Introduction
Increasing outpatient care in all medical departments will pose a challenge for daily routines and force us to rethink established processes. In hemato-oncology there is good evidence for the continuous improvement of overall survival after allogeneic stem cell transplantation (allo-HCT) during the last decades. However, the chronic character of the underlying hematopoietic malignancy and the accompanying long-lasting consequences of an allo-HCT are often not properly addressed in follow-up care. The health care status of this population should be determined on physical and mental condition and serious longer-term sequelae need to be monitored more closely than on quarterly basis. Patient-reported outcome measurements (PROMs) are able to address this issue in clinical routine and capture the multidimensional construct of quality of life (QoL). PROMs focus mainly on how a patient survives after a treatment, and not only on whether she/he survives and how long.
Patients and Methods
We performed a cross-sectional survey including all adult allo-HCT recipients who attended follow-up care in the period from March to July 2023 at the University Hospital Tübingen, Germany. Eligible participants completed both, the EORTC Core Quality of Life questionnaire (EORTC QLQ-C30) and the Functional Assessment of Cancer Therapy General (FACT-G) with the subscale for Bone Marrow Transplantation (FACT-BMT). We built 8 cohorts (day 30, day 100, month 6, month 12, year 3, year 5, year 10 and >10 years) to evaluate QoL after allo-HCT and to identify predictors like age, performance status (PS), conditioning regime, graft-versus-host disease (GvHD) development and relapse.
Results
We included 200 recipients (93 women, average age 54.2 years) who received allo-HCT between 2004 and 2022. The majority was treated for acute leukemia (n=95), followed by chronic leukemia (n=16), myelofibrosis (n=25), myelodysplastic neoplasm (n=20), lymphoma/myeloma (n=14) and others (n=30). 82.5% (n=165) received reduced-intensity conditioning (RIC) and 17.5% (n=35) myeloablative conditioning (MAC). 75.5% (n=151) of allogeneic donors were HLA-matched, 14.5% (n=29) HLA-mismatched and 8.5% (n=17) haplo-identical. The median follow-up was 43.4 months with the following patient numbers in the 8 cohorts: n=25 (d30), n=21 (d100), n=24 (m6), n=34 (m12), n=32 (y3), n=30 (y5), n=23 (y10) and n=11 (>10y). 73% (n=146) showed complete remission at last follow up, 14% (n=28) relapsed. Acute GvHD was observed in 39% (n=78) with additional 6.5% (n=13) suspected to have one. Chronic GvHD was observed in 39.5% (n=79).
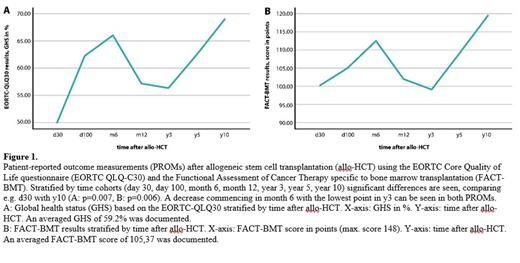
Average GHS in the EORTC QLQ-30 was 59.2%, average total scores in the FACT-G and FACT-BMT were 77.68 (max. score 108) and 105.37 (max. score 148), respectively. Both PROMs (EORTC QLQ30, FACTs) demonstrated the same biphasic course with a significant QoL recovery over time (Figure 1), comparing for example the global health status (GHS) on d30 (50%) with y10 (68,8%, p=0.07). Interestingly, allo-HCT recipients again experience a drastic decrease achieving y3, mainly caused by worse emotional and physical well-being. The median ECOG PS before allo-HCT was 0 and degraded to 1 in all cohorts until y10, where a return to baseline was seen. Current PS and PRO results showed a significant correlation (p<0.001). No correlations between QoL and age, GvHD or conditioning regime were found.
Conclusion
Allo-HCT recipients manage to regain a good QoL in long-term follow-up over 10 years but experience a significant low around y3. PROMs are able to detect such developments and can help to improve patient management. As indicated by our data, a higher degree of support in y3 could improve QoL and well-being of allo-HCT patients. However, until today, we lack the implementation of efficient strategies to do so in clinical routine.
Disclosures
No relevant conflicts of interest to declare.