMP2 and MT1-MMP (Figure5C-D). In addition, a large amount of TIMP2 was released and remained associated with platelet membranes during platelet activation (Figure 5E). A very small amount of MMP9 was detected on resting platelets and did not increase after platelet activation (Figure 5B).
Flow cytometry analysis of MMPs on the platelet membrane surface.
Resting and collagen- (0.5 μg/mL) activated platelets were treated as described in “Materials and methods.” (A) Nonspecific fluorescence intensity where resting (i) and activated (ii) platelets were pretreated with mouse IgG (control isotype). (B-E) Fluorescence intensities when resting (i) and activated (ii) platelets were pretreated with specific MMP9 (B), MMP2 (C), MT1-MMP (D), and TIMP2 (E) monoclonal antibodies, respectively. Results are representative of 3 separate experiments.
Flow cytometry analysis of MMPs on the platelet membrane surface.
Resting and collagen- (0.5 μg/mL) activated platelets were treated as described in “Materials and methods.” (A) Nonspecific fluorescence intensity where resting (i) and activated (ii) platelets were pretreated with mouse IgG (control isotype). (B-E) Fluorescence intensities when resting (i) and activated (ii) platelets were pretreated with specific MMP9 (B), MMP2 (C), MT1-MMP (D), and TIMP2 (E) monoclonal antibodies, respectively. Results are representative of 3 separate experiments.
Inhibition of platelet aggregation and of MMP2 activation by MMP inhibitors
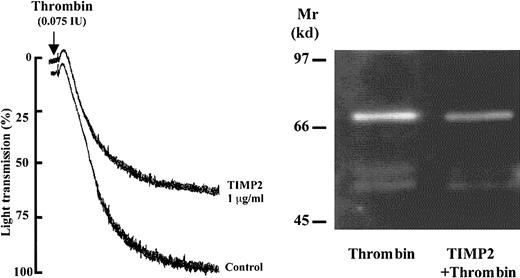
The role of MMP inhibitors in platelet aggregation was studied using various agonists. Washed platelets (108 cells/mL) were preincubated with MMP-specific tissue inhibitors TIMP1 (1.5 μg/mL), TIMP2 (0.5-1.5 μg/mL) or a synthetic compound BB94 (2.5-4.0 μmol/L). After 2 minutes, platelets were exposed to collagen (1 μg/mL), AA (10 μmol/L), ADP (10 μmol/L), or thrombin (0.075 IU/mL). Both TIMP2 and BB94 inhibited collagen-induced platelet aggregation in a concentration-dependent manner (Figure6A, upper panel). The inhibition of platelet aggregation was associated with the absence of activation of MMP2 as shown by zymography analysis of the same supernatants (Figure6B). In contrast, TIMP1 had no significant inhibitory effect (Figure6A, upper panel). Similar inhibition of platelet aggregation was observed with TIMP2 and BB94 when platelets were triggered by AA or by ADP (Figure 6A, lower panel). When platelets were stimulated by thrombin, only a partial inhibition of platelet response and MMP2 activation was observed in the presence of TIMP2 (Figure7).
Inhibition of platelet aggregation by TIMP2 and BB94.
(A) Platelets were pretreated for 2 minutes with MMP inhibitors as indicated and then triggered by collagen (1 μg/mL), AA (10 μmol/L), or ADP (10 μmol/L). The figure shows the inhibition by TIMP2 (0.5-1.5 μg/mL) and BB94 (2.5-4 μmol/L) but not by TIMP1 (1.5 μg/mL) of platelet response. Results are representative of 3 separate experiments. (B) The supernatants of platelets treated as indicated on the figure were analyzed by gelatin zymography.
Inhibition of platelet aggregation by TIMP2 and BB94.
(A) Platelets were pretreated for 2 minutes with MMP inhibitors as indicated and then triggered by collagen (1 μg/mL), AA (10 μmol/L), or ADP (10 μmol/L). The figure shows the inhibition by TIMP2 (0.5-1.5 μg/mL) and BB94 (2.5-4 μmol/L) but not by TIMP1 (1.5 μg/mL) of platelet response. Results are representative of 3 separate experiments. (B) The supernatants of platelets treated as indicated on the figure were analyzed by gelatin zymography.
Effect of TIMP2 on thrombin-induced platelet aggregation and MMP2 activation.
(Left panel) The platelets were pretreated for 2 minutes with TIMP2 (1 μg/mL) and exposed to thrombin (0.075 IU/mL). (Right panel) The supernatants of platelets treated as indicated were studied by gelatin zymography.
Effect of TIMP2 on thrombin-induced platelet aggregation and MMP2 activation.
(Left panel) The platelets were pretreated for 2 minutes with TIMP2 (1 μg/mL) and exposed to thrombin (0.075 IU/mL). (Right panel) The supernatants of platelets treated as indicated were studied by gelatin zymography.
Discussion
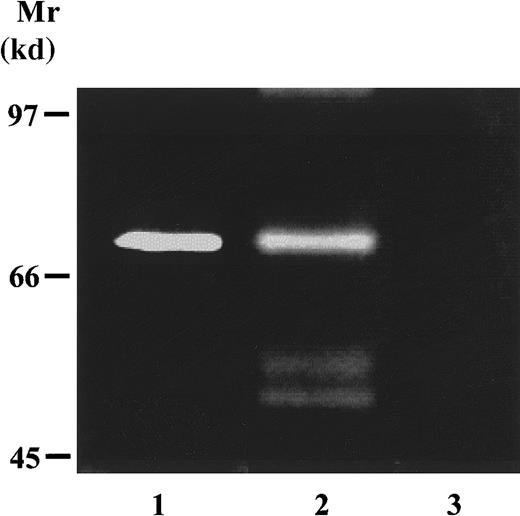
Recently, Sawicki et al26 have reported the release of pro-MMP2 by platelets and have demonstrated a proaggregatory effect of active human recombinant MMP2, but the mechanism of pro-MMP2 activation was not elucidated and, in particular, the expression of MT1-MMP by platelets has never been addressed. MT1-MMP has been described in at least 3 membrane-associated forms: a native 63-kd, a 45-kD inactive-processed, and the 60-kd furin-processed form.33,34 We have previously shown the existence of a soluble MT1-MMP of 55 kd in human mesangial cell supernatants,30 and recently we found it in human plasma and serum (I.K. et al, unpublished data, 1998). This finding lead us to study MT1-MMP secretion by human platelets. The results of Western blot experiments on human resting platelet membranes showed 2 major immunoreactive bands of 45 and 89 kd. The 89-kd band, recognized by the MT1-MMP monoclonal antibody, was never described before. To study whether this 89-kd protein could represent a new molecular form of MT1-MMP or a complex containing MT1-MMP, the platelet membranes were also analyzed in reduced conditions. In the presence of β-mercaptoethanol, the 89-kd band totally disappeared, pointing to the existence of a complex. Considering the apparent molecular weight (89 kd), this protein could be either a 45-kd MT1-MMP dimer or native MT1-MMP (63 kd) complexed to TIMP2 (21 kd). Interestingly, it was recently shown that TIMP2 could bind MT1-MMP at the cell surface, generating the MT1-MMP/TIMP2 receptor necessary for pro-MMP2 activation.20 35-37 It was tempting to hypothesize that the 89-kd protein could represent a readily assembled receptor on platelet membranes, especially because the reverse zymogram and the flow cytometry data showed the existence of TIMP2, a soluble protein, on membranes of resting platelets. However, Western blot with our anti-TIMP2 antibodies failed to detect the 89-kd band (data not shown), and this is currently studied.
The apparent discrepancy between the increase of MT1-MMP expression observed by flow cytometry during platelet activation and the decrease of total MT1-MMP protein on membranes after collagen-induced aggregation, visualized by Western blot, may be explained by differences in the experimental conditions. In the flow cytometry experiments, platelets were activated without stirring and were not aggregated; MT1-MMP was expressed at the cell surface but not consumed. Then platelets were fixed and stained with anti–MT1-MMP antibody. In contrast, in Western blot experiments, platelets were recovered by centrifugation at the end of the aggregation and lysed in the sample buffer. During platelet aggregation, MT1-MMP had been totally activated and processed into the 45-kd inactive form.
Pro-MMP2 activation on the cell surface is a complex process involving a trimolecular complex composed of TIMP2 interacting simultaneously with the catalytic site of MT1-MMP and with the C-terminal domain of pro-MMP2.21,36 Then, a second “free” MT1-MMP molecule cleaves and activates pro-MMP2, generating an intermediate 64-kd form.37-39 The autocatalytic cleavage of MMP2 generates the active 62- and 59-kd forms. MT1-MMP activation sequentially generates the 60-kd active and a 45-kd inactive species, the latter being a product of MMP2 activation.40 41 Indeed, we observed in membranes of activated platelets the total disappearance of the 89-kd MT1-MMP concomitantly to the generation of the 62- to 59-kd active forms of MMP2 in platelet supernatant. Therefore, our results indicate that MT1-MMP is not only a major determinant of pro-MMP2 activation on platelets but also that this activation has taken place within the trimolecular complex MT1-MMP/TIMP2/MMP2. This finding is further supported by the presence of TIMP2 in platelets.
The platelet collagenolytic activity has been studied in guinea pigs42 and in human beings,26 and the presence of TIMP1 and TIMP2 in human megakaryocytes and platelets has been established recently.43 The fact that TIMP1 was also expressed by platelets could explain the existence of latent MMP2 in both resting and activated platelets. MMP2 activity is sensitive to inhibition by both TIMP1 and TIMP2,21 but recent studies have reported contrary effects of TIMP1 and TIMP2 on MMP2 and MT1-MMP activity. TIMP1 appears to be an effective inhibitor of MMP244 but is not able to form a complex with pro-MMP2.45 TIMP2 has dual effects on MMP2. At stochiometric concentrations, TIMP2 allows pro-MMP2 activation in the trimolecular complex and, in excess, TIMP2 binds free MT1-MMP, therefore preventing pro-MMP2 cleavage and activation by free MT1-MMP. MT1-MMP is also sensitive to the inhibition by TIMPs; however, unlike TIMP2, TIMP1 even at high concentration is unable to inhibit the processing of MT1-MMP.40 The fact that platelet aggregation could be inhibited by BB94 indicates that this inhibition is rather due to the inhibition of MMP2 and of MT1-MMP than to a direct effect of TIMP2 on platelets. In addition, the inhibition of platelet aggregation by TIMP2, but not by TIMP1, indicates an inhibitory profile characteristic of MT1-MMP.35,36 The partial inhibition of thrombin-induced platelet aggregation could be explained by the direct proteolysis and activation of MMP2 by thrombin,46bypassing the inhibitory effect of TIMP2 on the activation of MMP2 within the trimolecular complex.
In conclusion, our results have demonstrated the presence of MT1-MMP in human platelets, the release of the components of the trimolecular complex MT1-MMP/TIMP2/MMP2 during platelet activation, and MT1-MMP's role in the modulation of platelet aggregation.
Acknowledgment
We thank Dr Agnes Noel for helpful suggestions.
Supported by a grant from the French Academy of Medicine.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Isabelle Kazes, INSERM U489, Hôpital Tenon, 4 rue de la Chine, 75020, Paris, France; e-mail:kazes@b3e.jussieu.fr.