Introduction:
Richter transformation (RT) refers to the progression of an aggressive lymphoma arising on the background of chronic lymphocytic leukemia/small cell lymphoma (CLL/SLL). Despite the incidence of RT among CLL/SLL is low (range 2-10%), the prognosis is very poor. Usually, different clinical and biology characteristics were observed between CLL/SLL and RT stages, and their impacts on disease progression remains unknown. In this report, we investigated the clinical characteristics and outcomes of 37 Chinese patients (pts) in CLL/SLL and in RT stages. This 18-year follow-up retrospective study might serve as a basis for future prospective clinical studies.
Methods:
From Feb 2004 to Feb 2022, all of the CLL/SLL pts who developed biopsy-proven RT in our institution were enrolled. Clinical characteristics and survival data (treatment course, clinical response to treatment as determined by treating physician, and survival information) were collected by chart review. Overall survival 1 (OS 1) was defined as the time from initial CLL/SLL diagnosis to death. Overall survival 2 (OS 2) was defined as the time from RT to death.
Results:
A total of 37 Chinese pts with pathological proven RT were enrolled from Feb 2004 to Feb 2022. The median age at CLL/SLL diagnosis and at RT were 60 years (range 29-63 years) and 63 years (range 35-77 years), respectively. Twenty-four pts (64.9%) were male. Frequencies of several adverse clinical/laboratory factors were significantly higher at RT diagnosis compared to at CLL/SLL diagnosis, including elderly age (40.5% vs. 16.2%, p=0.020), bulky disease (45.9% vs. 18.9%, p=0.017), extranodal disease (37.8% vs. 5.4%, p=0.001), B symptoms (67.6% vs. 27.0%, p<0.001) and hypogammaglobulinemia (70.3% vs. 51.4%, p=0.026). The rate of advanced Rai staging was higher in RT stage than in CLL/SLL stage. However, no statistically significant difference was observed in Binet staging or CLL-international prognostic index (CLL-IPI).
In CLL/SLL stage, 27 pts (27/37, 73.0%) received at least one line of therapy. The median number of treatment lines was 1 (range: 0-4). Ten pts (27.0%) received BTK inhibitor and 4 pts (10.8%) treated with Bcl-2 inhibitor treatment, 11 pts (29.7%) received purine analogue therapy (i.e. fludarabine) and 9 pts (24.3%) were exposed to anti-CD20 antibody.
In our study, the median time from CLL/SLL diagnosis to RT was 45.3 months (95% CI 36.0-54.6 months). In RT stage, the median number of treatment lines was 2 (range: 0-6). Twenty-four pts (64.9%) received BTK inhibitors, 4 pts (10.8%) received Bcl-2 inhibitor treatment, 6 pts (16.2%) received anti-PD1 treatment as part of salvage therapy and 2 pts (5.1%) underwent chimeric antigen receptor T (CAR-T) therapy.The best overall response (BOR) data post RT was collected in our study. Among 36 pts who ever received any anti-cancer treatment and had at least one disease assessment, 1 pt (2.8%) achieved complete response (CR), 19 pts(52.8%) achieved partial response (PR), the rest pts resulted in stable disease (SD) (8/36, 22.2%) and progressive disease (PD)(8/36, 22.2%).
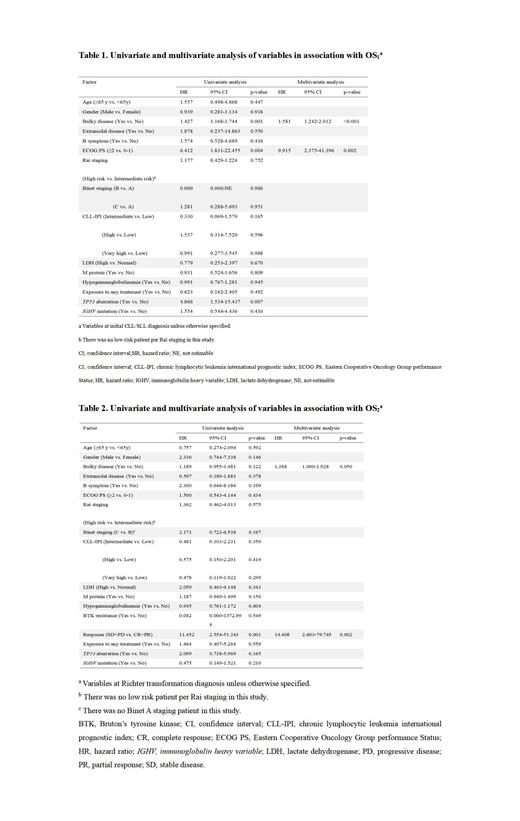
The median OS 1 was 119.7 months (95% CI 77.78-161.6 months). Clinically significant difference of OS 1 was observed between salvage therapy responders (CR+PR) compared to non-responders (SD+PD). The estimated median OS 1 was not reached (NR) for responders and 78.8 months (95% CI 30.1-127.5, p=0.001) for non-responders. For OS 1, in the univariate analysis, bulky disease, Eastern Cooperative Oncology Group (ECOG) and TP53 aberration are identified as three prognostic factors. In the multivariate analysis, bulky disease and ECOG were confirmed as independent prognostic factors.(Table 1)
The median OS 2 was 39.6 months (95% CI 3.4-75.8 months). Patients who responded to salvage therapy had significantly better OS 2 than non-responders. The median OS 2 was NR vs. 8.3 months (95% CI 0-25.2, p<0.001). For OS 2, in both the univariate analysis and multivariate analysis, bulky disease and treatment response were identified as two prognostic factors in RT stage.(Table 2)
Conclusion:
In this long-term follow-up study, pts presented more aggressive clinical/laboratory characteristics in RT stage than in CLL/SLL stage. The outcome of Chinese pts with RT was very poor. For OS 1, bulky disease and ECOG are identified as prognostic factors. While, bulky disease and treatment response were confirmed as the indepedent prognostic factors in RT stage.
Disclosures
No relevant conflicts of interest to declare.