Abstract
In the attempt to develop immunotherapeutic strategies for acquired immunodeficiency syndrome capable of activating effector cells in an antigen-specific manner while maintaining the broadest possible T-cell repertoire, we evaluated two canarypox (ALVAC)-based vectors for their capacity to induce ex vivo activation/expansion of human immunodeficiency virus (HIV)-specific CD8+ cytotoxic lymphocyte precursors (CTLp) obtained from HIV-1–infected donors. These two vectors, vCP205 encoding HIV-1 gp120 + TM (28 amino acid transmembrane anchor sequence) in addition to Gag/protease and vCP300 encoding gp120 + Gag/protease as well as Nef and Pol CTL determinants, are pancytotropic but replication incompetent in mammalian cells. Bulk peripheral blood mononuclear cells (PBMCs) or enriched CD8+ T cells were stimulated for 10 days with autologous ALVAC-infected PBMCs in the presence of different cytokine combinations (interleukin-2 [IL-2], IL-4, IL-7, and IL-12). Activation by ALVAC constructs was highly antigen-specific, because vCP205 elicited only Env and Gag CTL, whereas vCP300 elicited broader reactivities against Env, Gag, Pol, and Nef determinants. The ALVAC activation of CTLp was IL-2 dependent and enhanced by the addition of IL-7, whereas IL-4 and IL-12 failed to augment cytotoxic reactivities elicited by these constructs. The expansion of enriched CD8+ T cells after activation with vCP300 was higher in patients with CD4 counts greater than 400 cells/μL. Two rounds of in vitro stimulation (IVS) with vCP300 resulted in nearly an eightfold expansion of CD8+ lymphocytes over a 25-day period. After the second IVS, an average 3.2-fold increase among the different antigen-specific CTL frequencies was achieved. These studies clearly show that HIV-recombinant ALVAC vectors represent powerful polyvalent antigenic stimuli for activation and expansion of the CD8 lymphocyte response that occurs as a result of HIV infection.
THE NATURAL HISTORY of human immunodeficiency virus-1 (HIV-1) infection is complicated by a multitude of host and viral factors, but in most infected patients leads to the development of the acquired immunodeficiency syndrome (AIDS) within 10 years of seroconversion.1-3 During this time, a balance is established between active virus replication4,5 and immune reactivities capable of preventing rapid impairment of overall immunologic integrity. In humans, CD8+ cytotoxic T lymphocytes (CTL) seem to play a central role in the host defense against viral infections.6,7 Several recent observations suggest that a similar role may be played in the context of HIV infection. Peak viremia during the acute phase of disease is resolved concomitantly with the detection of CTL reactivities.8,9 A steady decrease of CTL activity has also been well documented during progression of HIV disease,10,11 as well as the persistence of HIV-1 CTL responses in long-term asymptomatic subjects.12 Finally, HIV-exposed but uninfected women, as well as uninfected babies born to infected mothers, displayed HIV-specific CTL responses.13-15 This body of evidence strongly suggests that cytotoxic lymphocytes may represent an important element not only in controlling the progression of disease, but also as a component of protective immunity against HIV infection. Therefore, immunotherapeutic strategies involving either ex vivo expansion and reinfusion of antigen-specific effectors or in vivo activation of cytotoxic T lymphocytes via active immunization may be capable of altering the natural history of disease by impacting on the proviral load of the infected host.
In previous studies conducted in our laboratory, we developed an antigen-specific, recombinant vaccinia-based in vitro stimulation (Ag-IVS) procedure that facilitated the activation and expansion of HIV-specific CTL.16,17 If this strategy is to be applied in a clinical setting, the vaccinia vectors used for antigen-specific stimulation may present a major safety concern, because a pathogenic and fully replication-competent vector can have lethal consequences in an immunocompromised host.18 The naturally attenuated canarypox (ALVAC) constructs have been shown to be an efficient tool in the induction of protective immunity against rabies and feline leukemia viruses.19,20 More recently, these constructs have been shown to protect rhesus macaques from HIV infection21 and to induce anti–HIV-1 Env-specific CTL in seronegative volunteers.22,23 Canarypox viral vectors retain the pancytotropism of most poxviruses, but are unable to productively replicate in nonavian species,24 25 thus eliminating the safety concerns that exist for vaccinia vectors. In this study, we evaluate the capacity of ALVAC constructs to bring about the activation and expansion of antigen-specific CTL populations present in the peripheral blood of HIV-infected individuals.
MATERIALS AND METHODS
Patients.Ten HIV-1–infected volunteers selected for this study were enrolled by Dr J. A. Bartlett at the Adult Infectious Diseases Clinic, Duke University Medical Center (Durham, NC). At the time of study, 8 patients were clinically asymptomatic with absolute CD4 cell counts greater than 400 cells/μL (patients no. 1, 2, 3, 4, 5, 8, 9, and 10). Patients no. 6 and 7 had absolute CD4 cell counts lower than 400 cells/μL but remained asymptomatic. All of the subjects enrolled in this study had a history of smallpox immunization. Venous blood samples were obtained from these volunteers after informed consent was given.
Cytokines.Recombinant human interleukin-7 (IL-7) was purchased from Genzyme Corp (Cambridge, MA) and reconstituted according to the manufacturer's instructions. For all assays, IL-7 was used at a concentration of 330 U/mL and added at the initiation of IVS. Recombinant human IL-2 was provided by Hoffman-La Roche (Nutley, NJ). Recombinant human IL-4 and IL-12 were purchased from Genzyme Corp (Cambridge, MA) and R&D Systems (Minneapolis, MN), respectively.
Generation of ALVAC-based recombinant viruses.The generation of the ALVAC (canarypoxvirus25 )-HIV env (vCP112) construct has been described previously.26 ALVAC-MN120TMG (vCP205) was generated in a similar fashion using the donor plasmid, pHIV32, that enabled the coinsertion of the poxvirus/HIV expression cassette into the C3 locus of the ALVAC genome using standard procedures.27 One inserted expression cassette contained the region of the HIV-1MN env gene corresponding the extracellular envelope gp120 moiety28 linked to the sequence encoding the HIV-1 Env transmembrane anchor sequence (28 amino acids29 ). This cassette was engineered to be under the control of the vaccinia virus H6 promoter.30 The Gag cassette contained the entire HIV-IIIB gag coding sequence and a portion of the pol region sufficient to encode the protease function. This cassette was juxtaposed 3′ to the vaccinia virus I3L promoter region. Insertion of these individual cassettes occurred in a head to head (5′ to 5′) configuration in the ALVAC genome to generate ALVAC-MN120TMG (vCP205).
ALVAC-MN120TMGNP (vCP300) was derived from ALVAC-MN120TMG (vCP205) by the insertion of cassettes that encode polypeptides that contain the known Nef- and Pol-specific human CTL epitopes.31 The two cassettes encoding the Nef-specific polypeptides (amino acids 66-147; 182-198, according to Ratner et al29 ) were coinserted by standard protocols27 into the ALVAC C5 locus, whereas the three Pol polypeptides (amino acids 179-219; 325-383; 461-519, according to Ratner et al29 ) were coinserted in the C6 locus.
Genomic DNA from recombinant viruses was analyzed by restriction analysis to ensure the precise incorporation of foreign genetic material with no other gross genomic alterations. Furthermore, nucleotide sequence analysis was performed on polymerase chain reaction (PCR)-derived DNA fragments amplified from recombinant genomic DNA (results not shown). Results from these analyses confirmed the sequence of the inserted expression cassettes and flanking ALVAC genomic sequences. Expression of the HIV-1 Env and Gag components was confirmed by immunoprecipitation using [35S]-methionine–labeled lysates derived from recombinant virus infected cells and appropriate antiserum preparations, as per standard protocols.32
Recombinant vaccinia viruses.Autologous Epstein-Barr virus-transformed B-lymphocyte cell line (BLCL) targets for CTL assays were infected with recombinant vaccinia viruses expressing the following extrinsic gene inserts: vSC8 (E coli lac operon), vP1174 (HIV-1MN gp160), VDK1 (HIV-1IIIB gag), vCF21 [HIV-1IIIB all but the last 22 residues of HXB.2 subclone reverse transcriptase (pol)], vP1206 (HIV-1IIIB gag/pol), and vP1218 (HIV-1MN nef ). The lac and pol vectors were kindly provided by B. Moss (National Cancer Institute, National Institutes of Health, Bethesda, MD) and the gag construct was a generous gift from D. Kuritzkes (University of Colorado Health Sciences Center, Denver, CO). The env, gag/pol, and nef constructs were supplied by J. Tartaglia (Virogenetics, Troy, NY).
In vitro stimulation of bulk peripheral blood mononuclear cells (PBMCs) with recombinant virus.PBMCs were obtained by standard Ficoll density gradient separation. Twenty-five million PBMCs were resuspended at 1 × 106 cells/mL in AIM-V medium (GIBCO Laboratories), supplemented with 5% human AB serum (Advanced Biotechnologies Inc, Columbia, MD; culture medium), and 330 U/mL of IL-7. Five million cells were used as stimulator cells (SC). The SC were infected with ALVAC constructs for 75 minutes at 37°C in 15 mL polypropylene tubes (Sarsted Inc, Newton, NC) at a multiplicity of infection (MOI) of 10:1, washed once, and cocultured with the remaining PBMC in T-75 flasks (Costar, Cambridge, MA) at a responder:stimulator ratio of 5:1. At day 3, 50 U/mL of IL-2 was added to the Ag-IVS cultures, which were reincubated at 37°C in 5% CO2 until day 10, when they were tested for the presence of anti-HIV cytotoxic lymphocytes.
Purification and expansion of autologous CD8+ T cells.Purified CD8+ T lymphocytes were captured onto CD8 T25 MicroCELLector flasks (RPR Gencell, Santa Clara, CA), as previously described by Whiteside et al.33 The nonadherent cells were subsequently placed in T25 CD5/8 MicroCELLector flasks to reduce the number of contaminating CD4 T lymphocytes among the cells to be used as stimulators. After 1 hour of incubation, the nonadherent cells from the CD5/8 devices were collected by gentle washing and infected with ALVAC constructs (MOI = 10) for 1 hour at 37°C. After washing, the stimulator cells were added to CD8+ purified cells at an R:S = 5:1, and fresh culture medium supplemented with IL-7 was added to achieve a concentration of 1 × 106 cells/mL. In selected experiments CD8 cells were also stimulated with either 0.1 μg/mL phytohemagglutinin (Sigma, St Louis, MO) or 50 ng/mL of anti-CD3 monoclonal antibody (MoAb; Orthoclone OKT3; Ortho Biotech, Raritan, NJ) and 50 U/mL IL-2. After 3 days, an additional 50 U/mL of IL-2 was added to the Ag-IVS cultures. Cell counts were performed on all cultures every 3 to 4 days and the cell concentration was adjusted to 1 × 106 cells/mL with culture medium supplemented with 50 U/mL of IL-2. The combination of IL-7 and IL-2 was always used in the subsequent experiments of CD8 expansion with antigen stimulation.
To determine the influence of IL-4 and IL-12 on the expansion of CD8 lymphocytes, the two cytokines were added at different times during the in vitro stimulation according to previous reports.34 35 CTL frequencies were calculated by limiting dilution analysis at day 10.
To evaluate the effect of a second round of stimulation, Ag-IVS CD8 cells from patient no. 2 were restimulated on day 18 with ALVAC-infected PBMC prepared as described above and used at an R:S = 5:1. In this experiment, the CTLp frequencies were determined on days 14 and 25.
Magnetic beads.Anti-CD4 and anti-CD8 MoAb-coated beads (Dynal, Oslo, Norway) were used according to manufacturer's instructions and at a 10:1 bead-to-cell ratio to selectively deplete effector cells for the CTL assay. Goat antimouse IgG-coated beads were used as controls for the manipulations. Lymphocyte depletion efficiency was analyzed by flow cytometry and was generally found to be greater than 90%.
CTL assay.Autologous BLCLs were used as targets in the CTL assay after infection with recombinant vaccinia-HIV constructs. Briefly, aliquots of 2 × 106 BLCLs were infected (MOI = 5:1) for 90 minutes at 37°C with the vSC8, vP1174, vDK1 or vP1206, vCF21, and vP1218 constructs. Cells were subsequently washed and incubated in 1 mL of medium containing 100 to 200 μCi of sodium chromate (51Cr; E.I. Du Pont Inc, Wilmington, DE) for 16 hours at 37°C and 5% CO2 . At the end of this incubation, the cells were washed, counted, resuspended in RPMI-1640 supplemented with 10% fetal calf serum (assay medium), and plated at a concentration of 5 × 103 viable target cells/well in a round-bottomed 96-well plate. Fresh PBMCs and in vitro-stimulated lymphocytes (IVSL) were treated with antibody-coated magnetic beads as described above. Unfractionated (ie, anti-MoIgG–treated) IVSL were resuspended in assay medium and used as effectors at E:T ratios ranging from 40:1 to 5:1. Subset-depleted populations (anti-CD4– and anti-CD8–treated cells) were resuspended to the same volume as unfractionated samples. Each E:T ratio was tested in triplicate. Target cells plus either medium or 0.5% Triton X-100 served as controls for spontaneous release (SR) and maximum 51Cr release (MR), respectively. After 4 hours of incubation at 37°C in 5% CO2 , cell-free supernatants were harvested and counted on a gamma counter. The percent specific lysis (%SL) was calculated according to the formula: ([cpm experimental release] − [cpm SR])/([cpm MR] − [cpm SR]) × 100. Spontaneous release did not exceed 20% of MR. The %SL against the HIV constructs was considered significant when it was greater than 10% above the SL against the control (vSC8) targets.
The results expressed in lytic units (LU) were calculated according to the method described by Pross et al.36 One LU is defined as the number of effectors required for 20% lysis of 5 × 103 target cells, and the number of LU present in 106 effector cells was calculated. The HIV-1–specific activity detectable above the baseline activity against the vaccinia-infected targets was considered as positive.
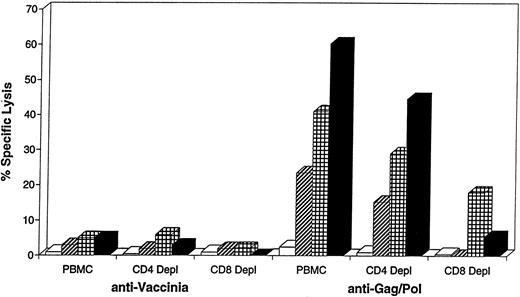
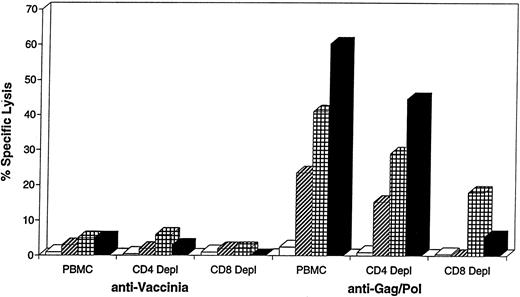
Effect of IL-7 and IL-2 on the activation/expansion of anti-HIV CTL after Ag-IVS with vCP300. The CTL assay was performed at day 10 after IVS and data are reported as the percentage of specific lysis against vaccinia control (vP1170) and Gag/Pol-expressing (vP1206) autologous BLCL. The effector:target ratio was 10:1. Effector cells were depleted for CD4 or CD8 cells using magnetic beads as described in the Materials and Methods. (□) vCP300; (▨) vCP300 + IL-7; (▦) vCP300 + IL-2; (▪) vCP300 + IL-7 + IL-2.
Effect of IL-7 and IL-2 on the activation/expansion of anti-HIV CTL after Ag-IVS with vCP300. The CTL assay was performed at day 10 after IVS and data are reported as the percentage of specific lysis against vaccinia control (vP1170) and Gag/Pol-expressing (vP1206) autologous BLCL. The effector:target ratio was 10:1. Effector cells were depleted for CD4 or CD8 cells using magnetic beads as described in the Materials and Methods. (□) vCP300; (▨) vCP300 + IL-7; (▦) vCP300 + IL-2; (▪) vCP300 + IL-7 + IL-2.
Anti-HIV–specific CTL frequency.The frequencies of anti-HIV–specific CTL after IVS were determined by limiting dilution analysis.37,38 Between 781 and 5 × 104 IVSL were tested in 4-hour 51Cr release assays against 51Cr-labeled BLCLs infected with various recombinant vaccinia constructs. Each effector cell dilution was plated into 24 replicate wells. A well was considered positive if 51Cr release exceeded by 3 standard deviations the mean of 24 control wells containing target cells and media. The effector cell frequency was estimated by single hit model Poisson distribution analysis,39 using the maximum likelihood method; a 95% confidence limit was determined for each estimate. The calculations were performed by using a software package kindly provided by Dr S. Kalams (Massachusetts General Hospital, Boston, MA).
Cytofluorimetric analysis.Two million cells were washed once with 1% fetal calf serum (FCS)-phosphate-buffered saline solution (PBS) and resuspended at a concentration of 1 × 106 cells/mL. One-hundred–microliter aliquots of cells were then added to appropriately labeled tubes containing the manufacturer's recommended amounts of MoAb combinations, as previously reported.17 After 15 minutes of incubation at room temperature and in the dark, cells were washed once with 1% FCS-PBS and resuspended in 250 μL of a 1% formaldehyde-PBS solution. Within 24 hours of collection, 100-μL aliquots of whole blood were added to tubes containing the manufacturer's recommended amounts of MoAb combinations, as previously reported.17 Samples were briefly vortexed and incubated for 15 minutes at room temperature in the dark. Red blood cells were then lysed using Coulter's Multi-Q-Prep automated lysing system (Coulter Corp, Hialeah, FL). After lysing, samples were washed once with PBS and resuspended in 250 μL of a 1% formaldehyde-PBS solution. Samples were analyzed on an EPICS XL flow cytometer (Coulter Corp). Lymphocyte purity of the gate was assessed using the CD14−CD45+ bright percentage and statistical analysis regions were set to include no greater than 5% background fluorescence.
RESULTS
Influence of cytokines on ALVAC-based IVS.Our previous work with recombinant vaccinia vector-based IVS showed that the addition of IL-7 at day 0 was essential for optimal activation/expansion of CTLp,17 whereas the addition of IL-2 during the first 10 days of culture had no significant impact on the expansion of CD8+ effector cells due in large part to the endogenous production of this cytokine.40 To define the optimal cytokine parameters in the context of canarypox (ALVAC)-based IVS, a series of experiments was performed in which the relative contributions of IL-7 and IL-2 were evaluated. Representative data from a total of four experiments are depicted in Fig 1. As shown, vector stimulation in the absence of exogenous cytokine failed to activate CTLp against either vaccinia (vSC8) or HIV-1-Gag/Pol (vP1206) in PBMCs obtained from patient no. 3. However, the inclusion of IL-7 at the inception of the IVS cultures as well as the addition of IL-2 on day 3 of culture resulted in amplification of anti-HIV CTL reactivities, and the two cytokines showed a partial additive effect when used in combination. Although vCP300-IVS with IL-2 was able to induce a detectable level of CTL activity, the cell recovery was lower than that obtained with IL-7 alone or with IL-7 in combination with IL-2 (data not shown). In all instances, lysis was mediated principally by a population of CD8+ CTL population, as evidenced by a 90% reduction in specific lysis after the removal of CD8+ cells. A slight reduction in specific lysis was also observed in the CD4-depleted sample. This could be due either to the activation of a minor population of CD4+ CTL against HIV-1 or to incomplete depletion of CD8+ cells.
Because recombinant IL-4 and IL-12 have been previously described as modulators of CTL responses in humans, we next investigated the effect of their addition to the Ag-IVS cultures. On the basis of two previous studies,34 35 IL-4 was added on day 5 at a concentration of 100 U/mL, whereas IL-12 was added on day 0 at a concentration of 160 pg/mL. As shown in Table 1, neither cytokine was able to improve the overall cell recovery after IVS. The elicited CTL reactivity is expressed in terms of LU20 /106 cells. Once again, the addition of IL-4 did not enhance specific CTL reactivity beyond that attained by the combination of IL-7 and IL-2 in any of the 4 patients. Moreover, in patients no. 8, 9, and 10, at least a twofold reduction in anti-Gag and anti-Pol CTL activities was observed. IL-4 also had a variable negative impact on the recovery of anti-Env and anti-Nef CTL in all of the 4 patients. The addition of IL-12 to the Ag-IVS cultures decreased the level of detectable anti-HIV CTL in patients no. 4, 8, and 9. A modest enhancing effect due to the IL-12 was observed only in patient no. 10, with a less than twofold increase in the anti-Env, anti-Gag, and anti-Nef CTL reactivities. These results indicate that IL-12 has little positive impact on the activation of CTL in the context of the current IVS scheme.
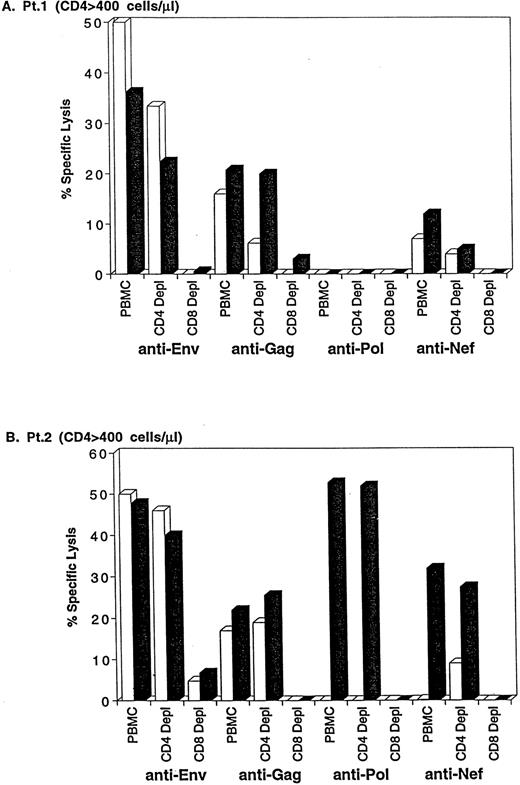
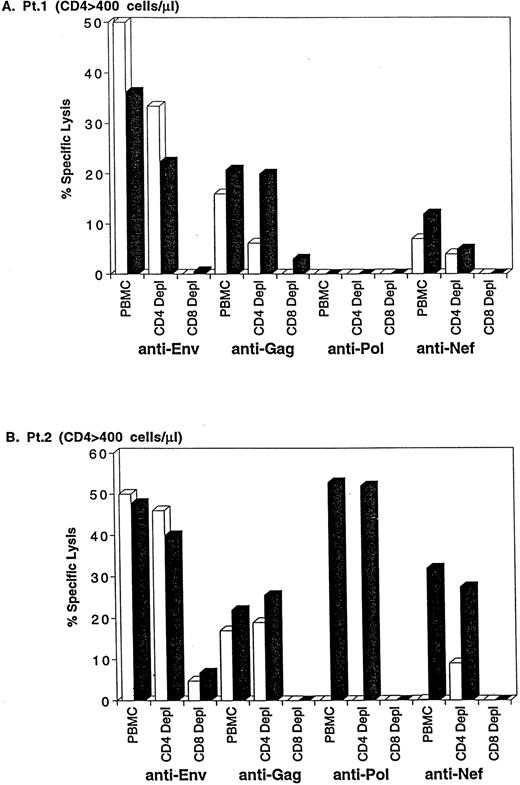
Specificity of CD8 CTLp activation by ALVAC constructs.By the nature of the HIV-1 genes inserted into their genomic DNA, the individual canarypox constructs should be capable of selectively activating CTLp in an antigen-specific manner. To investigate this property of the ALVAC vectors, PBMCs obtained from two different patients with CD4 counts greater than 400 cells/μL were stimulated in parallel with vCP205 and vCP300 constructs following the described procedures. The presence of anti-HIV CTL was tested at day 10 of IVS and the results are reported in Fig 2 as the percentage of specific lysis at an E:T = 10:1. In both patients, the vCP205 construct was able to induce both anti-Env and anti-Gag reactivities that were principally mediated by CD8+ lymphocytes. Stimulation with the vCP300 vector induced a broader spectrum of anti-HIV cytotoxic activities, including anti-Nef and anti-Pol CTL. It should be noted that a different pattern of CTL activities was evident in these two patients. In fact, patient no. 1 lacks demonstrable CD8+ anti-Pol CTLp, as evidenced by the failure of vCP300 to activate Pol CTL activities. Conversely, a full anti-HIV CTL complement against Env, Gag, Pol, and Nef antigens was detectable in PBMCs from patient no. 2.
Specific activation of anti-HIV CTL in patients no. 1 (A) and 2 (B) by vCP205 (Env and Gag) and vCP300 (Env, Gag, Pol, and Nef ) ALVAC vectors. Data are reported as the percentage of specific lysis at an E:T = 10:1, subtracting the background against vaccinia-infected autologous BLCL. CD4- or CD8-depleted effector populations were obtained according to the procedure described in the Materials and Methods. (□) vCP205; (▪) vCP300.
Specific activation of anti-HIV CTL in patients no. 1 (A) and 2 (B) by vCP205 (Env and Gag) and vCP300 (Env, Gag, Pol, and Nef ) ALVAC vectors. Data are reported as the percentage of specific lysis at an E:T = 10:1, subtracting the background against vaccinia-infected autologous BLCL. CD4- or CD8-depleted effector populations were obtained according to the procedure described in the Materials and Methods. (□) vCP205; (▪) vCP300.
CTL reactivity and cell phenotype after IVS.To compare the relative efficiency of polyclonal versus antigen-specific IVS, PBMC samples from 4 patients were studied. Fresh PBMCs were analyzed by flow cytometry and CD8 lymphocytes were isolated as described and subsequently stimulated with either soluble anti-CD3 MoAb or autologous PBMCs acutely infected with vCP300. At the conclusion of IVS (day 14), cell cultures were examined for relative functional CTL reactivity in the context of an LU20 formatted assay and phenotypic changes in the effector populations were assessed by flow cytometry. The results of these experiments are presented in Table 2. It should be noted that, for the functional data, the anti-vaccinia background CTL activity that was present after both types of stimulation has been subtracted from the LU20 values presented in Table 2, which thereby represent true HIV-specific CTL activities. With the possible exception of the anti-Env reactivities for patients no. 4 and 5, Ag-IVS appears far more efficient in activating CTL than polyclonal stimulation. Despite these striking differences in functional reactivities, phenotypic analyses failed to show major differences in the two effector populations. In fact, naive (ie, CD45RA+) and memory (ie, C45RO+) subsets of CD8+ cells increased similarly after both types of stimulation. However, the CD8+HLA-DR+ and CD8+CD38+ subsets were increased in parallel fashion in 3 of 4 patients after Ag-IVS, whereas the anti-CD3 stimulation lead to a preferential expansion of CD8+CD38+ cells.
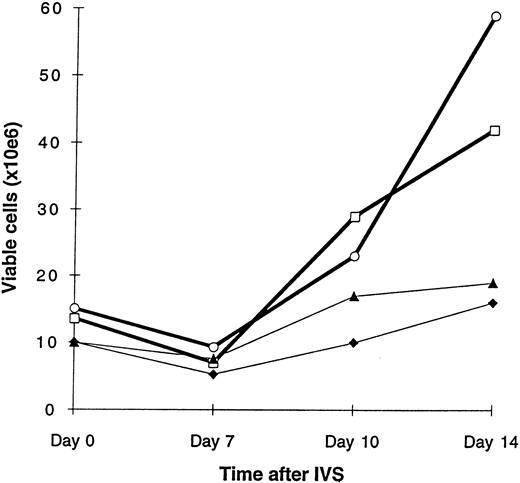
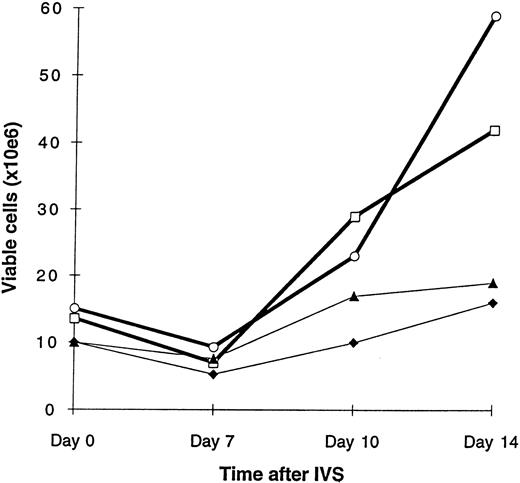
Activation/expansion of anti-HIV CTLp at different stages of disease.Once the specificity of CTL activation with the ALVAC constructs was determined, we focused our attention on the ability of these constructs to activate and expand CD8 CTLp in patients at different stages of disease. Four patients were selected for the study: patients no. 4 and 5 with CD4 counts greater than 400 cells/μL and patients no. 6 and 7 with CD4 less than 400 cells/μL. Because in previous clinical studies the expansion of purified CD8+ CTL was accomplished using a mitogenic stimulus,35 CD8+ lymphocytes obtained from these patients were stimulated in parallel with vCP300, PHA, or anti-CD3 MoAb. After 14 days of culture, the CTL frequencies were determined by a limiting dilution analysis (LDA) assay. As shown in Fig 3, the cell recovery at day 14 of IVS with vCP300 was higher in patients no. 4 and 5 (3- and 3.9-fold increase, respectively) compared with patients no. 6 and 7, in whom only a 1.9- and 1.6-fold increase, respectively, was observed. These data suggest that the efficiency of cell expansion in response to antigen stimulation was correlated with the CD4 count. CTL frequencies obtained after either mitogen or antigen stimulation are reported in Table 3. First, the anti-Env CTL frequencies in 3 of 4 patients were significantly higher in cultures stimulated with the vCP300, as indicated by the nonoverlapping 95% confidence intervals. Interestingly, in both patients with CD4 counts less than 400 cells/μL, the Ag-IVS strategy was the more efficient way to activate anti-Env CTL. Second, although different anti-Gag frequencies were obtained using the two stimulation strategies, the pattern of CTL reactivity elicited with the vCP300 stimulation was consistent with the pattern obtained after mitogen stimulation. Third, different levels of anti-Pol and anti-Nef reactivities were recovered among the 4 patients by the two stimulation strategies. Mitogen-stimulated cultures had higher anti-Pol and anti-Nef reactivities from patients no. 4 and 7, respectively. In contrast, the Ag-IVS was more effective in eliciting the anti-Pol and anti-Nef reactivities in PBMC cultures from patients no. 6 and 4, respectively.
Cell growth after in Ag-IVS. The results are reported as total viable lymphocytes. Cell viability was determined by erythrosin B exclusion. (□) Patient no. 4 (CD4 <400); (○) patient no. 5 (CD4 <400); (▴) patient no. 6 (CD4 <400); (♦) patient no. 7 (CD4 <400).
Cell growth after in Ag-IVS. The results are reported as total viable lymphocytes. Cell viability was determined by erythrosin B exclusion. (□) Patient no. 4 (CD4 <400); (○) patient no. 5 (CD4 <400); (▴) patient no. 6 (CD4 <400); (♦) patient no. 7 (CD4 <400).
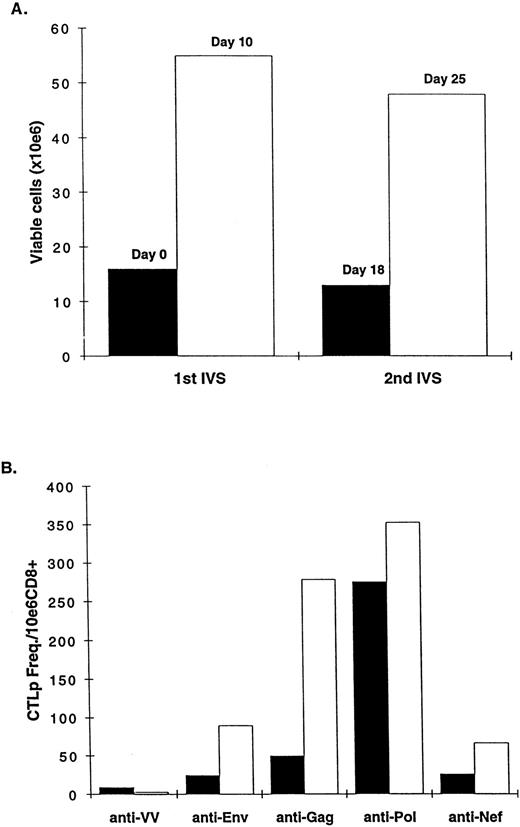
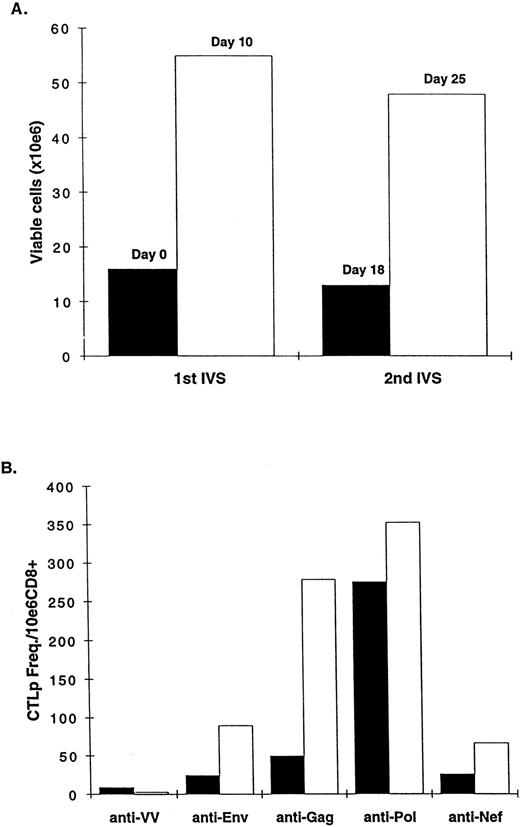
Expansion of anti–HIV-1 CTL with two rounds of Ag-IVS.Canarypox-based constructs were further studied for their capacity to selectively support the expansion of anti-HIV CD8 CTL after two rounds of IVS. CD8+ T lymphocytes were obtained from patient no. 2 and stimulated on day 0 with vCP300-infected autologous PBMCs. The cells were expanded until day 18, when a portion of the cells was restimulated using the same procedures. The CTL frequency was determined by LDA assay on day 10 and day 25 and the results are reported in Fig 4. As shown in Fig 4A, a 3.4- and a 3.6-fold range of cell expansions was obtained after the first and second IVS, respectively. The most pronounced effect on the CTL frequency was observed in the expansion of Gag-specific CTL. As shown in Fig 4B, the anti-Gag CTL frequency increased from 50 to 279 CTLp/106 cells (5.5-fold increase). Among the different antigen-specific CTL reactivities, an overall average of 3.2- ± 1.8-fold increase was achieved with the second stimulation. It should also be noted that a very low background against the vaccinia target control was elicited by this procedure. In no instance were CTL frequencies decreased after a second round of IVS.
(A) Cell expansion after two rounds of Ag-IVS of CD8+ lymphocytes from patient no. 2. (B) CTL frequencies were calculated by LDA after the first and second IVS with vCP300 (days 10 and 25, respectively) and reported as CTLp frequency per 1 × 106 lymphocytes. (▪) After first IVS; (□) after second IVS.
(A) Cell expansion after two rounds of Ag-IVS of CD8+ lymphocytes from patient no. 2. (B) CTL frequencies were calculated by LDA after the first and second IVS with vCP300 (days 10 and 25, respectively) and reported as CTLp frequency per 1 × 106 lymphocytes. (▪) After first IVS; (□) after second IVS.
DISCUSSION
In the present study, we show the highly efficient, antigen-specific activation and expansion of anti–HIV-1 CTLp from infected patients via stimulation with transient expression canarypox/HIV vector constructs. Moreover, this maturation of CTLp into functionally mature CTL is highly dependent on the relative disease status (ie, CD4 count) of the patient. Previous studies have examined ex vivo expansion of anti-HIV CD8+ CTL from HIV-infected individuals, but all of these involved polyclonal activators. Ho et al41 reported that CD8+ lymphocytes expanded using mitogenic stimulation retained their ability to recognize several HIV antigens. However, polyclonal stimuli may activate lymphocytes with unknown and possibly detrimental functions, a risk that can be reduced or eliminated by antigen-specific IVS. Moreover, antigenic stimulation as described in this study uses cells expressing costimulatory molecules as antigen-presenting cells (ie, monocytes/macrophages) and thereby is able to recruit naive as well as antigen-primed memory and effector cells, whereas mitogenic stimulation, lacking costimulatory stimuli, has a restricted effect on antigen-experienced cells.42 Stimulation induced through TcR-linked signals alone (ie, anti-CD3) can also induce apoptosis of activated cells, reducing the pool of cells that can be expanded in vitro.43 This could, in part, account for the decreased recovery of anti-HIV CTL reactivities after the stimulation with soluble anti-CD3, as shown in Table 2. Unlike anti-CD3 activation, IL-7 is essential to our antigen-specific IVS strategy. We do not know, at present, whether IL-7 could also augment the antibody-based polyclonal expansion of CTLp from a population of highly enriched CD8+ lymphocytes. Stimulation with the vCP205 construct did not induce cross activation of anti-Pol– or anti-Nef–specific CD8+ CTL, otherwise activated by the vCP300 construct, suggesting that activation of CTLp is not induced by secondary activation of endogenous virus.
When Ag-IVS was used in parallel to a mitogenic stimulation for the activation and short-term expansion (14 days) of CD8 cells, three important results were obtained. First, it was evident that, under these culture conditions, CD8 CTL obtained from asymptomatic individuals were successfully activated and underwent a threefold to fourfold expansion. Conversely, CD8 lymphocytes obtained from individuals with CD4 counts less than 400 cells/μL proliferated poorly despite CTL activation. Secondly, Ag-IVS was able to induce significantly higher anti-Env CTL frequencies in 3 of 4 patients. Lastly, a comparable pattern of anti-Gag reactivity was elicited by antigen-specific and mitogenic stimulation, whereas anti-Pol and anti-Nef reactivities after Ag-IVS were significantly lower in 2 of the 4 patients. The apparent discordance in the activation of anti-Pol and anti-Nef CTL by Ag-IVS may be the results of the limited numbers of Pol and Nef CTL epitopes expressed by the canarypox constructs. The Pol and Nef epitopes recognized by patients no. 4 and 7, respectively, might be different from the previously reported epitopes inserted in the vCP300 vector.
Taken together, these results suggest that ex vivo expansion therapy after antigen-specific activation may only be feasible in the early stages of the infection when the proliferative capability of the CD8+ lymphocytes is not compromised.10,11 44 In such patients, it should be possible to increase the pool of cells that are acting as a first line of defense against virus spread. However, it is interesting to note that, despite a diminished expansion in the patients with CD4 counts less than 400 cells/μL, we were still able to show CTL activation. Curiously, in these patients, the anti-vaccinia CTL frequencies were higher than in the earlier stage patients.
More recently, Lieberman et al45 reported a procedure of polyclonal activation and subsequent peptide restimulation that was based on the epitope repertoire recognized by individual patients in the context of their MHC class I expression. Two rounds of peptide stimulation allowed the establishment of T-cell lines against specific HIV epitopes. The complex work of characterizing individual immunodominant epitopes is readily overcome with canarypox vectors that express the full complement of HIV epitopes presented by different MHC class I alleles.
Koenig et al46 derived a cytotoxic T-lymphocyte clone directed against the HIV-1 Nef protein after polyclonal activation and expansion. The infusion of this clone induced an in vivo selection of HIV isolates lacking the Nef epitope, strongly suggestive of an immunoselective pressure. In our experience, the ALVAC vectors used in this study do not selectively expand one type of antigen-specific CTL, but, as indicated in Table 2, the full repertoire present in the patient. Therefore, the reinfusion of these cells with a broad repertoire is unlikely to represent an immune pressure capable of selecting CTL resistant viral variants.
It is also encouraging that a first round of in vitro stimulation can be successfully followed by a second with a further expansion of the CTL cells as presented in Fig 4. It is important to note that in no instances were CTL frequencies diminished after a second round of IVS.
The analysis of the CD8 subtypes showed a similar increase in the percentage of memory and naive cells in both mitogen and antigen-specific stimulated cultures compared with the fresh PBMCs. However, the expression of activation markers such as CD38 was lower in the antigen-stimulated cells compared with the mitogen-stimulated cells, suggesting that antigen stimulation could be acting on a fraction of the total cells. Furthermore, if we consider the expression of activation markers in circulating PBMCs, mitogenic stimulation supported a preferential expansion of CD8+HLA-DR+ cells, whereas a comparable percentage of CD8+ cells were expressing both CD38 and HLA-DR markers only after Ag-IVS. Once again, these data suggest that antigen-specific stimulation is more effective in expanding the CTL population, according to a previous study by Ho et al,47 which showed that anti-HIV CTL activity is mainly mediated by the CD8+CD38+HLA-DR+ lymphocytes. The only concern in this IVS scheme was the increase in CD3−CD16−56+ cells, defining the NK population, in patients no. 4 and 10. However, NK cell expansion did not play a role in the increased CTLp frequency, because different levels of frequencies were noted among the antigen-specific CTL populations. CD3−CD16−56+ cells have been described as the effector cells in the antibody dependent cell-mediated cytotoxicity (ADCC), a mechanism by which infected cells can be cleared from the system in an MHC-unrestricted fashion.48
Different cytokines can play a relevant role in the maturation and growth of antiviral and antitumor CTL lymphocytes.17,34,35,49-51 The data obtained in our study suggest that IL-7 and IL-2 can effectively support the activation/expansion of anti-HIV CTL. In contrast to previous studies by Mehrotra et al35 with human anti-influenza CTL, we did not observe either significantly increased cell recoveries or CTL activity when optimal concentrations of IL-12 were used. Our observations concerning the addition of IL-4 to the cultures is in partial agreement with previous results reported by Horohov et al.34 In fact, IL-4 inhibited the activation/growth of anti-HIV CTL when added on day 0 (data not shown), as previously described, but it failed to significantly affect the CTL reactivities when added on day 5. Collectively these data suggest that neither exogenous IL-4 nor IL-12 plays a critical role in this scheme of antigen activation. Human recombinant IL-12 might be required only during the early phases of CD8 differentiation into mature CTL,52 and its presence may be not essential for the Ag-restimulation of memory cells. Previous studies have shown that IL-4 can actually inhibit the activation/maturation of CD8+ CTL,53 thus providing an additional rationale for excluding this cytokine from our IVS scheme.
Several investigators have reported that CD8+ T lymphocytes are capable of controlling virus spread not only by cytolytic mechanisms, but also by releasing soluble factors able to inhibit either HIV-1 transcription54-57 or virus entry.58-61 In preliminary experiments we have begun to compare the ability of mitogen- and antigen-stimulated CD8+ T lymphocytes to suppress virus replication, and the results thus far suggest that suppressive activity was comparable in both conditions (G. Ferrari and J. Toso, unpublished observation). Therefore, it is noteworthy that our IVS strategy is able to activate both of the anti-HIV activities mediated by CD8+ cells that have been so far characterized. This could be a reflection of expanded CTL populations that are capable of mediating cytolytic events as well as noncytolytic virus suppression as described by Toso et al62 and most recently by Yang et al63 using clonal CTL populations.
Studies conducted in our laboratories as part of the evaluation of HIV candidate vaccines suggest that the antigen-specific in vitro stimulation described in this report is able to recruit only CTL precursors. In fact, de novo CTL induction in lymphocytes from preimmunization baselines and placebo-treated volunteers enrolled in the HIV vaccine protocols is an extremely rare event (ie, <3%) using this IVS procedure (data not shown). According to these observations in seronegative volunteers, it appears unlikely that this in vitro stimulation can induce the recognition of new CTL epitopes different than those expressed by resident virus(es) in infected patients.
Overall Ag-IVS stimulation with ALVAC constructs described in the present studies can specifically activate and expand a wide repertoire of anti-HIV CTL. Because canarypox viral vectors retain pancytotropic properties, but do not productively replicate in mammalian host cells as the vaccinia vectors, safety concerns are eliminated for immunotherapeutic applications. Canarypox vectors activate anti–HIV-1 CTLp in a manner similar to recombinant vaccinia constructs, except that ALVAC stimulation is highly dependent on the presence of exogenous IL-2 (G. Ferrari, unpublished observation). Obviously, vector replication is not a requirement for CTLp activation. Although canarypox vectors are potent stimulators of antigen-specific CTL, they are poor targeting vectors when used in the context of acute infection of BLCL targets used for CTL assays (K. Weinhold, unpublished observation). Targeting may be more dependent on overexpression of extrinsic gene products than is CTLp activation.
The present studies are germane to the future therapeutic use of canarypox constructs either as a direct in vivo stimulus (ie, active immunization) or as a modality for ex vivo activation and expansion of CTL for use in adoptive immunotherapeutic approaches. In the current climate of combination antiretroviral therapies capable of greatly reducing plasma viremia,64 65 consideration of active or adoptive CTL-based therapies remains appropriate in light of the uncertainties of the impact of drug therapy on the proviral load established in long-lived cellular reservoirs. Unlike plasma virus, these are the true targets for CTL therapy, and long-term control of viral load will depend on significant reduction in these important viral sanctuaries.
ACKNOWLEDGMENT
The authors thank Barlett Humphries and the clinical staff of the Duke Adult Infectious Disease Clinic as well as the patients involved in these studies for their generous participation.
Supported by Grants No. 5-RO1-AI29852 and 5-P30-AI28662 from the National Institute of Allergy and Infectious Disease.
Address reprint requests to Kent J. Weinhold, PhD, PO Box 2926, Duke University Medical Center, Durham, NC 27710-2996.